Document
Female Reproductive System: Functions
Role of male is to produce and deliver sperm. Role of female is
1. Generate and release fertile ova
2. Maintain fertilized ova throughout development
3. Deliver newborn
4. Nourish newborn
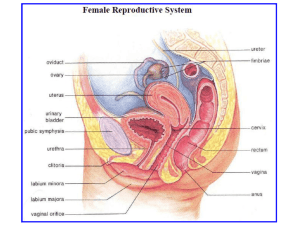
Basic Anatomy
Ovarian Cycle
Beginning at puberty and continuing until menopause, ovaries cycle between two endocrine states every 28 days or so unless interrupted by pregnancy.
1. Primary follicles in ovary = primary oocyte in layer of granulosa cells.
2. Granulosa cells proliferate
-> fluid-filled follicle with oocyte in granulosa cells
3. Follicular cells secrete estrogens
(mainly estradiol) into circulation and follicular fluid
Ovarian Cycle (continued)
4. One follicle (usually) grows faster than others, becoming a mature Graafian follicle.
5. At about 14 days into the cycle, it ruptures. This releases oocyte and estrogen-rich fluid into body cavity at entrance to oviducts.
6. This is ovulation; it ends the follicular phase.
Ovarian Cycle (continued)
7. End of follicular phase = beginning of luteal phase.
8. Follicular cells that remain on ovarian surface accumulate precursors of steroids, which makes them yellow. They’re now called the corpus luteum (= yellow body)
Ovarian Cycle (continued)
9. Corpus luteum secretes two steroid hormones: lots of progesterone, not so much estradiol.
10. If the ovum isn’t implanted in the uterus, this phase lasts about
14 days, corpus luteum degenerates and a new follicular phase begins.
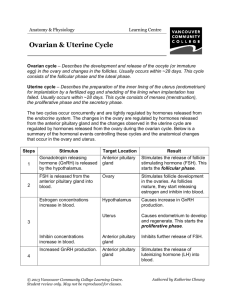
Control of Ovarian Cycle
Hypothalamus releases pulses of GnRH, stimulates LH and FSH
1. Ovulation is triggered by surge in plasma LH levels.
2. LH maintains corpus luteum for about 14 days.
Uterine (Menstrual) Cycle Results from Effects on Uterus
To simplify, pretend that uterus consists only of myometrium
(muscle) and endometrium (lining). Estrogens stimulate growth of both, induces progesterone receptor formation in endometrium
(follicular phase of ovarian cycle).
Endometrium accumulates electrolytes and water, becomes more vascular, stores lots of glycogen. Progesterone inhibits myometrial contractions during luteal phase.
Uterine cycle = proliferative phase (starts around day 7 of ovarian follicular phase) + menstrual phase (starts around day 28 of ovarian cycle; during luteal phase).
Day 1 of uterine cycle is defined as first day of menstrual flow.
This happens when corpus luteum degeneration sharply reduces plasma estrogen and progesterone levels.
Endometrium secretes prostaglandins, which constrict endometrial vessels. Causes degeneration of endometrium and stimulates myometrial contractions. Menstrual flow is the expulsion of dead endometrium. Typical volume = about 100 ml.
After 5 to 7 days, follicular secretion of estrogens ends menstrual flow and initiates proliferative phase. This ends at ovulation.
Fertilization and Pregnancy
Sperm are deposited in the distal part of the vagina, migrate through the cervix, uterus, into the oviducts. Fertilization usually occurs in the distal part of the oviduct, occasionally occurs outside the oviduct.
Notice how far the sperm travel, and how little must go wrong for fertilization to happen outside the oviduct. A fertilized egg that implants outside the uterus is an ectopic pregnancy.
The fertilized ovum is propelled through the oviducts into the uterus, and if it implants in the uterine wall, a pregnancy begins.
Note how many things can prevent a pregnancy from occurring.
When a fertilized egg implants, it induces formation of placenta, which supports the embryo/fetus until the end of pregnancy.
Placenta
1. Maternal and fetal blood supplies pass close enough to exchange materials through capillaries. This provides fetus with nutrients and oxygen and a route for excretion of wastes.
2. Produces chorionic gonadotropin, which maintains pregnancy conditions in uterus (maintains corpus luteum, thus preventing endometrial degeneration).
3. HCG has been the basis of pregnancy tests for about 100 years.
4. Produces estrogens and progesterone during third trimester.
5. After delivery of newborn, placenta detaches and is expelled
(“afterbirth”)
Milk Production
High circulating levels of estrogens during pregnancy stimulates prolactin secretion.
Prolactin plus placenta’s secretion of chorionic gonadotropin stimulate mammary glands.
After delivery of newborn, prolactin stimulates milk production, oxytocin stimulates milk expulsion.
Suckling initiates reflexes that cause hypothalamus to secrete PRH, which promotes prolactin secretion and maintains milk production.
Also stimulates reflexive release of oxytocin from posterior lobe.
All of this can be conditioned to stimuli other than suckling and can be inhibited by various kinds of stress.