Morphology-Bioch-Libya-6-13-2007-Presentation1
advertisement

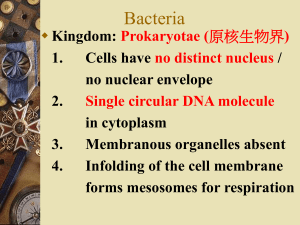
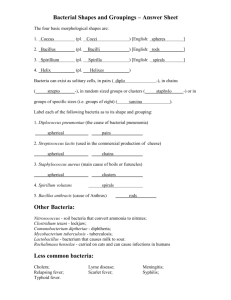
Specimen Collection and Transport The most important aspects of microbiological testing are collection of the right specimen and transport of the specimen to lab in a manner that insure the reliability of the diagnostic procedure (e.g., culture, microscopy and antigen or antibody tests). As a general guideline for all specimens the following consideration should be kept in mind: Specimens should always be considered infectious. Therefore, gloves should always be worn when handling specimens. Specimens should be collected from the areas where organisms are present. For example, diagnosis of a lower respiratory tract infection requires collection of material from that site (e.g., sputum) and not from the mouth (e.g., saliva) The quantity of specimen collected must be sufficient to ensure that all requested tests (culture, microscopy, antigen tests ,nucleic acid probes and amplification) can be performed properly. Transport of specimens should maintain the viability of etiologic agent (if culture is performed) and prevent overgrowth with contaminating organisms. Specimens should always be transported in a leak-proof container inserted in a leakproof plastic bag. for shipement of speciemen or isolates, refer to the International Air Transport Association (IATA) Dangerous Goods Regulation (http://www.IATA.org/dangerousgoods/index), the U.S. Department of Transportation (http://hazmat.dot.gov/rules.htm) and the international Civil Aviation Organization (ICAO). Each specimen type requires specific packing and handling procedures. The Classification and Identification of Bacteria of Medical Importance Gram negative cell wall Gram positive cell wall Gram stain One of the most important techniques in bacteriology is the Gram stain, first described by Hans-Christian Gram in 1884. It allows the differentiation of bacteria into two groups: Grampositive bacteria can retain a complex made between crystalviolet and iodine when decolourised with acetone, whereas Gram-negative bacteria are decolourised on treatment with acetone. the Gram stain enables the shape of bacterial cells to be observed easily. Bacteria fall into two major classes: rod shaped bacteria are known as 'bacilli' (singular: 'bacillus') and round or roundish bacteria are known as 'cocci' (singular: 'coccus'). This property reveals fundamental differences in the cell envelope between the two groups. Gram-positive bacteria have many layers of peptidoglycan in their cell wall; Gram-negative bacteria have only one or two peptidoglycan layers but, additionally, they have an outer membrane. These differences have important consequences. For example, certain antibiotics cannot penetrate the outer membrane of Gram-negative bacteria, which are intrinsically resistant to these drugs as a consequence. Micrococcus luteus Staphylococcus aureus Bacillus subtilis E. coli Serratia marcescens Performance standards for stains Control organism/ material ATCC No Expected result Ziehl-Neelsen Mycobacterium sp. Esch. coli 25177 25922 Pink red bacilli Blue bacilli Acridine orange Esch. coli Staph.aurues 25922 25923 Fluorescent bacilli/cocci Giemsa Thin film blood smear Gram Esch. coli Staph.aureus Iodine solution Formalin treated stool specimen with cysts Visible cyst nuclei Spores Bacillus species Spores stain one colour and bacillus stains with counterstain Stain Distinct staining of WBCs and RBCs 25922 25923 Gram -ve bacilli Gram +ve cocci Quality control of stains need to be performed on weekly basis and also as and when a new lot of reagents for staining are procured Staphylococcus aureus, and shows Gram-positive cocci in grapelike clusters. There are two major groups of Gram-positive cocci that are of medical importance: the staphylococci and the streptococci . When viewed microscopically, staphylococci appear in clumps, like bunches of grapes. Staphule is Greek for grapes. Streptococci form chains, and are named after streptos, the Greek word for twisted. These groups of bacteria can be distinguished because staphylococci produce an enzyme, catalase and streptococci do not. Catalase causes the conversion of hydrogen peroxide to water with the concomitant release of oxygen gas, seen as bubbles in the reaction tube. The catalase test is a more reliable test to differentiate staphylococci from streptococci than microscopic observation. Streptococcus pyogenes and shows Gram-positive cocci again, this time in chains. Streptococci are classified according to their ability to break down blood in fresh blood agar plates. Some streptococci have no effect on blood. These are the non-haemolytic streptococci (see below). The α-haemolytic streptococci cause partial breakdown of blood, and their colonies are surrounded by a greenish halo. The green pigment is thought to comprise the metabolic degradation products of haem. Because of the colour of halo that surrounds ahaemolytic streptococci, they are often referred to as "viridans" streptococci (viridis is Latin for green). There is one α -haemolytic streptococcus that must be differentiated from the others. This is Streptococcus pneumoniae. This is the cause of pneumococcal pneumonia and meningitis, as well as less serious infections. Streptococcus pneumoniae is sensitive to optochin, an antimicrobial agent. All other viridans streptococci are resistant to optochin . Streptococcus Gram stain Greening Streptococcus In Blood Agar The ß-haemolytic streptococci cause the complete breakdown of blood in fresh blood agar plates. The colonies are surrounded by haloes that are completely clear. Clinically, the most important of the b-haemolytic streptococci is Streptococcus pyogenes. This belongs to the "Lancefield Group A" based upon its antigenic structure. Streptococcus pyogenes may be differentiated from other b-haemolytic streptococci on the basis of its sensitivity to the antibiotic bacitracin. The most important of the non-haemolytic streptococci are the enterococci such as Enterococcus faecalis and Enterococcus faecium. Until the early 1990's these bacteria were classified in the genus Streptococcus but molecular biological techniques have shown that they are sufficiently distant from other streptococci to warrant being placed in their own genus. As their names imply, these bacteria can be found in the gut, and can grow in the presence of bile salts. • Beta-Hemolytic Streptoccus; group of bacteria, most common of which is Streptococcus pyogenes, which may cause Strep Throat, Scarlet Fever, Glomerulonephritis, or Rheumatic Fever. Hemolysis on blood agar. LM Gram-positive Bacilli The genus Bacillus The Gram-positive rods can be divided according to their ability or otherwise to produce spores. Spores of Gram-positive rods are highly resistant structures that may add considerably to their pathogenic capacity. Sporing Gram-positive rods that are confined to the (somewhat confusingly named) genus Bacillus. Important members of this genus include Bacillus anthracis the cause of anthrax, and Bacillus cereus a cause of food poisoning. (Ceres was a Roman goddess of the harvest). The genus Bacillus also has members that produce clinically useful antibiotics, like Bacillus polymyxa, the source of polymyxin. The image on the left is of Clostridium perfringens, stained from a clinical specimen using the Gram staining protocol. Spores can be seen as areas with no stain in a few of the dark fat rods of this bacterium. In culture, it is very difficult to persuade this bacterium to form spores but they are seen in clinical specimens. The spores are located towards the centre of the bacillus in this species and they do not cause the bacilliary body to swell. In contrast, the spores of Clostridium tetani are located at the end of the cell and are wider than the bacilliary body. Sporing bacteria of Clostridium tetani have a characteristic 'drumstick' appearance, as seen in the image on the right. This is a spore stain made from a pure culture of these bacteria. Clostridium tetani Bacteria are gram-postive rods or bacilli with terminal spores that cause tetanus in humans, spore Bacillus of Anthracis (Gram Stain) Other Gram-positive bacilli The motility of the non-sporing Gram-positive rods is an important attribute in distinguishing coryneform bacteria and lactobacilli from listeria. Listeria monocytogenes is an important human pathogen, and it is capable of a characteristic tumbling motility seen at 25 degrees C but not at 37 degrees C. Lactobacilli appear microscopically as long, slender rods that often grow in chains. They may appear "Gram-variable" with some parts of the cell appearing blue-black and other portions looking red. They tend to make their immediate environment too acid for other bacteria to tolerate. Some lactobacilli are important members of the vaginal commensal flora of women of child-bearing age. These are sometimes referred to as Döderlein bacilli. The lactobacilli are catalase-negative, and can thus be distinguished from the coryneform bacteria that do produce catalase. The most infamous of the coryneform bacteria is Corynebacterium diphtheriae , toxigenic strains of which cause diphtheria. This gives the coryneform bacteria their alternative name - diphtheroids. They appear somewhat irregular in shape, and tend to cluster in Gram films. Some microbiologists think that this gives them the microscopic appearance of Chinese letters. Propionibacteria are coryneforms that cannot grow in the presence of air. A notable example is Propionibacterium acnes, associated with acne. Gram stain of a Corynebacterium seen on a skin swab Gram stain of Corynebacterium spp. demonstrating "Chinese letters" formations Small, nonmotile, irregularly staining pleomorphic Gram-positive rods with club-shaped swelled ends but no spores; may be straight or slightly curved C. diphtheriae and related organisms are collectively termed coryneforms or diphtheroids Corynebacteria possess capsular (K) and somatic antigens (O) The top image is of a group of corynebacteria stained using Gram's method and clustered in their characteristic shape. Some bacteriologists consider these to resemble Chinese pictograms. An idealsied version is shown in the lower image Pasteurella (Francisella) tularensis) Bacteria, the gram-negative coccobacillus pathogen that causes Tularemia or Rabbit Fever. LM X500. Description: Gram Stain Smears of the Agents of Anthrax (Bacillus anthracis), Plague (Yersinia pestis), and Tularemia (Francisella tularensis), Demonstrating Comparative Morphology, Size, and Staining Characteristics (Dennis et al., 2001). Tularemia, also known as rabbit fever or deer-fly fever, is a zoonotic disease caused by the gram-negative intracellular pathogen Francisella tularensis (Farlow et al., 2005 Francisella tularensis Growth at 72 Hours After Inoculation These Francisella tularensis colonies show characteristic opalescence on cysteine heart agar with sheep blood (cultured at 37 C for 72 hours). Note: On cysteine heart agar, F tularensis colonies are characteristically opalescent and do not discolor the medium (Dennis et al., 2001). • F. tularensis grows best in cysteine-enriched broth and thioglycollate broth. It grows best on cysteine heart blood agar, sheep blood agar, and on cysteine-supplemented agar such as buffered charcoal-yeast agar, Thayer-Martin agar, and chocolate agar. Selective agar may be useful when culturing materials from nonsterile sites, such as sputum. Optimal Temperature: 37 C , (Dennis et al., 2001). Mycobacteria The mycobacteria are a group of bacteria that are classified with other Gram-positive bacteria on the basis of their cellular architecture, but they possess a very waxy cell wall, and they rarely stain using conventional protocols such as the Gram stain. They require special staining techniques in order to be observed easily under the microscope. In the Ziehl Neelsen technique, a strong solution of carbol fuchsin is applied to the microscope slide which is then heated and held near boiling point for at least five minutes. This is to allow the stain to penetrate the mycobacterial cells. Following this treatment the stain will remain in the cell, even when the slide is treated with a mixture of inorganic acid and alcohol. To visualise any other material on the slide, methylene blue is applied as a counterstain. Because mycobacteria resist decolourisation with acids and alcohol they are sometimes called acid alcohol-fast bacilli. Important examples include Mycobacterium tuberculosis and Mycobacterium leprae . The former causes tuberculosis, and the latter is the cause of leprosy. It takes 6-8 weeks to grow Mycobacterium tuberculosis in artificial culture, and as yet Mycobacterium leprae cannot be grown in artificial culture. Mycobacterium tuberculosis Bacteria in human sputum. LM X1600 Mycobacterium tuberculosis in sputum, stained by the Ziehl Neelsen technique The red rods visible in the image above are cells of Mycobacterium tuberculosis seen in a film made from a sputum sample. They have retained the strong carbol fuchsin dye that has penetrated the cells following heating of the slide to steam heat, even though the film has been decolourised with a mixture of acid and alcohol. Because of this property, mycobacteria are referred to as acid alcohol-fast. The background material has been counterstained with methylene blue. Gram-negative cocci Medically, the most important of the Gram-negative cocci belong to the genus Neisseria. Neisseria meningitidis is an important cause of bacterial meningitis, and Neisseria gonorrhoeae causes gonorrhoea. Members of the genus Neisseria are most often seen in pairs, and are hence sometimes referred to as diplococci. They are very vulnerable to drying, and can only be cultivated in an atmosphere where the concentration of carbon dioxide is greater than that found in air. In the laboratory, carbon dioxide incubators are used that maintain a moist environment with a carbon dioxide concentration of 5-10% Gram-negative cocci Neisseria gonorrhoeae in pus from a urethral discharge This bacterium is typically found in pairs, known as diplococci. Here the diplococcal cells are seen within a polymorphonuclear leukocyte seen in pus from a urethral discharge. This is sufficient information to make a provisional diagnosis of gonorrhoea, which will be confirmed following a positive culture result, Gram-negative bacilli Enterobacteriaceae This image shows the typical appearance of Escherichia coli when stained using the Gram staining method The Enterobacteriaceae are a large family of medically important Gram-negative bacilli. They can grow in the presence or absence of oxygen, and are frequently found in the guts of humans and other animals, and hence their name. They are differentiated from one another largely on the basis of their metabolic behaviour and on their antigenic structure. Some, like Escherichia coli and members of the genus Klebsiella can ferment lactose to produce acid, whereas others including salmonellas, shigellas and proteeae cannot and are thus known as non-lactose fermenters (NLF's). There are almost 2,000 different varieties of salmonella recognised on the basis of differences in their surface antigens. Members of the genus Proteus are so highly motile that a single colony can grow to swarm over the entire surface of a Petri dish after overnight incubation. This is how the genus acquired its name, from Proteus, the Greek sea god who had the miraculous ability to change his shape. The family Enterobacteriaceae include Yersinia pestis, the cause of plague, Salmonella typhi, the cause of typhoid, Shigella dysenteriae, the cause of bacilliary dysentery, and Salmonella enteritidis implicated in many cases of food poisoning. Mixed bacterial colonies on MacConkey agar, Escherichia coli (red) and Salmonella typhimurium (white). Some bacteria are enclosed within a capsule. This protects the bacterium, even within phagocytes, helping to prevent the cell from being killed. Encapsulated bacteria grow as 'smooth' colonies, whereas colonies of bacteria that have lost their capsules appear rough. Rough colonies do not generally cause disease. Encapsulated bacteria do not succumb to intracellular killing as easily as bacteria that lack capsules. Cultures of Salmonella typhimurium on tryptone glucose agar (left) and on MacConkey agar (right). Salmonella typhosa: gram negative, brightfield. LM X500 Conventional Biochemical tubes for Shigella spp Conventional Biochemical tubes for Salmonella spp TABLE 1: BIOCHEMICAL IDENTIFICATION OF ENTERIC Pathogens K Shigella dysenteriae K Shigella flexneri K Shigella boydii Shigella sonnei Aeromonas Spp. 0% K 1% Other Salmonella spp. 8% K Oxidase Salmonella pullorum Urease K NaCl U Butt Salmonella gallinarum LIA Slant K O Ornithine S. paratyphi A + + - - K K - - - + - + K A - - A V - - V K V - - A V - - V K V - - + + - + K K - - A A - - V - K A - - - - V - K A - - K A - - V - K A - - K A - - - + K A - - A - + V - K A - + - + + K @ A Indole K I Motility S. typhi M H2S butt Slant Identification A I AG AG * Plesiomonas spp. K A - + + + K K - + - + + Vibrio cholerae K A - + + + K K - + - + + V. parahaemolyticus K A - + + + K K - + + + - V. fluvialis K A - + V - K A - + - + - Symbols: KIA: Kligler Iron Agar, MIO: Motility Indole Ornithine Agar, LIA: Lysine Iron Agar, K: alkaline, A: acid, G: gas, S: slant, B: butt, Ure: urease, Oxid: oxidase, * Some strains produce gas. @ Some strains ferment lactose (KIA=A/A) according to Farmer and Kelly, (1991) Pseudomonads Members of the family Enterobacteriaceae do not elaborate the enzyme complex known as "oxidase", whereas many Gram-negative bacteria do. Pseudomonas aeruginosa is an oxidase-positive Gram-negative bacillus that is an obligate aerobe. It cannot be grown in the absence of oxygen. It is responsible for wound infections, and the bacteria in this species produce a soluble pigment. Culture of Pseudomonas aeruginosa Bacteria on blood agar. Curved Gram-negative rods • • The vibrios and campylobacters are Gram-negative rods that appear curved or spiral in shape. These bacteria are commonly found in natural waters, both fresh-water and marine. Vibrio cholerae causes cholera, a waterborne infection. Campylobacters have only been recognised as human pathogens since the late 1970's, although they have been long considered to be animal pathogens. Campylobacters are now responsible for more cases of bacterial enteritis annually than salmonellas. The bacterium Helicobacter pylori, found associated with stomach ulcers, is a good example of a bacterium that has undergone a radical change in taxonomy. When they were first observed, they could not be cultured and were called "campylobacter-like organisms". Conditions were then discovered that allowed these bacteria to be grown in artificial culture, and they were first called Campylobacter pyloridis. This was then found to be linguistically incorrect, and the name was corrected to Campylobacter pylori. Later, molecular studies showed that it was not very closely related to the other campylobacters, and they then became the type species of a new genus, Helicobacter. This entire process of taxonomic change took less than five years. Campylobacter Species speciation chart Skirrow Campy plate primary plate 42 degrees C Microaerophilic Oxidase Test Positive Oxidase Test negative Gram Stain Gram negative curved rods Not Campylobacter spp Hippurate Hydrolysis Positive Negative C.jejuni Indoxyl Acetate Hydrolysis positive C.coli positive negative Catalase test Campylobacter species negativ C.upsaliensis Other Gram-negative bacilli • • • Some Gram-negative bacilli appear so short that they resemble cocci in the light microscope. Because of this they are sometimes called cocco-bacilli. These include members of the genus Moraxella, related to the neisserias, and also members of the genus Acinetobacter. Members of this genus are increasingly associated with hospital-acquired infection. Some Gram-negative bacteria are very fastidious (fussy) in their nutritional requirements. Members of the recently recognised genus Legionella, some of which cause atypical pneumonias like Legionnaires' disease, require higher levels of iron and cysteine than are usually present in bacteriological media, and they grow best in media that incorporate activated charcoal to adsorb their toxic metabolic products. Similarly bacteria of the genus Bordetella also generate toxic metabolic products that inhibit their own artificial culture. These bacteria also grow best on media that contain activated charcoal. Bordetella pertussis, the cause of whooping cough, is an important member of this genus. At one time, species of the genus Bordetella were classified in the genus Haemophilus, but they were re-classified. This is partly because they require neither the X- nor the V-factor for growth such as required by members of the genus Haemophilus. The X-factor has now been identified as haem, and the V-factor is nicotinamide adenine dinucleotide or NAD. Haemophilus influenzae requires both X- and V-factors for growth whereas Haemophilus parainfluenzae requires just the V-factor to support its growth, since it can elaborate its own supply of haem. The most important group of obligately anaerobic Gram-negative bacilli are the bacteroides. This is a heterogeneous group that form part of the human commensal flora, and that are also implicated in anaerobic infections. The taxonomy of the anaerobic Gram-negative rods is currently undergoing radical revision. X and V dependence in Haemophilus influenzae The pathogenic Haemophilus influenzae can be differentiated from its non-pathogenic relative, Haemophilus parainfluenzae, by its dependence on an external supply of two growth factors, known as 'X' (haem) and 'V' (NAD). Haemophilus influenzae requires both, while Haemophilus parainfluenzae requires only the 'V' factor, since it can make its own haem. In the image above, the bacteria can only grow around the disc containing both 'X' and 'V' factors, indicating that it is the pathogen, Haemophilus influenzae. X and V dependence may also be demonstrated by the phenomenon of 'satellitism'. The second image above illustrates this. A lawn of test bacteria is plated onto a fresh blood agar plate. This provides a supply of haem. An inoculum of Staphylococcus aureus, which can provide NAD, is placed on the plate and the culture is incubated. Haemophili can be seen growing larger near to the staphylococcal colony, where the supply of NAD is greatest. Colonies of haemophili growing further from the staphylococcal colony are proportionately smaller, as the supply of NAD from the staphylococcus diminishes. This test is good for detecting haemophili, but cannot distinguish the pathogenic Haemophilus influenzae from Haemophilus parainfluenzae. Haemophilus influenzae • Haemophilus influenzae Bacteria, a gram-negative rod that causes Bacterial . Meningitis. LM X500 (Haemophilus influenzae) and (Staphylococcus) satellite test (Haemophilus influenzae) and (Staphylococcus aureus) on blood agar, culture (Haemophilus influenzae) and (Staphylococcus) satellite test Quality control procedures for commonly used tests Procedure/ Test Control organism Expected result Expected reaction Catalase Staph aureus Streptococcus species + – Bubbling reaction No bubbling Coagulase Staph aureus + Clot formation in 4 hours No clot Staph epidermidis – Indole Esch coli Enterobacter aerogenes + – Red ring at surface Yellow ring at surface Methyl red Esch coli Ent aerogenes + – Instant red colour No colour change Oxidase P. aeruginosa + Purple colour in 20 seconds No colour in 20 seconds Esch. coli – Voges Proskauer Enterobacter aerogenes Esch. coli + – Red colour No colour change Bacitracin disc Streptococcus group A Enterobacter faecalis + – Zone of inhibition No zone of inhibition Optochin disc Strept. Pneumoniae Strept. viridans + – Zone of inhibition No zone of inhibition ONPG disc Esch. Coli Proteus vulgaris + – Yellow colour No change in colour Oxidase disc P aeruginosa + Purple colour in 30 seconds No change in colour Esch. coli – Quality control procedures • It is also essential to undertake quality control procedures at regular intervals. These should be performed: • With each new batch of reagents • With each new vial of reagent • Daily for catalse, oxidase, and coagulase • Weekly for bacitracin, optochin and ONPG • A test procedure not giving anticipated results with the control organisms should not be used till such time that remedial steps have been taken to correct the Basic sets of drugs for routine susceptibility tests Set 1 Set 2 Staphylococcus Benzylpenicillin Oxacillin Erythromycin Tetracycline Chloramphenicol Gentamicin Amikacin Co-trimoxazole Clindamycin - Intestinal Ampicillin Chloramphenicol Co-trimoxazole Nalidixic acid Tetracycline Norfloxacin Enterobacteriaceae Urinary Sulfonamide rimethoprim Co-trimoxazole Ampicillin Nitrofurantoin Nalidixic acid Tetracycline Norfloxacin Chloramphenicol Gentamicin Blood and tissues Ampicillin Chloramphenicol Co-trimoxazole Tetracycline Cefalotin Gentamicin Cefuroxime Ceftriaxone Ciprofloxacin Piperacillin Amikacin Piperacillin Gentamicin Tobramycin Amikacin Pseudomonas aeruginosa Factors influencing zone size in antibiotic susceptibility testing Factor Influence Inoculum density Larger zones with light inoculum and vice versa Timing of disc application If after application of disc, the plate is kept for longer time at room temperature, small zones may form Temperature of incubation Larger zones are seen with temperatures < 35oC Incubation time Ideal 16-18 hours; less time does not give reliable results Size of the plate Smaller plates accommodate less number of discs Depth of the agar medium Thin media yield excessively large inhibition zones and vice versa Proper spacing of the discs Avoids overlapping of zones Potency of antibiotic discs Deterioration in contents leads to reduced size Composition of medium Affects rate of growth, diffusion of antibiotics and activity of antibiotics Acidic pH of medium Tetracycline, novobiocin, methicillin zones are larger Alkaline pH of medium Aminoglycosides, erythromycin zones are larger Incubation in the presence of CO2 Increases zone size of tetracycline and methicillin Addition of thymidine to medium Decreases activity of trimethoprim Addition of defibrinated blood Decreases activity of sulfonamides On chocolate agar, decreased activity of Sulfonamides, trimethoprim, aminoglycosides Reading of zones Subjective errors in determining the clear edge Chelating agents such magnesium and iron as cal-cium, Decreases diffusion of tetracycline and gentamicin Need for quality control in susceptibility test • The final result of a disc diffusion test is influenced by a large number of variables. Some of the factors, such as the inoculum density and the incubation temperature, are easy to control, but a laboratory rarely knows the exact composition of a commercial medium or the batch-tobatch variations in its quality, and it cannot take for granted the antimicrobial content of the discs. The results of the test must, therefore, be monitored constantly by a quality control programme which should be considered part of the procedure itself. • The precision and accuracy of the test are controlled by the parallel use of a set of control strains, with known susceptibility to the antimicrobial agents. These quality control strains are tested using exactly the same procedure as for the test organisms. The zone sizes shown by the control organisms should fall within the range of diameters given in Table 11.4. When results regularly fall outside this range, they should be regarded as evidence that a technical error has been introduced into the test, or that the reagents are at fault. Each reagent and each step in the test should then be investigated until the cause of the error has been found and eliminated Quality Control – Susceptibility of Control Strains* Diameter of zone of inhibition (mm ) Antibiotic Disc potency Staph.aureus (ATCC 25923) Esch.coli (ATCC 25922) P.aeruginosa (ATCC 27853) Amikacin 30 mg 20-26 19-26 18-26 Ampicillin 10 mg 27-35 16-22 – Ceftriaxone 30 mg 22-28 29-35 17-23 Cephalothin 30 mg 29-37 15-21 – Chloramphenicol 30 mg 19-26 21-27 – Ciprofloxacin 5 mg 22-30 30-40 25-33 Clindamycin 2 mg 24-30 – – Erythromicin 15 mg 22-30 – – Gentamicin 10 mg 19-27 19-26 16-21 Nalidixic acid 30 mg – 22-28 – Nitrofurantoin 300 mg 18-22 20-25 – Norfloxacin 10 mg 17-28 28-35 – Oxacillin 1 mg 18-24 – – Penicillin G 10 units 26-37 – – Piperacillin 100 mg – 24-30 25-33 Tetracycline 30 mg 19-28 18-25 – Tobramycin 10 mg 19-29 18-26 19-25 *NCCLS: 1995 Trimethoprim 5 mg 19-26 21-28 – Trimethoprimsulfamethoxazole 1.25/23.75 24-32 24-32 – Troubleshooting guide for disc diffusion test in antibiotic susceptibility testing Aberrant results Probable cause Tetracycline zone too small pH of medium too low Aminoglycoside zone too small pH of medium too high Aminoglycoside zone too large Ca2+ and/or Mg2+ level too high in medium Ca2+ and/or Mg2+ level too low in medium Too large zone on control plates Inoculum too light Nutritionally poor medium Slow growing organisms (not seen with controls) Improper medium depth (too thin) Zone universally too small on control plates Inoculum too heavy Methicillin zone indeterminant in disc test Methicillin degraded by strong b lactamase producing staphylococci Carbenicillin zone disappears with Pseudomonas control Resistant mutant has been selected for testing Single disc result above or below control limits Error in reading, fuzzy zone edge, transcription error, bad disc Disc may not be pressed firmly onto agar surface Colonies within zone of inhibition Mixed culture Resistant mutants within zone Zones overlap Discs too close together Zones indistinct Poorly streaked plates Zone within zone phenomenon Swarming Proteus species Feather edge of zones around penicillin or ampicillin discs usually with b lactamase negative strains of Staph.aureus PCR Gram negative cell wall Gram positive cell wall Back to FRET Fluorescence Resonance Energy Transfer Reporter-Quencher probe system that allows the detection, and quantifying, of nucleotide amplification in real time. R R Q e- Q __________________________________________________________ TaqMan Bacteria The bacterial cell lacks a membrane-bound nucleus. Because of this, bacteria are described as prokaryotes, "pro-" meaning "before" and "-karyon" from the Greek word for a "nucleus". There are three basic shapes that bacterial cells adopt. They are either round, rod shaped or spiral. Round bacteria are referred to as cocci (singular: coccus), and rod shaped bacteria are known as bacilli (singular: bacillus). The term 'bacillus' meaning a rod-shaped bacterium should NOT be confused with the genus of bacteria known as 'Bacillus'. Staphylococci Diplococcal cells of Streptococcus pnuemoniae Streptococci Sporing cells of Clostridium tetani Note spores do not stain and in this case cause the bacilli to swell Sporing cells of Bacillus anthracis Note spores do not cause the bacilli to swell in this species Spiral cells of Treponema pallidum This bacterium causes syphilis and is so slender that it cannot be seen using conventional light microscopy. It is most easily visualized using dark-ground microscopy. Irregular cells of Corynebacterium diphtheriae Various shaped cells of Haemophilus influenzae Curved rods of Vibrio cholerae • Strains of Streptococcus pnuemoniae that lack capsules do not cause disease. All the bacteria that cause meningitis are encapsulated. • Suspending bacteria in India ink is an easy way of demonstrating capsules. Ink particles cannot penetrate the capsular material and encapsulated cells appear to have a halo around them. This is the Quellung reaction. • In the 'Quellung' reaction, bacterial cells are resuspended in antiserum that carries antibodies raised against the capsule. This causes the capsule to swell, and this can be easily visualised by suspension in India Ink. The ink particles cannot penetrate the capsule, which this appears as a halo around the bacterial cells. The Quellung reaction Endospores (or simply spores) • A few species of bacteria have the ability to produce highly resistant structures known as endospores (or simply spores). These resist a range of hazardous environments, and protect against heat, radiation, and desiccation. • Endospores form within (hence endo-) special vegetative cells known as sporangia (singular sporangium). • Diseases caused by sporing bacteria include botulism (Clostridium botulinum), Ggas gangrene (Clostridium perfringens), Ttetanus (Clostridium tetani) Acute food poisoning (Clostridium perfringens, again) All these bacteria are 'anaerobic'. The aerobic sporing bacteria can also cause disease. Anthrax is caused by Bacillus anthracis. Bacillus cereus causes two types of food poisoning. • • • • • Microfungi Microfungi All fungi are eukaryotic. Most possess a cell wall made of chitin: a polymer of N-acetyl glucosamine that is found in the cell walls of the majority of fungi. It is also a major component of the exoskeleton of arthropods such as insects. The cell walls of plants are made of cellulose whereas the walls of fungal cells are made of chitin and other polymers. Chitin is also the material found in insect shells. The dreaded•). black mould in the bathroom of the student flat? This is most likely to be a fungus of the genus Cladosporium. Who has not seen Penicillium spp. growing on stale bread? These are all moulds: fungi that grow in mats of tiny filaments known as hyphae (singular: hypha, Greek for a thread) or mycelia (singular: mycelium, from the Greek mukes, meaning a mushroom). These may or may not be subdivided into separate compartments by cross walls known as septa (singular: septum). Aseptate and septate mycelia Moulds are multicellular organisms. There are, however, unicellular fungi: the yeasts. Most familiar of the yeasts is Saccharomyces cerevisiae. Depending upon your viewpoint, this is baker's yeast, used in the production of leavened bread, or brewer's yeast, used in alcohol production. Yeasts grow and multiply by budding daughter cells off from a mother cell. Budding Yeasts Fungi can multiply either sexually or asexually. In classifying fungi, great weight is placed upon the appearance and structure of sexual fruiting bodies. Any fungus that does not exhibit a recognizable sexual structure is difficult to classify. They are grouped in the collection known as "fungi imperfecti". Among the most important of fungi imperfecti are members of the genus Penicillium. It is from these fungi that we derive penicillins. These were the first true antibiotics and are still among the most used antimicrobial agents world-wide. Fungi also produce a staggering variety of spores. These may be produced asexually or sexually and are important in the identification of moulds. Examples of asexual spore structures produced by fungi The umbrella is the spore-bearing structure once it has discharged its load Asexual spores can be enclosed within specialised sacs The umbrella is the spore-bearing structure once it has discharged its load Examples of sexual spore structures produced by fungi Spores within an enclosed structure - a cleistothecium The warty zygospore is suspended between two mycelia of different mating types Spores contained inside a more open structure - a perithecium Moulds cause a variety of common, superficial infections such as ringworm and athlete's foot. In compromised individuals they can cause much more severe infections but these are rare. The most common yeast infection is "thrush" caused by Candida albicans. Under certain conditions, some yeasts have the ability to develop pseudomycelia. This happens, for example, when the commensal form of Candida albicans causes active thrush. "Pseudomycelia" produced by Candida albicans Gram-stain of vaginal smear showing Candida albicans, epithelial cells, and many gram-negative rods Gram-stain of vaginal smear showing Candida albicans epithelial cells and many gram-negative rods. (1,000X oil) Viruses Viruses • • • • • Viruses are obligate intracellular parasites (requires to live within a cell in its host). They comprise a nucleic acid core wrapped in a protein coat. Some viruses have an envelope, made of lipid and usually derived from the cell in which they grow. Other viruses are naked and just have their protein coat exposed, protecting the nucleic acid within the centre of the structure. Specific viruses attack specific types of cells. Respiratory syncytial virus infects only the cells of the respiratory tract, for example. There is a special class of virus that attacks bacteria. These are the bacteriophage. Most viruses are simple in shape: round, rod-shaped, icosahedral, brick-shaped or bullet-shaped Viruses have a nucleic acid core, either DNA or RNA but not both. Retroviruses are unusual in that the virion carries an RNA copy of the genome but upon infection of a host cell a cDNA copy of the virus genome is made using the enzyme reverse transcriptase Human immunodeficiency virus - the cause of AIDS Around the nucleic acid core lies a protein coat, made up of units called capsomeres. Some viruses also have an envelope derived from the host cell membranes. The envelope may be either baggy or tight, depending upon the nature of the virus. •. Rabies virus Adenovirus - associated with respiratory and gastrointestinal disease A T-even bacteriophage that can infect Escherichia coli Herpes simplex virus (note the lipid envelope)