Peptic Ulcer Disease
advertisement

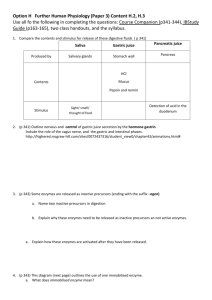
TASHKENT - 2011 1 2 Erect radiographic image of esophagus (lower portion), stomach and first part of duodenum after ingestion of contrast medium 3 Topography and internal surface of a stomach (blue line represent notional lines marking the parts of the stomach) 4 Microscopic section of a gastric gland 5 THE PARIETAL CELLS – acid secretion THE CHIEF CELLS – pepsinogen secretion THE ENDOCRINE CELLS: ◦ The G-cells – gastrin secretion ◦ The D-cells – somatostatin secretion ◦ The ECL-cells – histamine production THE MUCOUS NECK CELLS – mucus secretion 6 Components involved in providing gastroduodenal mucosal defense and repair 7 Primary chronic recurrent disease of upper gastrointestinal tract associated with circumscribed ulcers within stomach and duodenum 8 is disruption of the mucosal integrity of the stomach and/or duodenum leading to a local defect or excavation due to active inflammation 9 1 – submucosa 2 – hard, undermined margin 10 11 A break in the mucosa not penetrating muscularis mucosa Peristalsis is not affected Heals rapidly 12 Duodenal ulcers (5x) > gastric ulcers ♂ (4x) > ♀ Urban resident > rural resident 13 Helicobacter pylori NSAIDs (aspirin) 14 Healthy subjects Chronic active gastritis Duodenal ulcer Gastric ulcer Gastric adenocarcinoma Gastric lymphoma 20-50% 100% >90% 50 - 80% 90% 85% 15 Barry Marshal Robin Warran 16 Predisposing factors Producing factors Heredity Active duodenitis or gastritis Emotional stress Gastric metaplasia Blood group 17 Aggravating causes of, and defense mechanisms against, peptic ulceration 18 Any area where pepsin and acid are present Prevailing locations ◦ Duodenum: duodenal bulb ◦ Stomach: over lesser curvature 19 I type – ulcers of lesser curvature of stomach II type – combined ulcers of stomach and duodenum III type – ulcers of prepyloric part stomach IV type – ulcers of duodenum 20 21 PAIN LOCATION TIME CHARACTER IRRADIATION PAIN RELIEF •Gastric ulcer: in the centre of or left to epigastrium •Duodenal ulcer: to the right of midline in epigastruim •Early: 0.5-1 h after meal, duration 1.5-2 hh, in gastric ulcers •Late: 1.5-2 hh after meal, in duodenal and pyloric ulcers •Nocturnal •Pain of “hunger”: 6-7 hh after meal and ceased after meal •Burning •Gnawing •Dull •Cramplike •Cardiac area •Left scapula •Thoracic part of spinal column •Lumbar region •Antacids •Milk •Meal •After vomiting 22 DYSPEPSIA HEARTBURN BELCHING NAUSEA & VOMITING APPETITE •Related with gastroesophageal reflux •After meal •More common in gastric ulcers •At the peak of pain •More common in gastric ulcers •Pain relief after vomiting •Excessive 23 Vegetative dystonia: cold, damp palms, mottled skin, bradycardia, hypotension Palpation: tenderness Percussion: Mendel’s symptom, succussion splash (gastric outlet obstruction) 24 Non-complicated PUD – service of 1st category Complicated PUD – service of 2nd category Services of 3.1 category: Services of 3.2 category: Services of 4 category: ◦ ◦ ◦ ◦ ◦ Professional examination Interpretation of clinical and biochemical tests CBC Gastric lavage Diet prescription ◦ ◦ ◦ ◦ ◦ Analysis of gastric juice and duodenal contents Ultrasound Endoscopy Radiologic examination Biopsy ◦ Rational nutrition ◦ Struggle with harmful habits ◦ Personal hygiene 25 CBC • ↑Hb • ↑Erythrocyte Secretory function of stomach Occult blood feces analysis Endoscopy X-ray (Barium meal) • ↑BAO (N=5 mmol/h) • Latent PUD • Round or oval • Niche sign • Exacerbation • ↑MAO (N=18-26 mmol/h) • Stomach cancer • Edges: sharp, hyperemic, edematous • Retention of barium meal • Duodenogastric reflux • Fold convergence • Local spasm of stomach *BAO – basal acid output *MAO – maximal acid output •Biopsy •Test with Insulin •Test with Histamine •pH meter •Gastrin concentration in serum 26 Invasive( through endoscopy) ◦ Gastric biopsy and staining ◦ Culture of biopsy specimen ◦ Tests using urease enzyme in biopsy specimens Non-invasive: ◦ ◦ ◦ ◦ Urea breath test H.pylori antibodies Stool antigen Salivary antigen 27 28 29 30 31 32 33 34 35 Haemorrhage Perforation Penetration (pancreas, liver) Pyloric stenosis (due to scarring) Malignization 36 37 Hematemesis Melena Bergman’s symptom 38 I STAGE II STAGE III STAGE Signs of stopped fresh haemorrhage Actively bleeding ulcer Thrombosed vessels at the bottom of ulcer Absence of bleeding apparent signs Clot of blood 39 40 41 Compensation Subcompensation Decompensation 1-0.5 cm 0.5-0.3 cm <0.3 cm 42 Neoplasm of the stomach Pancreatitis Pancreatic cancer Diverticulitis Nonulcer dyspepsia (also called functional dyspepsia) Cholecystitis Gastritis MI—not to be missed if having chest pain 43 Diet №1: white stale bread, vegetable soups, softly boiled porridge, potato mash, fish, birds, mature fruits, berry and fruit juices, cottage cheese, milk, omelette, pudding Banned: spicy foods, marinated and smoked products Frequent small meals: 6-7 times a day 44 H.pylori supressors: De-nol, Metronidazole, Antisecretory drugs Furazolidone, Oxacillin, Amoxycillin • M-anticholinergic drugs: • Nonselective: Atropine, Platyphyllin, Methacin • Selective: Gastrozepine, Pirenzepine • H2-histamine receptor blockers: Cimetidine, Ranitidine, Famotidine • Proton pomp inhibitors: Omeprazole, Lansoprazole, Rabeprazole • Antagonists of gastrin receptors: Milid, Proglumide • Antacids: Magnesium hydroxide, Aluminum hydroxide, Almagel, Maalox 45 Gastrocytoprotectors • • • Cytoprotectors that stimulate mucus production: Carbenoxolone, synthetic prostaglandins (Enprostile, Misoprostole) Cytoprotectors that form protective film: Sucralfate, colloid bismuth (De-nol), Smecta Astringents: Vicaline, Vicair Drugs that normalize motor function of stomach and duodenum (Metoclopramide), spasmolytics (Papaverine, No-spa) 46 H2-blockers: gynecomastia, impotence Aluminum hydroxide: constipation Magnesium hydroxide: diarrhea 47 De-nol 1 tablet 3 times/day, 4-6 weeks Clarythromycin 250 mg, 2 times/day, 7-10 days Metronidazole 250 mg, 4 times/day, 14 days 48 De-nol [4-6 weeks] Metronidazole + [10-14 days] De-nol [4-6 weeks] + Tetracyclin OR Amoxycillin Amoxycillin + Omeprazole [10 days] OR Clarythromycin [7- 10 days] [40 mg, 4-6 weeks] 49 De-nol [4-6 weeks] + Metronidazole [10-14 days] Tetracyclin [7-10 days] Omeprazole + Amoxycillin OR Clarythromycin + Metronidazole Metronidazole [10-14 days] + Amoxycillin [10 days] + Ranitidine [150 mg, 10-14 days] 50 Omeprazole + De-nol+ Amoxycillin OR Clarythromycin + Metronidazole 10 days 51 • Revelation and elimination of risk factors PRIMARY • Sanitary and prophylactic measures • Early diagnosis and timely treatment • Screening, professional examination, SECONDARY questionnarires • Prevention of complications TERTIARY 52 53 54