Care of Patient with GERD & Peptic Ulcer
advertisement

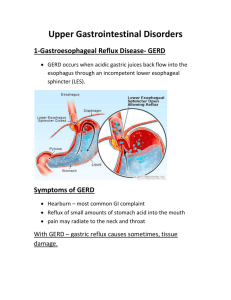
Care of Patient with GERD & Peptic Ulcer 63-273 1 GERD: Background Gastroesophageal reflux is a normal physiologic phenomenon in most people, particularly after a meal. Gastroesophageal reflux disease (GERD) occurs when the amount of gastric juice that refluxes into the esophagus exceeds the normal limit 2 Causes of GERD 3 GERD: Symptoms Typical symptoms: Heartburn (Pyrosis): Regurgitation: Most common Felt as a retrosternal sensation of burning or discomfort Occurs usually after eating or when lying down or bending over. Often relieved with milk or water Effortless return of gastric and/or esophageal contents into the pharynx. It can induce respiratory complications if gastric contents spill into the tracheobronchial tree. Atypical symptoms Cough, dyspnea, hoarseness, and chestpain 4 Diagnosis Role out other potential causes for the heartburn: Cardiac Peptic ulcer Esophagitis Esophageal Endoscopy: The gold standard as a definitive diagnosis Barium swallow Not as definitive in mild cases 5 Collaborative Care Lifestyle modifications Nutritional therapy Decrease high-fat foods, avoid milk products at night, and avoid late snacking or meals Drug Therapy Surgical therapy Endoscopic therapy 6 GERD: Complications Are related to HCl effect on the esophageal mucosa Esophagitis Can complicate to esophageal ulceration Barrett’s esophagus (esophageal metaplasia) Pre-cancerous lesion 7 Nursing Management Avoid factors that cause reflux Stop smoking Avoid acid or acid producing foods Elevate HOB ~30° Do not lie down 2 to 3 hours after eating Patient teaching (see Table 40-10 in textbook) Drug therapy Evaluate effectiveness Observe for side effects 8 Peptic ulcer Erosion or excavation of mucosal wall of the esophagus, stomach, pylorus, duodenum (most common). “Autodigestion” Requires acid environment to develop Mucosal defenses impaired; cannot protect from effects of acid/pepsin Result from infection with H. pylori or Zollinger-Ellison syndrome Risk factors: Alcohol, smoking, and stress, medications 9 Three types of peptic ulcer Gastric Duodenal Stress 10 Gastric ulcer Most common in the lesser curvature of stomach near the pylorus Mucus and bicarb. generally protect mucosal barrier from acid H. pylori plays a role Break in gastric mucosal barrier allows HCl to damage epithelium via “back diffusion” Bile reflux from duodenum may break integrity Decreased blood flow 11 Duodenal ulcer Results from excessive acid Associated with protein-rich meals, Ca++, and vagal stimulation) Rapid emptying of food from stomach large acid load in duodenum H. pylori infection plays key role in development produces substances that damage the mucosa, and contributes to higher acid concentrations 12 Stress ulcer Occurs after acute medical crisis, surgery, or trauma Proximal portion of stomach and duodenum are most common sites Ischemia and elevated HCl contribute to evolution of erosions ulcerations May progress to hemorrhage 13 Duodenal versus Gastric ulcers Gastric Normal/hypo-secretion of gastric acid Pain 1-2 hrs pc meals Food aggravates pain Vomiting common More likely to hemorrhage – manifests as hematemesis Duodenal Hyper-secretion Pain 2-4 hrs pc meals Food may relieve pain Vomiting not common Less likely to hemorrhage, but if occurs, likely to manifest as melena 14 Diagnostic tests Esphagogastroduodenoscopy Fiberoptic endoscope allows direct visualization of esophagus, stomach and duodenum 15 Diagnostic tests: Upper GI series Patients ingests barium, a thick, white, milkshake-like liquid, then multiple X-rays. Can detect structural disorders After the exam, provide plenty of liquids for 24 to 48 hours. The barium may make the stool white for several days. If constipation occurs, the doctor may recommend a mild laxative. 16 Complications of ulcers: Hemorrhage Manifested by: Orthostatic hypotension, BP, HR, cool, clammy skin overt bleeding Hematemesis (bloody vomit) – bright red or coffee ground (more likely with gastric ulcer) Melena (bloody or tarry [black] stool) – more likely with duodenal ulcer Hgb, Hct 17 Remember: Management during Haemorrhage includes Monitor S/S Determine rate amount of blood loss (Hct/hct), NGT Replace blood, fluid and electrolyte loss saline lavage via NGT NGT to low intermittent suction Prevents distension Assess amount/rate of bleeding, Medications, oxygen, possible surgery 18 Complications: Perforation GI contents empty into peritoneal cavity Manifested by: Sudden, sharp mid-epigastric pain which can shortly spread to all abdomen Rigid, tender, board-like abdomen Patient assumes the fetal position to reduce tension on muscles Can lead to shock It is a surgical emergency 19 Remember: Management during perforation includes NGT to prevent additional spillage of GI contents in peritoneum Replace blood, fluid, electrolytes Antibiotics I & O, NPO SURGERY: Urgent 20 Complications: Pyloric obstruction Caused by inflammation or edema of the pylorus Stomach cannot empty abdominal bloating, N&V Persistent vomiting Hypokalemia and metabolic alkalosis 21 Medical Management of ulcers Conservative therapy: Rest: Both physical and emotional Dietary modifications Elimination of smoking Long term follow up care Pharmaceutical: Antibiotics Antiacids Initial drugs of choice Histmaine H2 receptor antagonists To eradicate H. Pylori infections Recurrence of ulcer is 75-90% as high with infection Histamine is the final intracellular activator of HCL secretion Anticholinergic: Stop the cholinergic stimulation of HCl secretion and slow gastric motility Not commonly used, if used need to be used with caution in pts with Glaucoma 22 Surgical Management of ulcerations Gastroduodenostomy (Billroth I) Removal of the lower portion of stomach and small portion of duodenum and connects remaining of stomach to duodenum 23 Surgical Management of ulcerations Gastojejunostomy Removes lower stomach and small portion of duodenum. Reconnects stomach to jejunum. Subtotal gastrectomy - removal distal third of stomach, reconnecting to duodenum or jejunum Total gastrectomy removal of stomach; connects esophagus to jejunum 24 Dumping syndrome A complication of gastric surgery S&S occurs after eating vertigo, sweating, palpitations, syncope, pallor, tachycardia D/t rapid emptying of hypertonic stomach contents into small intestine fluid shifts into gut abd. distention and cramps and S/S of plasma volume. Later get rapid elevation of blood glucose followed by insulin secretion and hypoglycemia Management Small frequent meals fat, protein, CHO meals liquid between (not with) meals Lie down after meals 25 Nursing diagnoses Pain r/t mucosal injury Anxiety Knowledge deficit Risk for fluid volum deficit r/t hemorrhage or vomiting 26 Intervention: Pain Medications Give antacids after meals and at bedtime to decrease gastric acidity; buffers the acid. Give H2 receptor antagonists as prescribed to decrease acid secretion Diet therapy Effectiveness controversial Avoid caffeinated beverages Exclude foods that cause discomfort Provide frequent, small, bland meals Avoid smoking, alcohol 27 Intervention: Anxiety & Knowledge deficit Anxiety Provide emotional support Teach and provide relaxation techniques Identify and manage sources of stress Knowledge deficit Teach re diet, medications, Teach the risks associated with continued smoking Teach S/S of complications 28