Brain Injury Program (continued)
advertisement

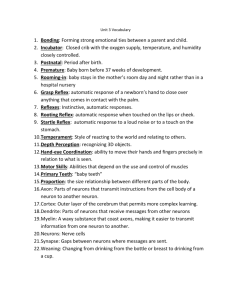
Overview Nuclear lamin molecules DNA Non-muscle myosin-II molecules Dr. O’neil W. Guthrie is the Director of the Cell and Molecular Pathology Laboratory (CMPL). The CMPL is broadly focused on defining the cellular and molecular bases of diseases as a necessary prerequisite to the development of biomedical therapies. To this end, work in the CMPL is identifying and manipulating endogenous molecular mechanisms that mediate cellular/tissue injury and repair. The laboratory employs multiple strategies that encompasses molecular biology, biochemistry, genetics, epigenetics, exploratory pharmacology, electrophysiology, microscopy, histopathology & cytology and design-based stereology. RESEARCH PROGRAMS BIOMEDICINE DISCOVERY PROGRAM The CMPL is interested in developing biomedical approaches to prevent or treat intractable conditions such as hearing loss. Therefore, two independent approaches are currently under research and development. The newest approach is based on the engineering of specific molecular constructs that will increase the capacity of cells to repair themselves after injury (further information is restricted at this time). The other approach employs specific low molecular weight chemotypes called carboxy alkyl esters (CAEs) to enhance recovery of sensory and neural functions following injury. This research is important because it suggests (for the first time) that CAEs may be used as a novel approach to prevent or treat hearing loss. The goals of this line of research are to 1) determine the underlying molecular mechanisms that facilitate cellular repair, 2) optimize the treatment regimen to achieve maximal repair, 3) identify other molecules that have the capacity to augment cellular repair, and 4) conduct clinical trials to determine efficacy among patients. What are CAEs and how do they work? CAEs are phytochemicals found in healthy foods and beverages such as fruits, vegetables, coffee and tea. They provide direct trophic support to cells. However, they can function through systemic metabolism. For instance, CAEs are involved in systemic biochemical reactions that increase bioavailability of essential nutrients. One proposed reaction that is currently under investigation is illustrated. OOH HO C OH 1 5 4 OH 1 3 Quinic acid O OH OH OH O (CAE) HO OOH HO C O 4 OH H2 O 2Pi Caffeic acid COO 1 5 4 3 OH NAD ATP PEP OH esterase 5 OH A OOH HO C B H 3 OH CH2 OH OH Quinic acid O Chorismate C OH Shikimate biosynthetic pathway of the gatrointestinal microflora COO- COO+ + H3 N C H CH2 synthesis of aromatic amino acids COOH H3 N C CH2 H COO + H3 N C CH2 C HC N H DNA repair antioxidation NAD + ATP synthesis inflammatory and immune responses Trp OH Phe Tyr H A) The metabolism of a CAE by enteric microbiota increases host DNA repair capacity, antioxidation, NAD/ATP synthesis and regulates inflammation and immune responses. B) Production of aromatic amino acids (Trp, Phe and Tyr) by the shikimate biosynthetic pathway of the gastrointestinal microflora. Abbreviations: NAD, nicotinamine adenine dinucleotide; ATP, adenosine triphosphate; 2Pi, two-inorganic phosphates; PEP, phosphoenolpyruvate; Trp, tryptophan; Phe, Phenylalanine; Tyr, tyrosine. CELLULAR REPAIR PROGRAM Green = cell borders marked by the F-actin molecule Blue and Red = DNA molecules coiled into polytene chromosomes Excessive noise exposure, certain medications and the aging process can all lead to progressive degeneration of a large portion of sensory neurons; however, a smaller population of sensory neurons consistently survive. We are pursuing the hypothesis that differences in survival capacity between neurons are dependent on the neurons’ ability to effectively mobilize a protective DNA damage response. Noise exposure and cancer chemotherapies can independently damage DNA within peripheral neurons leading to the loss of neural functions (e.g., hearing loss). We have shown that only a small population of peripheral neurons are able to defend themselves by mobilizing DNA repair pathways to repair damaged genes. However, the larger population of neurons do not express DNA repair proteins or fail to appropriately coordinate DNA repair pathways. We suspect that these neurons lack the repertoire necessary to effectively defend their genome beyond basal demands and are therefore a major mediator of sensory impairments. We are employing a range of molecular, epigenetic and pharmacologic strategies to increase the survival of neurons by improving their capacity to defend/repair their genome. This work is relevant to the development of biomedical approaches aimed at rescuing neurons from cell death processes. NEUROAUDIOLOGY PROGRAM The neuroaudiology research program is focused on delineating the underlying neural substrates that drive specific types of auditory dysfunctions, such as tinnitus. Tinnitus is the abnormal perception of a sound that has no external source. The sounds heard by tinnitus suffers can be a ringing, buzzing, chirping, roaring and/or a large variety of other types of sounds. The sound may be intermittent or constant and may localize to the right ear, left ear, either ears or neither ears but instead perceived in the head. The intensity of the tinnitus sound can be so loud that patients report interference with everyday listening. The effect of tinnitus can be so great that patients often contemplate suicide. Fifty million Americans suffer with tinnitus and it is the most prevalent service-connected disability among veterans (exceeding PTSD and TBI). The Veterans Administration (VA) spent over $1.1 billion in 2010 to compensate veterans for tinnitus and is projected to exceed $2.26 billion (ATA). Interestingly, public and private funding for research focused on tinnitus treatment is only $10 million (ATA). Our research is focused on an unorthodox line of thinking regarding the auditory system and tinnitus. For instance, we are pursuing the notion that some forms of neuronal dysfunctions that drive tinnitus may also lower the threshold of susceptibility and/or increase severity of other neuropathologic conditions. Supporting evidence for this notion comes from observations that 1) specific lesions to primary auditory neurons alter excitatory and inhibitory neural circuits in the brainstem and cortex. 2) Alterations to excitatory and inhibitory neural circuits in the brainstem and cortex are common to tinnitus and other neuropathologic conditions. BRAIN INJURY PROGRAM This research is a collaboration with the Wright-Patterson Air Force Base in Ohio. Epidemiologic evidence suggest an increased risk of auditory impairments among Air Force personnel exposed to Jet fuel. Therefore, the current work aims to determine whether jet fuel exposure affects the peripheral and/or central auditory nervous system as a necessary prerequisite to the development of novel biomedical therapies. The research has already led to several important results. First, we discovered that low level jet fuel exposure induced a central auditory dysfunction that manifested as impaired brainstem encoding of stimulus intensity. Second, this central auditory dysfunction was exacerbated by background noise exposure. Third, the brainstem impairment was dominant among neurons that are responsive to high levels of acoustic stimulation. These findings could represent important and major shifts in the theoretical framework that governs current understanding of jet fuel and/or noise induced ototoxicity. From a clinical perspective the results indicate that jet fuel+noise exposure have consequences to brainstem function that may be more wide-spread and insidious than what was previously known. Therefore, it is possible that a large population of military personnel who are suffering with the effects of jet fuel or jet fuel+noise exposure may be misidentified because they would exhibit normal auditory sensitivity (normal hearing thresholds) but harbor a "hidden" brainstem dysfunction. Such brainstem dysfunctions may be associated with a large variety of clinical conditions such as depression, anxiety, sleep disorders, post-traumatic stress, tinnitus (ringing in the ear), hyperacusis (hypersensitivity to sounds), diploacusis (miss perception of pitch) and impaired speech perception (in ability to understand speech sounds). Brain Injury Program (continued): 2f1 - f2 (dB SPL) 40 A B 30 R3 20 10 0 -10 R2 Control Noise Fuel Fuel+Noise Noise floor R1 Nerve fibers -20 2 4 8 16 32 64 f2 (kHz) C D Control Gain 1 µV 1 ms Fuel+Noise Brain Injury Program (continued): Panel A shows the pre-synaptic sensory function of a group of animals exposed to jet fuel+noise. In addition to this group (Fuel+Noise), there are groups that were exposed to only noise and only jet fuel. There is also a control group which was unexposed. Note that the presynaptic function between the groups are similar. Panel B is a representative photomicrograph which reveals that the pre-synaptic sensory cells and post-synaptic peripheral nerve fibers were undamaged by the exposures. Panels C & D, are brainstem recordings that illustrate that the jet fuel+noise exposures altered brain activity (p < 0.05). Taken together, the data suggest that exposure to jet fuel combined with background noise may preserve hearing sensitivity but impairs brain functions. All panels were taken from Guthrie et al., 2014, J Toxicol Environ Health A.,77,261-280. Data Presentations at Scientific Meetings Differential DNA Damage Response Among Auditory Sensory Neurons Following Ototrauma O'neil Guthrie Ph.D1,2, Terry Fleck MD2, Helen Xu MD1,2 Linda Veterans Affairs Hospital, 2Department of Otolaryngology – Head & Neck Surgery, School of Medicine, Loma Linda University Medical Center 1Loma A Introduction -15 2 4 8 16 f2 32 25 E 0.4 0.0 Noise XPA ** Control Noise 0.6 0.2 0.2 0.0 0.0 APEX MIDDLE APEX MIDDLE F BASE CSA * BASE A 5 APEX MIDDLE BASE 2 4 8 16 32 64 200 D E nuclear nucleoplasm 150 20 10 10 Control Noise 1.5 nuclear translocation Neurons/120 µm2 30 Control Noise 0 0.4 Control Noise 0.5 0.4 ** 0.0 Noise ** ** 0.4 ** * * * ** * 0.3 * 0.3 ** 0.3 0.2 0.2 0.2 0.1 0.1 0.1 Control 0.0 Noise 0.5 Control 0.0 Noise 0.5 0.4 ** Control middle Noise 0.5 * * 0.4 ** ** ** * ** * 0.4 * ** * ** 0.3 0.3 0.2 0.2 0.2 0.1 0.1 0.1 ** base Control 0.0 Noise Control 0.0 Noise Control Noise Figure 5. Spatial remodeling of subcellular distribution patterns. Neurons in the apical cochlear coil exhibited an increase in both nuclear and cytoplasmic retention of CSA which was accompanied by significant nuclear exclusion of XPA. Neurons in the middle coil of the cochlea exhibited significant nuclear exclusion of both CSA and XPA. These neurons also showed an increase in cytoplasmic retension of CSA coupled with a significant reduction of cytosplamic XPC. Neurons in the basal cochlear coil exhibited significant nuclear retention of XPC and reduction of cytoplasmic and nuclear XPA, [* = p < 0.05; ** = p < 0.01]. B A C γH2Ax 80 0 2 4 5 7 9 11 12 14 Distance (µm) 60 F 250 Apex Middle Base 1.5 control 150 100 50 nucleoplasm 0 2 4 5 7 Apex 9 11 12 14 Distance (µm) Middle Base 1.0 0.5 Middle 60 20 195 60 apex 20 0 80 D 40 210 225 240 255 0 195 80 E 60 210 225 240 255 240 255 F base middle 40 40 20 20 0 0 210 225 240 255 195 210 225 gray level Figure 7. Noise induced γ-H2Ax. (A) Photomicrograph of γ-H2Ax immunoreactivity within the spiral ganglia. (B) Enlargement of the area outlined in (A) showing dense nuclear reactions. Note the punctus reaction products that line the circumference of the nucleus. (C) Morphometric analysis of the reaction products with and without noise exposure. Note that the noise exposure induced an increase in γ-H2Ax (see arrows). Panel C is the overall frequency distribution of the density of the reaction products under control (dotted line) and noise (solid line) conditions. Panels D-F is the data for the three different cochlear coils. In panels C-F, the ordinate axis is the frequency of occurrence in percent and the abscissa is the measured gray level. The step tablet above panel C shows the direction of the gray levels where 0 = black (heavy staining) and 255 = white (no staining). Scale bar in panel A = 10 µm and panel B = 20 µm. XPA CSA 0.0 Conclusions Base Figure 2. Preservation of spiral ganglion neurons. (A) Representative photomicrograph of H&E stained spiral ganglion neurons. (B) The total number of neurons from the control or noise groups is not significantly different (p > 0.05) at 1-day post noise exposure. Furthermore, neuronal populations at the apical, middle and basal coils are similar (p > 0.05) between the control and noise groups (C). These combined data indicates that subsequent observations were not due to missing neurons. Noise Control 0.5 XPC Figure 5. Noise induced dys-synchrony. Under control conditions, spiral ganglion neurons exhibit a general response of the following order: Apex = XPA > CSA + XPC; Middle = XPA + CSA > XPC; Base = XPA + CSA > XPC. However, after noise stress the general response is characterized by: Apex = CSA > XPC > XPA; Middle = XPC > CSA + XPA; Base = XPC > CSA + XPA. Apex 80 C 40 200 noise 1.0 0.0 0 Control 0.5 50 0 C 20 0.0 Noise ** 100 0 (kHz) B 30 Control 0.5 0.0 apex ** 250 Figure 4. Representative example of subcellular distribution patterns. (A) Photomicrograph of a field of neurons exhibiting cytoplasmic expression. (B) Enlargement of the area outlined in (A) showing that reaction products were predominantly localized in the cytoplasm. (C) Representative 1-pixel wide linescan demonstrating that cytoplasmic reactive neurons exhibit a specific morphologic profile where chromogen intensity in the nucleoplasm (~4-10 µm) is minimal compared to the cytoplasm. The y-axis in panels C and F are inverted gray (g) level (1/g). (D) Photomicrograph of a field of neurons exhibiting nuclear expression. (E) Enlargement of the area outlined in (D) showing that reaction products were predominantly localized in the nucleus. (F) Representative 1-pixel wide linescan revealing that nuclear reactive neurons exhibit a specific morphological profile where chromogen intensity in the nucleoplasm (~4-10 µm) is maximal compared to the cytoplasm. 40 0.1 0.0 H&E 40 0.2 0.1 ** B cytoplasmic L1/L2 (65/55) f2 50 0.2 Linescan Profiles (kHz) 50 ** 0.1 0.0 ** ** 0.3 * 0.2 0.3 0.4 * Figure 1. Loss of cochlear function from the noise (8 kHz OBN @105 dB SPL /4 h) exposure. The levels of 2f 1-f2 DPOAE as a function of f2 frequency driven with primary levels (L) at 65/55 dB SPL are shown for both the control and noise treated groups. The gray bar in panel B represents the frequency bandwidth of the damaging noise. Note that the nose exposure induced a significant (p < 0.05) loss of sensitivity. The gray solid line in each panel is the noise floor. Error bars are standard errors of the means. A Proportion immunoreactive neurons Proportion reactive neurons Control -5 -25 64 XPC 0.2 0.0 15 -15 L1/L2 (65/55) 0.2 0.6 D 0.4 ** 0.3 * Frequency (%) 5 -5 0.6 Intensity (g-1) 2f1 - f2 (dB SPL) 15 -25 Control (n=12) Noise (n=11) Noise Floor 35 25 C * 0.4 * ** 0.3 negative control 0.4 CSA 0.5 * 0.4 ** * 0.6 XPA 0.5 Cytoplasmic Nuclear 0.4 Figure 3. Heterogeneity among spiral ganglion neurons. (A) No immunoreactivity for NER proteins are found in the spiral ganglia after the immunohistochemistry procedure with antibodies omitted. (B) A representative photomicrograph of a field of negative (arrows) and positive immunoreactive neurons and satellite cells (*), scale bars = 20 µm. (C) A small (~40%) cohort of neurons are immunoreactive under normal conditions and a similar cohort appears to be reactive following (1-day post) noise stress. (D) This noise stress did not cause a significant change in the proportion of neurons that are immunoreactive for XPC, however there was a reduction in the proportion of XPA reactive neurons at the middle and basal coils (E). Additionally, the proportion of CSA reactive neurons showed a significant reduction in the basal coil (F), [* = p < 0.05; ** = p < 0.01]. 1-day post-noise exposure 45 Control (n=12) Noise (n=11) Noise Floor 35 2f1 - f2 (dB SPL) B Baseline 45 XPC 0.5 * Intensity (g-1) A B * Noise exposure has been shown to precipitate free radical induced DNA damage products in the cochlea. Free radical DNA damage can result in mutated gene fragments that alter cellular functions and/or induce progressive cell death. The nucleotide excision repair (NER) pathway is particularly adapted to protecting both active and inactive genes through genetically distinct subpathways that require a Cockayne syndrome-A (CSA) E3-ubiquitin ligase complex (CSA/DDB1/Cullin-4A/ROC1/Rbx1/COP9) and the xeroderma pigmentosum-C (XPC) heterotrimeric (XPC/nHR23B/centrin2) preincision complex. The rate limiting factor in both pathways is the C4-type zinc-finger (Cys105X2-Cys108 -X17 -Cys126 -X2 -Cys129 ) scaffolding protein XPA, which positions and activates nucleases for excision of damaged gene fragments. Noise is known to induce progressive degeneration of spiral ganglion neurons, however a subpopulation of neurons consistently remain viable. This difference in viability might be mediated through NER. Therefore, it was posited that noise exposure would induce differential DNA damage responses among spiral ganglion neurons. Male Long-Evans rats were exposed to an 8 kHz octave band of noise at 105 dB SPL for 4 hours. Distortion product otoacoustic emissions were recorded before and after noise exposure and the animals were sacrificed via transcardial perfusion for temporal bone harvesting, immunohistochemistry and quantification of intracellular protein distribution. The results revealed that the majority (~60%) of spiral ganglion neurons do not express NER protein complexes as a defense against noise exposure which may help to explain selective neurodegeneration. However, under normal conditions a cohort of neurons (~40%) exhibited either cytoplasmic or nuclear localization of NER factors. After noise exposure the overall number of reactive neurons stayed the same but there was significant (p < 0.01) cytoplamic and nuclear redistribution of the various NER factors. This noise effects was accompanied by phosphorylation of histone H2Ax, indicating genomic stress. Translocation of NER factors from the cytoplasm to the nucleus was dependent on the location of neurons along the cochlear spiral. For instance, neurons at the apical coil exhibited significant (p < 0.01) nuclear translocation of the CSA complex while neurons at the basal coil revealed significant (p < 0.05) nuclear translocation of the XPC complex. This spatial difference in nuclear translocation between CSA and XPC complexes suggests a difference in genome defense repertoire between apical and basal spiral ganglion neurons. Furthermore, noise exposure depleted XPA from the nucleus regardless of location along the cochlear spiral. These findings provide a novel mechanism for interpreting noise induced primary neuropathy and provide a basis for noise induced mutagenesis. Acknowledgments This work was supported by a CDA-2 (C7600-W) Award from the Rehabilitation Research and Development Service of the Office of Research and Development United States Department of Veterans Affairs. The Loma Linda Veterans Affairs Hospital provided the facilities for conducting the experiments. NER is one of the most potent molecular mechanisms for determining resistance to cell death. The majority of spiral ganglion neurons do not express NER proteins with or without noise stress. This is significant because spiral ganglion neurons are hyper-susceptible to cell death from noise exposure, ototoxic xenobiotics and/or microbial infections. A small cohort of spiral ganglion neurons express NER proteins and mobilized these proteins in response to noise exposure. This is significant because in humans and animals a small proportion of spiral ganglion neurons persistently survive a wide variety of stressors. This capacity to survival may be driven by NER. DNA Repair Adjuvant Therapy Regenerates Neural Sensitivity When Administered After Noise Trauma 1Loma O’neil Guthrie 1,2, Jinwei Hu2, Helen Xu2 Linda Veterans Affairs Medical Center, 2Loma Linda University Medical Center Background Previous research has demonstrated the existence of an inducible DNA repair pathway within spiral ganglion neurons 1,2. After noise exposure or cisplatin intoxication, there is active transcription and intracellular translocation of DNA repair enzymes within a distinct population of neurons. Recent experiments have shown that carboxy alkyl esters (CAEs) that have been standardized to increase intracellular DNA repair can augment the capacity of spiral ganglion neurons to mobilize DNA repair enzymes 3. However, it is unclear whether such mobilization of DNA repair enzymes would restore neural sensitivity after trauma. Therefore in this study, we investigated whether or not adjuvant therapy with CAEs that begins after noise trauma could restore neural sensitivity. Methods Long-Evans rats were used as subjects and they were randomly divided into four experimental groups: vehicle-control, noise, CAE and noise+CAE. Hair cell and neural sensitivity were monitored with distortion product otoacoustic emissions (DPOAE) and auditory brainstem responses (ABR). Reference 1. Guthrie et al, Hear Res 239, 79-91, 2008; 2. Guthrie and Xu, Hear Res 294, 21-30, 2012; 3. Guthrie, Int J Neurosci 122, 757-766, 2001 Fig. 3A, The average ratio of click ABR thresholds at baseline and 1 day post-exposure. The control groups exhibited a ratio of ~1.0 which indicates that there were no differences in threshold between time points. Both the noise-only and the CAE+noise groups had a ratio of 0.4, indicating the acoustic overexposure induced similar loss of function. B. The average ratio of click ABR thresholds at 1 day and 1 week post-exposure. A ratio that is greater than 1.0 indicates that the threshold at 1 week has improved from that at baseline. C click ABR threshold shift at 1 month relative to baseline threshold for each experimental group. CAE+noise group exhibited greater recovery in ABR threshold than the noise-only group. Fig.1 DPOAE are robust within the time period of the study and elevated from the noise floor in the control and CAE treated rats. However, the acoustic overexposure depleted DPOAE levels into the noise floor and this depletion persisted over the duration of the study (1 month), which replicated in the noise+CAE group. N = 6-7 rats per group and the noise was a 5.6-11.3 kHz noise band @105 dB/4 hours. Fig. 4A DPOAE thresholds at 1 month after noise exposure. Thresholds for the noise groups (noise and CAE+noise) are similarly elevated above the control groups. 4B ABR thresholds at 1 month after noise exposure. The thresholds for the control groups are similar, there is a clear difference in thresholds between the noise and CAE+noise groups. The CAE+noise group has significantly better thresholds than that of the noise group. Fig. 2A Both noise groups (noise-only and the CAE+noise group) exhibited significant threshold elevations. 2B, ABR threshold shifts relative to the threshold of the control group. Note that the noise-only and the CAE+noise groups exhibited similar loss at 1 day post-noise exposure but the CAE+noise group showed better threshold recovery. Acknowledgements This work was supported by a CDA-2 (C7600-W) Award from the Rehabilitation Research and Development Service of the Office of Research and Development United States Department of Veterans Affairs. The Department of Otolaryngology and Head & Neck Surgery in the School of Medicine at Loma Linda University Medical Center also provided support. Conclusion 1. These results suggest that DNA repair adjuvant therapy may rescue neural functions when administered after injury. 2. This raises the possibility that treatment for NIHL may involve the use of hearing aids to address the permanent loss of audibility from OHC dysfunction combined with DNA repair therapy to preserve neural sensitivity. Neuronal Coupling of Cell Surface Receptor with DNA Repair Enzyme O’neil W. Guthrie1,2, Daniel Kwon2, Helen Xu2 1Research 2Department of Service-151, Loma Linda Veterans Affairs Medical Center, Loma Linda, CA 92357, USA. Otolaryngology and Head & Neck Surgery, School of Medicine, Loma Linda University Medical Center, Loma Linda, CA 92354, USA. Introduction Selected populations of spiral ganglion neurons have been shown to mobilize DNA repair enzymes1. We conducted experiments to determine whether or not such neurons express the epidermal growth factor receptor (EGFR). Gene and enzyme expression of the EGFR and the xeroderma pigmentosum-A (XPA) DNA repair factor were determined. Immunofluorescence assays were used to localize neurons expressing both EGFR and XPA. This work was then confirmed with double-immunohistochemical reactions. Rosenthals’ canal served as the reference space in these experiments and design-based stereology was employed. The results revealed that three populations of spiral ganglion neurons could be distinguished. For instance, there was a population that only expressed XPA and these neurons were predominantly clustered in the superior-medial quadrant of Rosenthal’s canal. There was a second population that only expressed the EGFR and these neurons were predominantly distributed throughout the inferior and superior-lateral quadrants of Rosenthal’s canal. The third and most abundant population, were neurons that expressed both the EGFR and the XPA enzyme. These neurons were distributed throughout the four quadrants of Rosenthal’s canal. The combined results provide the basis for future experiments designed to manipulate the EGFR in order to regulate DNA repair capacity and regenerate gene function after DNA damage. G I Fig I: Qualitative model of the data, showing distribution of the three population of neurons. Note the even distribution of neurons co-expressing EGFR and XPA. Conclusion Fig A, B: PCR and Western blot showing expression of both EGFR and XPA. Fig G: The 4 quadrants of Rosenthal’s canal and the corresponding stereologic quantification of EGFR and XPA; SM = superior medial; SL = superior lateral; IM = inferior medial and IL = inferior lateral H Subjects and Methods Six Long-Evans rats served as subjects in this study. Gene expression was measured with end-point polymerase chain reaction assays and related enzyme expression was measured with Western blots. After temporal bone harvesting, immunofluorescence confirmed by immunohistochemistry was used to localize expression of the EGFR and XPA enzyme. Design-based stereology employing the physical dissector approach was used for quantification of firstorder stereologic parameters. Fig C-F: Immunofluorescence (C-E) and immunohistochemical reactions (F) showing the immunoreactivity of distinct populations of neurons. Fig H: Breakdown of the three neuronal populations in each quadrant. Neurons are terminally differentiated cells and are known to have poor DNA repair defenses2. Cochlear neurons easily die after noise stress or injury from ototoxic exposure and with aging3 which might relate to the lack of DNA repair enzymes seen in these neurons1. However previous research has discovered a small population of cochlear neurons that express DNA repair enzymes1. This population of neurons may be more protected compared to the larger population of cochlear neurons. The current study further characterized this population of neurons by revealing that they express both EGFR as well as DNA repair enzymes which is a signature finding in cells that are resistant to cell death (i.e. cancer cells). This finding is a basis for future studies into the survival capacity of spiral ganglion neurons. References: 1. Guthrie and Xu. Noise exposure potentiates the subcellular distribution of nucleotide excision repair proteins within spiral ganglion neurons. Hearing Research. 294 (2012) 21e30 2. Nouspikel, T., Hanawalt, P.C., 2002. DNA repair in terminally differentiated cells. DNA Repair (Amst.) 1, 59e75. 3. Lin, H.W., Furman, A.C., Kujawa, S.G., Liberman, M.C., 2011. Primary neural degeneration in the Guinea pig cochlea after reversible noise-induced threshold shift. J. Assoc. Res. Otolaryngol. 12, 605e616. Subtoxic Levels of Jet Fuel Result in Abnormal Auditory Function O’neil W. Guthriea,b, Daniel Kwonb, Helen Xub, Pedro A. Ortizc, David R Mattie d aResearch Service-151, Loma Linda Veterans Affairs Medical Center, Loma Linda, CA of Otolaryngology-Head and Neck Surgery, Loma Linda University Medical Center, Loma Linda, CA cNaval Medical Research Unit - Dayton, Wright-Patterson, Air Force Base, OH. dMolecular Bioeffects Branch, Bioeffects Division, 711 Human Performance Wing, Human Effectiveness Directorate, Air Force Research Laboratory (711 HPW/RHDJ), Wright Patterson AFB, OH. bDept. Introduction Individuals who work within and around aircrafts are at risk for developing hearing loss. This is supported by studies that demonstrated that pilots, aircrew, aircraft technicians and mechanics have high (32-47%) prevalence rates of hearing loss when compared to the general adult population (15-20%). It is accepted that noise over-exposure is a prominent factor in the development of the hearing loss. In addition, preliminary epidemiologic analyses on aircraft maintenance personnel concluded that jet propulsion fuels (JP-8 or JP-4) may interact with noise to further induce hearing loss. Recent animal studies support this conclusion by revealing that exposure to JP-8 combined with noise may result in the loss of pre-neural cochlear sensitivity as well as loss of cochlear hair cells. This study investigated whether or not sub-ototoxic exposure to fuel, combined with a non-damaging dose of noise could interact to induce auditory impairment [Support for this research was obtained from the U.S. Air Force Surgeon General (SG5I) and managed through 711 HPW/RHDJ, Henry Jackson Foundation Subjects and Methods for Military Medicine, Loma Linda VA Medical Center, and Navy work unit number Eighty pigmented Long-Evans rats served as subjects in 61062]. the present study. Baseline screening of disortion product otoacoustic emission (DPOAE) levels was conducted on each animal to ensure normal DPOAE levels as determined by normative values publisehd by our laboratory. Animals were then randomized into 4 experimental groups, where each group consisted of 10 males and 10 females. There was a control (n = 20), a noise-only (n = 20), a jet fuel-only (n = 20) and a jet fuel+noise group (n = 20). Jet fuel animals were exposed to sub-toxic JP-8 for 6 hours per day, five days per week for four weeks. Noise exposure animals were exposed to non-damaging levels (85 dB) of noise for 6 hours per day, five days per week for four weeks. DPOAE, Auditory Brainstem Response (ABR) and Cytocochleograms were conducted on all rats. Statistical analyses were conducted with Prism 5, version 5.03 (GraphPad Software, Inc., La Jolla, CA. USA). ABR click thresholds were treated with one factor analysis of variance (ANOVA). The DPOAE, threshold shift, rate-level and gain-level data were treated with a split-plot ANOVA followed by Bonferroni pair-wise contrasts and Dunnett's post hoc testing. F-tests wereResults conducted to determine differences between slopes. Peripheral pre-neural function: DPOAE and cytocochloegrams revealed that fuel and noise exposures did not induce a pre-neural impairment. The sensitivity of the outer hair cells from the noise, fuel and fuel+noise groups is similar to that of control . Almost all outer hair cells, as well as inner hair cells and innervating nerve fibers were present (Fig.1). Peripheral neural function: Analysis of auditory electrophysiologic recordings revealed no detectable peripheral nerve impairment (wave I). There was no significant differences in click thresholds between groups. This was confirmed with frequency specific threshold shift analysis (Fig 2). Brainstem response function: Auditory brainstem response analysis demonstrated central auditory dysfunction with fuel and fuel+noise exposures. Amplification of peripheral neurotransmission was disrupted by the noise exposure as demonstrated by abnormal morphologies of evoked response recordings in the brainstem component in the fuel+noise exposed rats (Fig 3). Also, the fuel and fuel+noise groups exhibited a blunted response in the normal linear growth function of simulus intensity versus evoked response rate, suggesting compromise of brainstem encoding of stimulus intensity TEMPLATE DESIGN © 2008 www.PosterPresentations.com Discussion Individual noise and jet fuel exposure dosages used in the current study were deliberately chosen to be sub-ototoxic. This was done to determine whether or not subototoxic levels of each exposure could become ototoxic when combined (jet fuel+noise). The results revealed peripheral auditory function was not markedly effected but there was the presence of central auditory dysfunction. This indicates that central auditory processing dysfunction may be part of the ototoxic profile of jet fuel exposure. This line of thinking is supported by recent studies showing that military personnel exposed to jet fuel as well as gas station attendants demonstrate Central Auditory Processing Dysfunction (CAPD) such as poor auditory frequency discrimination and impaired ability to recognize speech in background listening situations despite normal hearing thresholds. From an epidemiologic perspective, the results imply that jet fuel exposure may have consequences to auditory function that could be more wide-spread and insidious than what was previously known. It is possible that a large population of military and civilian personnel who are suffering with the effects of jet fuel exposure may be misidentified because they might exhibit normal auditory sensitivity (normal hearing thresholds) but harbor a "hidden" brainstem dysfunction. Such brainstem dysfunctions may be associated with auditory and/or non-auditory symptoms. Therefore, the current study provides a basis for further research focused on jet fuel induced CAPD.. References Carrillo-de-la-Pena, M. T. 2001. One-year test-retest reliability of auditory evoked potentials (AEPs) to tones of increasing intensity. Psychophysiology 38:417-424 Fechter, L. D., J. W. Fisher, G. D. Chapman, V. P. Mokashi, P. A. Ortiz, J. E. Reboulet, J. E. Stubbs, A. M. Lear, S. M. McInturf, S. L. Prues, C. A. Gearhart, S. Fulton, and D. R. Mattie. 2012. Subchronic JP-8 jet fuel exposure enhances vulnerability to noise-induced hearing loss in rats. J Toxicol Environ Health A 75: 299-317. Fechter, L. D., C. A. Gearhart, and S. Fulton. 2010. Ototoxic potential of JP-8 and a Fischer-Tropsch synthetic jet fuel following subacute inhalation exposure in rats. Toxicol Sci 116 :239-248. Fechter, L. D., C. Gearhart, S. Fulton, J. Campbell, J. Fisher, K. Na, D. Cocker, A. Nelson-Miller, P. Moon, and B. Pouyatos. 2007. JP-8 jet fel can promote auditory impairment resulting from subsequent noise exposure in rats. Toxicol Sci 98 :510-525. Guest, M., M. Boggess, J. Attia, C. D'Este, A. Brown, R. Gibson, M. Tavener, I. Gardner, W. Harrex, K. Horsley, and J. Ross. 2010. Hearing impairment in F-111 maintenance workers: The study of health outcomes in aircraft maintenance personnel (SHOAMP) general health and medical study. Am J Ind Med 53:1159-1169 Kaufman, L. R., G. K. LeMasters, D. M. Olsen, and P. Succop. 2005. Effects of concurrent noise and jet fuel loss. exposure on hearing J Occup Environ Med 47:212-218. Quevedo, S., Tochetto, T., Siqueira, M.A., Machado, M.S. 2012. Auditory brainstem response in gas station attendants. Braz J Otorhinolaryngol 78:63-68. Genetic/transgenic conditional expression of nonmuscle myosin-II in auditory neurons: Head domain regulates assembly of the α-helical coiled-coil tail 1Loma O’neil Guthrie 1,2, Jinwei Hu2, Helen Xu2 Linda Veterans Affairs Medical Center, 2Loma Linda University Medical Center Background Nonmuscle myosin-II (MyoII) is an actin-binding protein that is involved in several motor functions including growth cone motility and neural migration, outgrowth and retraction. The molecule can be functionally divided into a head-domain and a α-helical coiled-coil tail. Self-assembly of the MyoII αhelical coiled-coil tail with other MyoII molecules form bipolar filaments that power cell movements. This selfassembly of the tail is intrinsically regulated by intramolecular interactions of the tail with the head-domain as demonstrated by in vitro experiments1. However, there is no in vivo evidence for this regulatory mechanism. Methods In this study, we further define whether the head-domain of MyoII regulates in vivo self-assembly of the α-helical coiledcoil tail in auditory neurons. A GAL4-UAS gene expression system was used to selectively express zip/MyoII fulllength, zip/MyoII tail with and without isoleucine-glutamine (IQ) motifs in Drosophila melanogaster auditory (Johnston’s organ) sensory neurons. The N-terminus of each construct was fused to green fluorescent protein (GFP) to follow the distributions of transgene expression. Figure 1. Sound evoked neural responses. The MyoII molecule was cloned and the head domain was removed to generate a headless (MyoII-tail) protein that harbors only the tail. This construct was genetically targeted to neurons, particularly auditory neurons. Note that conditional expression of the MyoII-tail showed reduced auditory nerve activity which suggest a potential hearing loss . Figure 2. Elav-GAL4 drives Elav-GFP expression in the auditory neurons of Johnston’s organ. Panel A shows a field of DAPI stained (blue) DNA from cells in Johnston’s organ. DNA from both neuronal and non-neuronal cells is stained. The neuron specific Elav promoter was used to drive GAL4 transcriptional regulation of UAS-GFP-elav (Panel A') in auditory neurons of Johnston’s organ. Panel A'' is a merger of panels A and A'. Panel A''' reveals the location of the neurons relative to the F-actin enriched (phalloidin stained) scolopale rods (red). Figure 3. Full-length zip/MyoII may exhibit rod or globular conformations in auditory neurons of Johnston’s organ. Panels A- A' reveals major sensory structures such as the actin enriched scolopale rods (red) and bipolar auditory neurons (green). The neuron specific Elav promoter was used to drive GAL4 transcriptional regulation of full-length UASGFP-zip/MyoII. Panels A''- A''' are enlarged from panel A and they reveal the two dominant conformations of GFP-zip/MyoII in the neurons. Note that zip/MyoII may assemble as rods (panel A'') or globular oligomers (panel A''' ). Figure 5. The tail domain of zip/MyoII assembles as rods in sensory neurons from living whole-mount preparations of Johnston’s organ. Panels A-A''' are optical sections through living tissue. The neuron specific Elav promoter was used to drive GAL4 transcriptional regulation of UAS-GFPzip/MyoII-tail domain in sensory neurons of Johnston’s organ. Panel A'''' is a Z-stack of the entire neuronal tissue of Johston’s organ. Figure 6. The tail+IQ domain of zip/MyoII diffuses throughout the cytoplasm of neuronal cell bodies and axons from fixed and living wholemount preparations of Johnston’s organ. Panels A-A''' shows neuronal expression of the tail+IQ domain in neurons from fixed whole-mount preparations of Johnston’s organ. The neuron specific Elav promoter was used to drive GAL4 transcriptional regulation of UAS-GFP-zip/MyoII-tail+IQ domain. Panels B-B' are 3 µm optical sections through living tissue. Figure 4. The tail domain of zip/MyoII assembles as rods in sensory neurons of Johnston’s organ. Panel A shows neuronal expression of the tail domain. The neuron specific Elav promoter was used to drive GAL4 transcriptional regulation of UAS-GFP-zip/MyoII-tail domain in sensory neurons of Johnston’s organ. Panel A' reveals dendrites projecting into the actin enriched (phalloidin stained red) scolopale rods. Panels A''- A''' are enlarged from panels A and A'. Note the elongated conformation of the tail domain. Scale bar =5 µm. Conclusion 1. Head-domain is critical for modulating the selfassembly of the tail in vivo. 2. These findings may help to explain why human mutations in the head domain result in severe diseased phenotypes. Reference: 1. Jung H.S, et al . Proc Natl Acad Sci U S A, 2008, 105: 6022-6026. Remodeling the intracellular distribution of DNA repair enzymes in spiral ganglion neurons in response to noise stress and otoprotective therapy 1Loma O’neil Guthrie 1,2, Jinwei Hu2, Helen Xu2 Linda Veterans Affairs Medical Center, 2Loma Linda University Medical Center Background Intracellular stress gradients drive the spatial distribution of DNA repair enzymes 1,2. In this study, we investigated if spiral ganglion neurons could remodel intracellular distributions of DNA repair enzymes in response to stress and otoprotective therapy. Methods The intracellular locations of DNA excision repair enzymes were determined within spiral ganglion neurons under normal conditions, after noise exposure, and following otoprotective treatment with carboxy alkyl esters (CAEs). Line scans were used to record immunoreactivity within the soma of each neuron to objectively profile the subcellular distribution of the enzymes. Figure 1. Positive and negative controls. (A) positive control cells. (BD) negative control. Scales bar=10 µm. Figure 3. Allocation of repair proteins across subcellular compartments from the control group. Each subcellular compartment is enriched with at least one repair protein. The XPC protein is predominantly localized in the cytoplasm while XPA is primarily diffused throughout the cytoplasm and nucleus. Additionally, the CSA protein exhibits a preference for cytoplasmic and perinuclear loci. Figure 7. The effect of the experimental conditions on the distribution patterns. The experimental conditions did not significantly change the distribution patterns for the XPC protein. However, there were significant changes for the XPA and CSA proteins. The experimental conditions were control (N = 5), noise (N = 5), CAE (N = 3) and CAE+noise (N = 3). Each plot displays the mean ± SEM. Figure 4. Re-allocation of repair proteins to the cytoplasmic compartment from the noise exposed group. Note that all the proteins exhibited preferential localization in the cytoplasm. Figure 8. Neuronal threshold shifts. Compound action potentials were recorded from each group at 4 weeks after the noise exposure. Note that the CAE treatment was neuroprotective. Figure 5. Allocation of repair proteins across subcellular compartments from the CAE treated group. The CAE treatment apparently equalized the distribution of the proteins across patterns. Statistical analyses reveal that no one localization pattern is significantly different than the other patterns for a given protein. Conclusion 1. The current study revealed that spiral ganglion neurons exhibit multiple compartmentalizing modes for excision repair enzymes and these modes exhibit plasticity following noise stress and otoprotective treatment. 2. Regulation of intracellular gradients of DNA excision repair enzymes may represent a novel approach to preserving neural function following stress. Reference 1.Griffiths LM, et al . Mol Cell Biol. 2009;29:794-807. 2.Guthrie OW..Anticancer Res. 2008;2637-2640. Figure 2. Representative examples of the intracellular distribution patterns of Neurons. (A-C) Diffuse expression. (D-F) Cytoplasmic expression. (G-I) Both nuclear and diffuse expression. (J-L) Perinuclear expression. The y-axis in panels C, F, I and L are inverted gray (g) levels (1/g). The scale bar (20 µm) in panel A applied to panels D, G and J. The scale bar (10 µm) in panel B applied to panels E, H, and K. Figure 6. Mixed allocation of repair proteins across subcellular compartments from the CAE+noise treated group. CAE+noise equalized the intracellular distribution of the XPC and XPA proteins. Statistical analyses reveal that no one localization pattern is significantly different than the other patterns. However, the CSA protein exhibited a preference for cytoplasmic and perinuclear loci. Acknowledgements This work was supported by a CDA-2 (C7600-W) Award from the Rehabilitation Research and Development Service of the Office of Research and Development United States Department of Veterans Affairs. The Department of Otolaryngology and Head & Neck Surgery in the School of Medicine at Loma Linda University Medical Center also provided support. The α-Helical Coiled-Coil Tail of Nonmuscle Myosin-II Mediate Interactions with the Nucleus O'neil Guthrie Ph.D1,2, Terry Fleck MD2, Helen Xu MD1,2 1Loma Linda Veterans Affairs Hospital, 2Department of Otolaryngology – Head & Neck Surgery, School of Medicine, Loma Linda University Medical Center A B C A B C Introduction Human genetic mutations (MYH9 and MYH14 related diseases) that affect the nonmuscle myosin-II (MyoII) molecular motor result in syndromic and nonsyndromic forms of sensorineural hearing loss but the underlying mechanisms are unresolved. We posit that one potential mechanism to account for MYH9/14 related diseases (e.g., hereditary macrothrombocytopenias) might be the interaction between MyoII and the cell nucleus. As a first approximation, we conducted genetic/transgenic conditional expression experiments to determine whether or not MyoII associates with the nucleus of cells in metazoan tissue. The giant cells within salivary gland organs from 3rd instar Drosophila melanogaster larvae were evaluated in living and fixed preparations. A UAS-Gal4 conditional expression system was used to drive gene expression of MyoII specifically within salivary gland organs. A GFP-MyoII protein trap line, which uses the endogenous MyoII promoter to control expression of full-length GFP-MyoII was also employed. Additionally, epitope immunoreactivity was used to localize endogenous MyoII proteins. The combined results demonstrate that the MyoII molecule may interact with the nucleus. For instance, the molecule formed oligomerized (filament-like) conformations on the cytoplasmic side of the nuclear lamin. The α-helical coiled-coil tail of the MyoII molecule was necessary and sufficient to mediate all nuclear interactions including perinuclear localization and oligomerization. These interactions affected the morphology of the nucleus and the nuclear associations of filamentous actin and actin-binding proteins. The data provide direct evidence for a nuclear association of MyoII within metazoan tissue and suggest that the interaction between MyoII and the nucleus might contribute to MYH9/14 related diseases. head domain α-helical coiled-coil tail domain Wild-type full-length ELC G A A1 B B1 DNA Lamin zip/MyoII D E F D G G' G'' G E F G' DNA 0 μm 3 μm 6 μm Figure 3. Oligomerized perinuclear pools zip/MyoII in a whole-mount salivary gland organ. In all panels green is GFP-zip/MyoII, red or blue is DNA and the cell junction protein, moesin is in white. Panel A is a Z-section through a whole-mount salivary gland. Panels B-F are stacked Z-sections. Panels B-C provides a 3D view of zip/MyoII and DNA. Panels D-F reveal the spatial orientation of DNA and/or GFPzip/MyoII within the salivary gland in general and specific cells in particular. Panels G-G'' are 0-6 μm sections through the nucleus outlined in panel A. Figure 4. zip/MyoII exhibits cytoplasmic perinuclear localization. Panels A-F are serial Z-zections through a single nucleus. Note that GFP-zip/MyoII is localized on the cytoplasmic side of the nuclear lamin (red). Panels G-G' are 3D reconstructions of panels B-F. Scale bar (10 µm) in panel C applies to all panels. A RLC B Figure 7. Perinuclear zip/MyoII co-localize with some actin-binding proteins. Panel A shows that spectrin (red, antibody stain) is localized around the nucleus of salivary gland cells. Panel A1 shows the same salivary gland with co-localization of spectrin (red) and GFP-zip/MyoII. Note that the yellow loci are areas of strong co-localization. Panel B shows that moesin (red, antibody stain) is localized at the periphery of the salivary gland. Panel B1 shows no colocalization between GFP-zip/MyoII and moesin. C A B neck + tail tail GFP-Tail fragment Figure 1. Schematic molecular structure of MyoII. MyoII consists of a hexameric holo-complex of two myosin heavy chains and two pairs of light chains. The N-terminal of the heavy chain comprises the MyoII head and consists of an SH3 domain and the motor domain which is the chemomechanical force producer and exhibits both ATPase and actin binding activities. The C-terminal of the head (called the neck domain) consists of an extended α-helix with isoleucine-glutamine or IQ motifs that bind to an essential light chain (ELC) and regulatory light chain (RLC). Both light chains (LC) stabilize the IQ motifs of the neck and stiffen the lever arm during force generation. The tail structure functions to dimerize the heavy chains through the formation of an α-helical coiled-coil and also includes a short, C-terminal non-helical tail piece. A A' GFP-Head+neck fragment GFP-Neck+tail fragment Figure 5. zip/MyoII tail domain regulates the assembly of perinuclear oligomers. Panels A-C are photomicrographs of living whole-mount salivary gland organs. Note that perinuclear oligomers are observed with expression of the tail and neck+tail domains and not the head+neck domain. neck+tail DAPI lamin C A D B A'' tail actin GFP-zip/MyoII DNA DAPI B zip/MyoII antibody staining B' B'' zip/MyoII protein trap DAPI C merge C' C D Conclusion merge C'' merge Figure 6. zip/MyoII co-localize with perinuclear actin. Panel A is phalloidin stained actin in whole mount salivary gland. The arrow reveals projections from both perinuclear and cell border actin pools. Panel B is the same salivary gland showing perinuclear localization of GFP-zip/MyoII. Panel C is the merger of panels A and B. Note that the yellow loci reveal strong perinuclear co-localization. Panel D is the Z-stack profile of the organ. DAPI zip/MyoII driven by Gal 4 merge Figure 2. Perinuclear localization of endogenous and transgenic zip/MyoII in single cells from whole-mount salivary gland organs. Endogenous (antibody stained) zip/MyoII (panels A-A") exhibit a prominent perinuclear localization. However, GFP-zip/MyoII protein trap (panels B-B") exhibit a modest perinuclear localization. Overexpression of GFP-zip/MyoII with the salivary gland specific Gal4 driver (panels C-C") result in prominent perinuclear localization. Arrows point to the perinuclear clusters of zip/MyoII. Figure 8. Headless myosin-II molecules may affect the morphology of the nucleus. Panel A-B shows that the morphology of the nucleus is maintained when the neck is attached to the tail. However, panels C-D reveals that removing the neck alters the morphology of the nucleus. The inset in panel D shows the percent of nuclei with altered morphology as a function of the various MyoII transgenic constructs. Abbreviation: F, full-length; H, head; N+T, neck+tail; T, tail. Acknowledgments The authors would like to thank Professor Dan Kiehart for helpful comments and support. The lamin Dm0(ADL67.10) monoclonal antibody developed by Paul A. Fisher was obtained from the Developmental Studies Hybridoma Bank and developed under the auspices of the NICHD and maintained by the University of Iowa, Department of Biology, Iowa City, IA 52242. The work was supported by the Hargitt Cell Biology Research Award. Previous cell culture observations were further bolstered in this study in which we clearly revealed perinuclear pools of MyoII in living and fixed preparations of Drosophila salivary gland organs. MyoII in cooperation with filamentous actin is known to generate force at the nucleus during disperate conditions such as mitosis, cellular locomotion and cell lineage determination. In this study MyoII affected the morphology of the nucleus and the nuclear associations of filamentous actin and actin-binding proteins. The data provide direct evidence for a nuclear association of MyoII within metazoan tissue and suggest that the interaction between MyoII and the nucleus might contribute to MYH9/14 related diseases. AUTOMETALLOGRAPHICAL AMPLIFICATION OF INTRACELLULAR ANTI-CANCER PLATINUM MOLECULES O’neil W. Guthrie1, Carey Balaban2 Science and Disorders, University of Pittsburgh, Forbes Tower, Pittsburgh, PA, United States, 2Otolaryngology and Neurobiology, University of Pittsburgh, 203 Lothrop, Pittsburgh, PA, United States 1,2Communication ABSTRACT METHODS This study utilized autometallography (Danscher et at, Neuroscience 105, 941947, 2001) to localize platinum in tissue. Platinum molecules from the drug cisplatin were amplified by reducing silver ions to silver atoms while chelating platinum bound to intracellular ligands. This redox activity allowed for detection of platinum embedded in black silver deposits at the light microscopy level. Kidneys were harvested from a Sprague-Dawley rat that was treated with 13 mg/kg of cisplatin i.p., euthanized 24 hours later and perfused transcardially with formalin. Control kidneys were harvested from an untreated, formalin-perfused SpragueDawley rat. Both control and experimental tissues were post-fixed with 10% buffered formalin and cryoprotected in PBS + 30% sucrose. Sections were then rinsed in Na acetate buffer before being immersed in a physical developer (AgNO3, Na acetate trihydrate, glacial acetic acid, cetylpyridinium Cl, Triton X-100, Na tungstate and Ascorbic acid). Silver deposits were fixed in potassium thiosulfate and sections were dehydrated and cover slipped. Autometallography silver deposits were observed in the nuclei of the proximal tubule cells of the kidney from the rat receiving systemic treatment of cisplatin. In vitro exposure of kidney tissues to 5 mM of cisplatin for 1 hour, by contrast, resulted in heavy staining of the renal cortex and less staining in the renal medulla. These findings suggest that autometallography may be a useful method for studying cisplatin uptake and distribution at the cellular level. [Supported by NIH-NIDCD (F31) DC05757-01 and the Eye & Ear Institute Foundation. The authors wish to thank Dr. Richard Salvi for providing tissue treated in vitro and Dr. Len Rybak for providing the in vivo treated materials.] Kidneys were harvested from a Sprague-Dawley rat that was treated with 13 mg/kg of cisplatin i.p., euthanized 24 hours later and perfused transcardially with formalin. Control kidneys were harvested from an untreated, formalin-perfused Sprague-Dawley rat. Both control and experimental tissues were post-fixed with 10% buffered formalin. Both tissues were sulfidated in 1% (NH4)2S in 70% ethanol, pH 9, at 22 C for 15 min. The tissues were then treated with 10% formic acid for seven days at 22° C and neutralized with 5% Na2SO4 for 24 hours at 22° C and then cryoprotected in PBS + 30% sucrose. Frozen sections of both tissues were cut on a sliding microtome (Microm HM440E) at 20 mm. The tissue sections were then ready for autometallography (see table 1 for autometallographic solutions). INTRODUCTION Cisplatin is an effective, widely used, broad-spectrum anticancer xenobiotic (Gordon & Hollander, 1993; Weiss & Christian, 1993). Its dose-limiting side effects are nephrotoxicity and ototoxicity. Therefore, knowledge of the cellular and subcellular binding sites of cisplatin is necessary to elucidate loci of toxic effects as well as aid in designing targeted prophylactic approaches. Thus, there is a need to develop sensitive techniques to identify trace amounts of the drug in the kidney and the cochlea. When cisplatin (cis-diamminedichloroplatinum II, (NH3)2PtCl2) enters a cell the dichloride ligands are dispelled, which renders the remaining platinum molecule highly reactive. This reactive platinum molecule acts as a potent electrophile, which reacts with nucleophilic ligands on nucleic acids (Kartalou & Essigmann, 2001). The approach in this study is based upon the observation that platinum bound to intracellular ligands may be chemically converted to a heterogeneous catalyst by reaction 1 (Zdolsek, 1993): Pt-ligand + S2- PtS + apo-ligand (1) This initial reaction facilitates the process of autometallography. Autometallography is the most sensitive cytochemical process for identifying the topographical distribution of catalytic metals in cells. Metallo-catalytic atoms or molecules within a cell may serve as a heterogeneous catalyst for the reduction of silver ions to metallic silver atoms. This redox activity leads to the identification of the catalytic metal, which allows for detection with electron and light microscopy. Autometallography has been used to identify endogenous trace metals such as, Cu2+, Fe2+, Zn2+, Co2+ and Ni2+ (Danscher, 1981). Additionally, nonessential and toxic metals such as, Hg2+, Cd2+, Pb2+, As2+, Bi2+, Tl2+, Au2+, and Ag2+ can be identified with autometallography (Danscher, 1981). In this study we have 2+ developed aAgsensitive platinum-sulfide autometallography (PtSAMG) procedure that 2+ allowed for Ag the detection and amplification of intracellular anti-cancer platinum Ag° moleculese in the nucleus of kidney cells (see 1. figure 1). Figure Principles of Autometallography: An - - Ag° Ag2+ PtS - ee- Ag° t1 Ag° eAg2+ - t2 Ag2+ Ag2+ + e2- Ago insoluble crystal lattice is formed from the electrovalent bonding of a metal (Pt) to a non-metal (S2-), which is able to conduct electrons (e-). An electrophile (Ag+) is reduced by a nucleophile (-) to form a metallic product (Ag°). This redox activity speeds up when both reagents come in contact with the metallic crystal lattice. The reagents chellates the initial crystal lattice, which generates a metallic shell of Ag° which grows with time, allowing for detection at the electron and light microscopy levels, t1= beginning time; t2= anytime post t1. RESULTS Panel A Table 1 Autometallography Chemicals Solution (sol.) C2H3O2Na.3H2O g *GAA AgNO3 C21H38NCl •TX Na2WO4.2H2O C6H8O6 K2S2O3 dH2O A 112.5 g B - 18.75 ml 2.75 g 1.0 g 2.5 ml 12.5 g 1872.5 ml 250 ml *GAA (Glacial Acetic Acid), •TX (Triton X-100) 2000 ml C - D - E - F 20 0.3 g 300 ml 20 ml 1980 ml 20 g 2000 ml - Panel B Panel C Black silver deposits show the localization of putative catalytic platinum molecules in the kidney. Panel A, is a photomicrograph at an intermediate depth within the renal cortex of a control kidney from a Sprague-Dawley rat. This section was processed with the autometallographic procedure. There are no black silver deposits. The same region of the kidney from a rat treated with cisplatin (13 mg/kg, i.p.) is shown in panels B and C. Note the prominent autometallographic black silver deposits in the nuclei of the proximal tubule cells and the lack of deposits within the renal corpuscle. This staining pattern was restricted to the middle third of the cortex. The nuclear localization is consistent with the known formation of cisplatin-DNA adducts (Kartalou & Essigmann, 2001). The localization of binding to proximal tubule cells in the middle third of the cortex suggests a selective affinity of these cells for cisplatin, which is consistent with the selective damage to proximal tubule cells after cisplatin treatment (Townsend, Deng, Zhang, Lapus & Hanigan, 2003). CONCLUSION We have presented a cytochemical approach to localize platinum molecules in cells. All chemicals were obtained from Sigma Chemical Company, St. Louis, MO. Autometallography may be a useful method for demonstrating cisplatin uptake and distribution at the cellular level. This method should be applicable to localize platinum in the inner ear. REFERENCES Autometallography Development Sequence } free floating sections sol. F 2 min } physical developer sol. A, B & C 1 or 4 min } Danscher, G. (1981). Histochemical demonstration of heavy metals: A revised version of the sulphide silver method suitable for both light and electron microscopy. Histochemistry 71, 1-16. } sol. D 10 min } sol. E 30 sec Gordon, M., & Hollander, S. (1993). Review of platinum anticancer compounds. Journal of Medicine, 24, 209-265. Kartalou, M., & Essigmann, J. M. (2001). Recognition of cisplatin adducts by cellular proteins. Mutation Research, 478, 1-21. Townsend, D. M., Deng, M., Zhang, L., Lapus, M. G., & Hanigan, M. H. (2003). Metabolism of cisplatin to a nephrotoxin in proximal tubule cells. Journal of the American Society of Nephrology, 14, 1-10. Autometallographic Technique for Visualizing Platinum in the Kidney Weiss, R. B., & Christian, M. C. (1993). New cisplatin analogues in development. Drugs, 46, 360377. Step 1: Kidney from an animal treated with cisplatin is sulfidated in vitro with (NH4)2S at pH 9 for 15 minutes. An insoluble platinum-sulfide reaction product is formed from the electrovalent bonding of platinum to sulfur, which is able to conduct electrons. Zdolsek, J. M., Roberg, K., & Brunk, U. T. (1993). Visualization of iron in cultured macrophages: A cytochemical light and electron microscopic study using autometallography. Free Radical Biology and Medicine, 15, 1-11. Step 2: Silver ions in solution A, are reduced by ascorbic acid (solution C) buffered by sodium tungstate (solution B) to form metallic silver. This redox activity speeds up when silver ions and ascorbic acid come in contact with tissue containing platinumsulfide reaction products (step 1). Silver ions once reduced by ascorbic acid chelates the initial platinum-sulfide reaction product, which generates black silver deposits. The silver deposits grow with incubation time, allowing for detection at the light microscopic level. ACKNOWLEDGEMENT This work was supported by NIH-NIDCD (F31) DC05757-01 and the Eye & Ear Institute Foundation. The authors wish to thank Dr. Len Rybak for providing the in vivo treated materials. The authors would also like to thank Drs. Catherine Palmer and John Durrant for helpful discussions regarding this project. Cisplatin Induces Cytoplamic to Nuclear Translocation of Nucleotide Excision Repair Factors Among a Proportion of Spiral Ganglion Neurons 1, Department O’neil W. Guthrie1, Carey Balaban2 of Biology, Developmental, Cell and Molecular Biology Group, Duke University, French Science Research Center, Durham, NC. 2, Otolaryngology and Neurobiology, University of Pittsburgh, 203 Lothrop, Pittsburgh, PA. INTRODUCTION Compared to other cell-types, neurons are poor at repairing damaged DNA among silent genes (global genome)[1]. The underlying mechanisms that result in poor neuronal repair of their global genome is unknown. Therefore, we evaluated the response of spiral ganglion neurons to sub-toxic cisplatin treatment cycles in order to better understand the mechanisms that underlie poor global genomic repair among neurons. Cisplatin is a potent anticancer drug that induces DNA damage in the cochlea among various cell types and human temporal bones reveal that cisplatin chemotherapy kills spiral ganglion neurons [2, 3]. Cancer research has revealed that cell survival from cisplatin chemotherapy is dependent on DNA nucleotide excision repair (NER) pathways [4]. One pathway is called global genomic-NER (GG-NER) and only repairs DNA damage among silent genes. The rate-limiting step in this pathway is DNA damage identification and verification by the proteins xeroderma pigmentosum complementation group C and A (XPC & XPA). The other pathway is called transcription coupled-NER (TC-NER) and only repairs DNA damage among active genes. The rate-limiting step in this pathway is accomplished by RNA polymerase II and XPA. Unlike RNA polymerase II, XPC and XPA have no known cellular function beyond DNA repair. Therefore, we suspected that cisplatin chemotherapy may stimulate the expression of XPC and XPA among spiral ganglion neurons. METHODS Sub-toxic cisplatin treatment cycles of 2 mg/kg, i.p., per day results in cisplatin DNA adducts among various cell types in the guinea pig cochlea [2] and stimulates antioxidant responses in the rat cochlea [5]. Therefore, we employed a 2 x 3 x 2 factorial design, consisting of two treatment conditions (cisplatin and saline treatment), three survival times (days 5, 19 and 22 of cisplatin treatment) and two analysis methods (quantitative RT-PCR and immunohistochemistry). The rats were treated with two cycles of cisplatin [5], each cycle consisting of four days of treatment (1 mg/kg, i.p., twice daily) separated by 10 days of rest. Each animal received daily hydration therapy consisting of 10 ml of saline administered subcutaneously. Survival times were 24 hours after each treatment cycle (days 5 and 19) and four days (recovery period) after the second treatment cycle (day 22). A total of 30 animals were treated with cisplatin, 10 were sacrificed at each of the three survival times for analyses. Another 30 animals received sterile physiological saline (vehicle) instead of cisplatin. Figure 4. XPC and XPA are expressed among cochlear hair cells with or without cisplatin treatment. A-B, are radial views of the organ of Corti showing XPC expression after cisplatin treatment (B) compared to saline treatment (A). C-D, are longitudinal views of the outer hair cells showing XPA expression after cisplatin treatment (D) compared to saline treatment (C). ihc, inner hair cell; ohc, outer hair cells, DC, Dieter’s cell; ip, inner pillar cells; op, outer pillar cells; sv, spiral vesicle. A-D are representative of all days sampled (days 5, 19 & 22), scale bars = 10 μm. Figure 5. Cisplatin treatment increases XPC and XPA immunoreactivity in the stria vascularis and spiral ligament. All cell types in the stria vascularis and spiral ligament seem to be immunoreactive after either saline (A, B, E, F) or cisplatin (C, D, G, H) treatment. Note that cisplatin treatment results in heavier immunoreactivity compared to saline treatment. B, D, F and H (scale bars = 10 μm) are enlargements of the outlined areas in A, C, E and G (scale bars = 50 μm) respectively. A-H are representative of all days sampled (days 5, 19 & 22). RM, Reissner’s membrane; Stv, stria vascularis; SLg, spiral ligament; O, osteocytes; SMC, strial marginal cells; SIC, strial intermediate cells; SBC, strial basal cells; I, type I fibrocytes; II, type II fibrocytes; III, type III fibrocytes. Figure 6. Cisplatin treatment increases XPA and XPC immunoreactivity in the spiral limbus. Spiral limbus fibrocytes (SLFs) and interdental cells (IDCs) exhibit light XPA (A-D) and XPC (E-F) immunoreactivity after saline treatment (A, B & E). SLF and IDC exhibit heavy XPA and XPC immunoreactivity after cisplatin treatment (C, D & F). No immunoreactivity is found in the negative control (G). RM, Reissner’s membrane; OC, organ of Corti; SL, spiral limbus; Stv, stria vascularis; SLg, spiral ligament. A-G are representative of all days sampled (days 5, 19 & 22). Scale bars A & C = 50 μm, scale bars for B, D, E & F = 10 μm and the scale bar for G = 100 μm. Figure 10. Cytoplasmic to nuclear translocation of XPA. XPC mRNA level x 10-9 140 cisplatin control A 120 100 80 60 40 20 0 180 saline Weight in grams 175 Saline Cisplatin 170 cisplatin Day 5 165 saline cisplatin Day 19 saline cisplatin Day 22 140 XPA mRNA level x 10-7 160 155 150 145 140 135 130 125 B 120 100 80 60 Figure 11. Total proportion of XPC and XPA immunoreactive ganglion cells. 40 20 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 0 saline Days cisplatin Day 5 saline cisplatin Day 19 saline cisplatin Day 22 Figure 1. Weight loss as a function of cisplatin treatment cycles. A 15 10 5 0 -5 Day 5 Day 19 Day 22 -10 OAE amplitude shift (dB) ABR threshold shift (dB) Figure 3. Cisplatin treatment increases cochlear XPC and XPA mRNA levels (2 ─∆Ct: y-axis). (A) XPC mRNA level for saline (n = 15) and cisplatin (n = 15) treated groups after days 5 (n = 5), 19 ( n = 5) and 22 (n = 5). (B) XPA mRNA level for saline (n = 15) and cisplatin (n = 15) treated groups after days 5 (n = 5), 19 (n = 5) and 22 (n = 5). Each bar represents mean ± SE for triplicate runs. 25 25 20 Figure 9. Cytoplasmic to nuclear translocation of XPC 20 B 15 10 5 0 -5 -10 -15 -15 4 8 16 1 2 3 4 5 6 7 8 Frequency (kHz) Figure 2. Cisplatin induced ABR threshold shifts and OAE amplitude shifts. Figure 8. Differential translocation of XPC (A-C) and XPA (D-F) among spiral ganglion neurons after cisplatin treatment. After the first treatment cycle (day 5) both XPC (A) and XPA (D) are localized in the nucleus of a proportion of spiral ganglion neurons (see arrows). After the second treatment cycle (day 19) XPA (E) remains localized in the nucleus while XPC (B) is now localized in the cytoplasm. After four days of recovery from the second treatment cycle (day 22) both XPC (C) and XPA (F) are predominantly localized in the cytoplasm. Interestingly, satellite cells (see arrow heads) are more immunnoreactive for XPA than for XPC and remained immunoreactive on all days sampled (D-F). Bars = 10 μm. Figure 7. Representative example of cytoplasmic to nuclear translocation among spiral ganglion neurons due to cisplatin treatment. (A) Negative control showing no immunoreactivity. (B) Enlarged area in (A) showing cell bodies of spiral ganglion neurons. (C) Schematic representation of a bipolar spiral ganglion neuron from (A). (D) XPC immunoreactivity is present under normal conditions (saline treatment) among some spiral ganglion neurons. (E) Enlarged area outlined in (D) showing predominant cytoplasmic localization of XPC. (F) Schematic representation of a bipolar spiral ganglion neuron from (E). (G) XPC immunoreactivity remained present after cisplatin treatment among spiral ganglion cells, except the immunoreactivity is now predominantly localized in the nucleus (H), which suggest translocation to the nucleus due to cisplatin treatment. (I) Schematic representation of a bipolar spiral ganglion neuron from (G). Scale bar (50 μm) in (A) applies to D and G as well. Scale bar (10 μm) in (B) applies to E and H as well. CONCLUSIONS: •Sub-toxic cisplatin treatment activates the NER cell survival pathway in the cochlea. •The time courses of nuclear translocation of XPC & XPA in spiral ganglion neurons vary along an apical to basal gradient. •Nuclear translocation of XPC occurs after the initial but not the second cisplatin treatment cycle in spiral ganglion cells. This finding suggests a global genomic NER response to only the first cycle of cisplatin exposure. •Nuclear translocation of XPA after both cycles of treatments suggests a transcription-coupled NER response to the second cycle of exposure. References: 1. Nouspikel, T. & Hanawalt, P. C. (2000). Molecular and Cellular Biology, 20, 1562-1570. 2. van Ruijven, M. W. M., de Groot, J. C. M. J., Hendriksen, F. & Smoorenburg, G. F. (2005). Hearing Research 203, 112-121. 3. Strauss, M., Towfighi, J., Lord, S., Lipton, A., Harvey, H. A., & Brown, B., (1983). Laryngoscope 93, 1554-1559. 4. Wu, X., Fan, W., Xu, S. & Zhou, Y. (2003) Clinical Cancer Research, 9, 5874-5879. 5. Minami, S. B., Sha, S. H. & Schacht, J. (2004). Hearing Research, 198, 137-143. Acknowledgements: NIH-NIDCD (F31), Eye and Ear Institute Foundation, Pennsylvania State K. Leroy Irvis Award, SHRS Research Development Fund Factors that Contribute To Tinnitus Distress in A Veteran Population Jinwei Hu, MD1; Jane Xu, BS1; Matthew Streelman, DDS2; Helen Xu, MD1; O’neil Guthrie, Ph.D1,3 1 Department of Otolaryngology-Head and Neck Surgery, Loma Linda University Medical Center, 2 Loma Linda University School of Medicine, 3Jerry L. Pettis VA Medical Center Objective: Neuronal dysfunctions that manifest as tinnitus are known to alter neuronal circuits in the brainstem and cortex, which are common to several comorbid conditions. This study is focused on the relations between tinnitus and anxiety/depression. Table 2A: Correlations between the degree of tinnitus and depression Pearson Correlation Significance (2-tailed) Total THI score * Depression 0.205 0.044 Study design: retrospective case review. Functional THI score * Depression 0.429 0.000 Setting: Veterans Affairs Medical Center (VAMC) Tinnitus Clinic. Emotional THI score * Depression 0.331 0.001 Catastrophic THI score * Depression 0.271 0.007 Patients: Ninety-one male veterans who reported subjective tinnitus were enrolled in a VAMC Tinnitus Clinic. Table 3: Tinnitus characteristics and duration Interventions: Case history, audiometric thresholds and selfassessment of tinnitus handicap were examined in all patients. Main outcome measures: Scores from the Tinnitus Handicap Inventory (THI) was used to assess tinnitus severity. ICD-9 codes for depression and anxiety were used to determine their prevalence among the patients. Pure tone averages (PTA) were used to assess hearing status. Table1: The median age, standard deviations, and age ranges of veterans with tinnitus with/without anxiety and depression (n=91). Age parameters Anxiety No anxiety Depression No depression Both Median 62.5 61 64 65 65 SD 10.04 11.40 10.18 11.76 10.18 Range 31-73 51-80 31-79 31-84 39-79 Figure 1. The mean PTAs (500, 1000, 2000Hz) showed no differences among the five groups or between ears (p > 0.05). The average hearing loss was around 38 dB HL among all the groups Figure 2: Tinnitus severity presented with total THI (A) and Functional (B), Emotional (C) and Catastrophic subscales (D) among tinnitus patients with and without anxiety and depression. Table 2A: Correlations between the degree of tinnitus and anxiety Pearson Correlation Significance (2-tailed) Total THI score * Anxiety 0.401 0.000 Functional THI score * Anxiety 0.474 0.000 Emotional THI score * Anxiety 0.473 0.000 Catastrophic THI score * Anxiety 0.279 0.006 Tinnitus characteristics x/n (%) Anxiety No anxiety Depression No depression Both Intermittent n=32 28/32 (87.5) 4/32 (12.5) 18/32 (56.2) 14/32 (43.7) 18/32 (56.2) Persistent n=47 37/47 (78.7) 10/47 (21.3) 31/47 (65.9) 16/47 (34.0) 30/47 (63.8) Bilateral n=71 59/71 (83.0) 12/71 (16.9) 46/71 (64.8) 25/71 (13.2) 45/71 (63.4) Unilateral n=6 6/6 (100.0) 0/6 (0) 3/6 (50.0) 3/6 (50.0) 3/6 (50.0) More than 10 years n=33 30/33 (90.9) 3/33 (9.0) 20/33 (60.6) 13/33 (39.4) 20/33 (60.6) Less than 10 years n=16 12/16 (75.0) 4/16 (25.0) 7/16 (43.7) 9/16 (56.2) 7/16 (43.7) Conclusions: The majority of patients with tinnitus exhibited a diagnosis of anxiety and depression. These patients suffer with more severe tinnitus than tinnitus patients without anxiety and depression. The data support the need for multidisciplinary intervention of veterans who suffer with tinnitus. Acknowledgements ?? The Department of Otolaryngology and Head & Neck Surgery in the School of Medicine at Loma Linda University Medical Center provided support. Regeneration of Pre-synaptic Sensory Functions May Not Restore Post-Synaptic Neurotransmission Eric Mendonsaa, Jinwei Hub, Helen Xub, O’neil W. Guthriea,b, aResearch Service-151, Loma Linda Veterans Affairs Medical Center, Loma Linda, CA 92357, USA. bDepartment of Otolaryngology and Head & Neck Surgery, School of Medicine, Loma Linda University Medical Center, Loma Linda, CA 92354, USA. Some instances of individual subject cochlear microphonics and summating potentials at low and high input stimuli show levels of sensory recovery 1 month after noise exposure. Rat 14 CMs and Rat 19 SPs displayed to the right. Subjects: Long-Evans rat model Treatment: An octave band of noise centered at 8 kHz at 105 dB SPL for 4 hours. Techniques: Pre-synaptic Distortion Product Otoacoustic Emission (DPOAE) Cochlear Microphonic (CM) Summating Potential (SP) Post-synaptic Auditory Brainstem Response (ABR) waves I-IV Measurements of pre and post synaptic cochlear functions were taken at baseline and 1 day, 1 week, and 1 month after noise exposure Experimental data illustrates a decoupling between pre-synaptic sensory function and post-synaptic neurotransmission after damaging levels of noise exposure. DPOAE responses from noise treated subjects exhibit detectable levels of sensory function recovery. A similar (although not as dramatic) effect can be observed in the pre-synaptic cochlear microphonic and summating potential data in which experimental subjects realize recovery at both low and high input stimuli. Post-synaptic neurotransmission, on the other hand, displayed a lack of recovery as illustrated by the negative trend from ABR waves I to IV. Overall, the data suggests that the restoration of pre-synaptic sensory functionality does not correlate with the degeneration of neural impulses from the peripheral to central nervous system. Consequently, further experimentation requires investigation of possible molecular mechanisms.