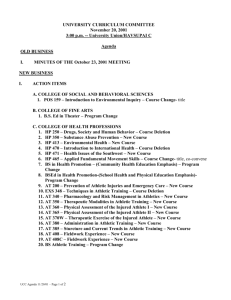
Introduction to Athletic Training
advertisement

Introduction to Athletic Training CORE CONCEPTS IN ATHLETIC TRAINING AND THERAPY SUSAN KAY HILLMAN Objectives Describe the education, training, and licensure and certification of the athletic trainer. Provide a general history of the athletic training profession. Identify the top three employment settings for athletic trainers in 2009. Identify various employment opportunities for athletic trainers. Describe five members of the sports medicine team and explain the general duties of each. Becoming an NATA Certified Athletic Trainer Training and Education Require at least 4 years of college education ATEP: Athletic Training Educational Program • Accredited school • Standards set by NATA • Housed under majors like Kinesiology • 350 + entry level ATEP programs Find on NATA website: CAATE-accredited athletic training programs 2 years of hands on practice Evaluation, prevention and management of athletic injuries Becoming an NATA Certified Athletic Trainer Certification Must satisfactorily complete undergraduate degree at accredited program See page 2 and 3 for courses required Take and pass a national certification exam Written, practical demonstration, and written simulation • Pass all 3 become an ATC, Certified Athletic Trainer • 80 CEU’s every 3 years to maintain certification • Adhere to NATABOC standards of professional practices Becoming an NATA Certified Athletic Trainer Licensure A.T. need to get licensed in some states Ensure legal practices of athletic training See figure I.1 California just denied licensure for athletic training Code of Ethics Written by athletic trainers in 1950’s Code of Ethics: www.nata.org Infractions may result in loss of certification Becoming an NATA Certified Athletic Trainer • Organization Each state represented within 1 of 10 NATA Districts: Figure I.2 Committees and subcommittees in each district Coordination of the organization from state to national level NATA provides money to state organizations for educational, research and licensure purposes History of Athletic Training Knowledge of history provides understanding of the AT profession Began with few athletic trainers across nation, mostly in college/university settings Current size of NATA more than 35,000 Clinics, schools, professional sports. Industry, health and fitness, and educational programs History of Athletic Training The 1930s and 1940s: Promoting the Exchange of Ideas Need for organization for AT Strain caused by WWII, but several accomplishments made The 1950s: Establishing the Organization 1947 AT began to grow, but AT had no formal education Skills learned from others in field 1950 first national meeting held and NATA established Considerable growth for NATA in 50’s Undergraduate programs established Constitution and By-Laws Official Logo Journal of AT established Code of ethics established History of Athletic Training The 1960s: Continuing the Growth 1969 American Medical Association recognized importance of AT The 1970s: Developing Standards for Certification Licensure debate began and each state responsible for own regulations The 1980s: Strengthening the NATA's Role Role delineation study to establish understanding of skills required for athletic trainers The 1990s: Becoming a Recognized Allied Health Profession Tremendous growth for NATA Official recognition of AT as allied health profession by AMA Monumental achievement Curriculum evaluation: creation of guidelines for schools to follow to ensure compliance for program accreditation AT moved from school and team environments to clinical and industrial settings History of Athletic Training SIDEBAR: Athletic Training Curriculum Model: Suggested Courses. Page 10 The New Millennium First female president of NATA Julie Max Internship route for ATS changed in 2004 Refine and develop competencies for which all AT are measured Redefine and structure clinical education Employment Opportunities in Athletic Training Athletic training Course Instructors University or College Athletic Trainers High School Athletics Trainers (Secondary Schools) Student Athletic Trainer Graduate School Opportunities Athletic Trainers/Coaches Clinic Athletic Trainers Athletic Trainers for Professional Sports Workplace Athletic Trainers Other Potential Opportunities The Sports Medicine Team The Athletic Training Team Physicians Orthopedic Surgeons and Other Specialists Rehabilitation Specialists Nutritionists Sport psychologists Paramedics and Emergency Medical Technicians Other Support Staff Coaches and Athletes The Sports Medicine Team Sports medicine refers to a broad field of medical practices related to physical activity and sport Defined by American College of Sports Medicine (ACSM) as multidisciplinary Includes physiological, biomechanical, psychological and pathological phenomena associated with exercise and sport Clinical application in these areas is aimed at improving and maintaining functional capacities for physical labor exercise and sports Sports medicines generally focuses on areas of performance enhancement, injury care, prevention and management The Sports Medicine Team Areas of specialization that focus primarily on performance enhancement Exercise physiology Biomechanics Sports psychology Sports nutrition Strength & conditioning Personal fitness training Coaching Physical education The Sports Medicine Team Areas of specialization that focus on health care and injury/illness management specific to the athlete Practice of medicine (physicians & physician assistants) Athletic training Sports physical therapy Massage therapy Dentistry Osteopathic medicine Sport podiatry Orthotist/prosthetists Sports chiropractic Role of Athletic Trainer Work with athletes from time of injury to resolution Directly responsible for all phases of health care in an athletic environment Role of Athletic Trainer Injury prevention Ensure appropriate training, monitor environment, nutrition, maintain & fitting equipment, appropriate use of medication Treatment, rehabilitation and Clinical evaluation and Organization & diagnosis Recognize nature and extent of injury Immediate care Provide first aid and management of acute injuries Minimum of CPR/AED and First Aid reconditioning Knowledge of equipment, manual therapy, therapeutic modalities administration Budgeting, inventory, injury records, supervision of assistants, insurance, EAP development Professional responsibility Educating the public through seminars, research & providing good care Relationship Between the Sports Medicine Team and Athlete Primary concern should be that of the athlete All individuals must work cooperatively in the best interest of the athlete Coach should differ to the medical staff and support decisions regarding athlete health care Close communication between all parties involved is critical Relationship Between the Sports Medicine Team and Athlete All parties must work to develop solid working relationship Each member will have to gain trust and confidence in the skills and abilities of each other Imperative that the athlete is kept well-informed Coach and athletic trainer must make a point of educating the student-athlete