hormones
advertisement

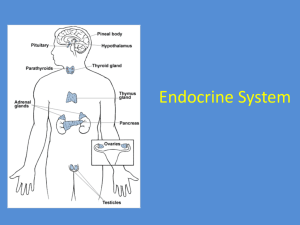
ENDOCRINE SYSTEM Dr. Othman Al-Shboul Department of Physiology & Biochemistry 1 College of Medicine OUTLINE Introduction to Endocrine System Pituitary Hormones – Growth Hormone Thyroid Hormones Adrenal Hormones Pancreatic Hormones Hormonal Regulation of Ca++ metabolism 2 INTRODUCTION TO ENDOCRINE SYSTEM 3 CLASSES OF CHEMICAL MESSENGERS Neurotransmitters: released by axon terminals of neurons into the synaptic junctions and act locally to control nerve cell functions. Endocrine hormones: released by glands or specialized cells into the circulating blood and influence the function of cells at another location. Neuroendocrine hormones: secreted by neurons into the circulating blood and influence the function of cells at another location in the body. Paracrines: secreted by cells into the extracellular fluid and affect neighboring cells of different type. Autocrines: secreted by cells into the extracellular fluid and affect the function of the same cells that produced them. 4 THE ENDOCRINE SYSTEM The endocrine system consists of the ductless glands and their hormones. The endocrine system regulates the internal milieu of an animal (homeostasis ). The “internal secretions” were liberated by one part of the body, traveled via the bloodstream to distant targets cells. Claude Bernard, Circa 1854 Target cells are specific for each hormone as these cells have receptors that uniquely bind to a specific chemical messenger 5 NERVOUS VS. ENDOCRINE SYSTEM 6 HORMONE LEVELS & TISSUE RESPONSES Priming effect (up regulation) o The cells of the body increase the number of receptors to a certain hormone (when there is low concentration of this hormone) o Results in greater response in target cell Desensitization (down regulation) o The cells of the body decrease the number of receptors to a certain hormone (when there is high concentration of this hormone) 7 o Results in weaker response in target cell CLASSES OF HORMONES i. Hydrophilic (peptide hormones and catecholamines) o o ii. Peptide hormones are chains of amino acids Include ADH, GH, insulin, oxytocin, glucagon, ACTH, PTH Catecholamines include norepinephrine & epinephrine Lipophilic (steroid hormones and thyroid hormone) o Steroid hormones are lipids derived from cholesterol Include testosterone, estrogen, progesterone, aldosterone and cortisol 8 CLASSES OF HORMONES i. Hydrophilic o o o Water soluble Surface membrane receptors Activate 2nd -messenger systems (cAMP, Ca++) Hydrophilic Hormone 9 2nd Messenger ADENYLATE CYCLASE-CAMP SYSTEM Hormone binds to receptor protein causing dissociation of subunit from Gprotein complex. G-protein subunit binds to and activates adenylate cyclase. ATP cAMP + PPi cAMP activates protein kinase. Protein kinase phosphorylates enzymes within the cell to produce hormone’s effects (activates or inhibits other enzymes). cAMP inactivated by phosphodiesterase. Protein Kinase A 10 CLASSES OF HORMONES ii. Lipophilic o o o Lipid soluble Cytoplasmic/nuclear receptors Affect gene transcription Lipophilic Hormone Gene Transcription 11 MECHANISM OF ACTION OF LIPOPHILIC HORMONES VIA ACTIVATION OF GENES 12 13 HORMONE PLASMA LEVELS Balance between: Rate of secretion & Rate of excretion 14 MECHANISMS CONTROLLING HORMONE SECRETION 1. Negative-feedback control 2. Neuroendocrine reflexes 3. Diurnal (circadian) rhythms 15 1. NEGATIVE-FEEDBACK CONTROL • After stimulus causes release of the hormone , the hormone (or its products) tends to suppress its further release. • To maintain the plasma concentration of a hormone at a given level. 16 2. NEUROENDOCRINE REFLEXES • Sensory stimulus (e.g., suckling) evokes a neural pathway that leads to secretion of a hormone Hypothalamus Pituitary Prolactin & Oxytocin To produce a sudden increase in hormone secretion Spinal cord 17 3. DIURNAL (CIRCADIAN) RHYTHMS Repetitive oscillations in hormone levels that are very regular and cycle once every 24 hours Example, cortisol secretion, high in the early morning and low at evening 18 HORMONE EXCRETION i. Hydrophilic hormones o o Dissolved in plasma, not bound to plasma proteins Rapidly eliminated from circulation, short half life. ii. Lipophilic hormones o Circulate in the blood mainly bound to plasma proteins. o Binding slows hormone clearance from plasma, long half life Half-life is the time required for blood level of a hormone to be reduced by half 19 PITUITARY HORMONES 20 THE PITUITARY GLAND (HYPOPHYSIS) Lies in sella turcica, a bony cavity at the base of the brain. Connected to the hypothalamus by the pituitary stalk (or infundibulum). The master gland Two Distinct Parts: * The Anterior lobe (adenohypophysis) * The Posterior lobe (neurohypophysis) 21 glandular epithelial tissue nervous tissue HYPOTHALAMIC-PITUITARY RELATIONSHIP Hypothalamus-anterior pituitary Hypothalamus-posterior pituitary vascular link neural link Factors (or hormones) released from hypothalamus reach anterior pituitary via circulation Axons from hypothalamus extend into posterior pituitary 22 I. POSTERIOR PITUITARY HORMONES 23 HYPOTHALAMUS & POSTERIOR PITUITARY Posterior pituitary gland does not synthesize hormones Posterior pituitary gland stores & releases hormones that are generated & secreted from hypothalamus 24 POSTERIOR PITUITARY HORMONES 1. VASOPRESSIN (antidiuretic hormone, ADH) 2. OXYTOCIN 25 VASOPRESSIN (ANTIDIURETIC HORMONE, ADH) It enhances the retention of H2O by the kidneys (an antidiuretic effect), more important It causes contraction of arteriolar smooth muscle (a vessel pressor effect, increasing resistance) 26 OXYTOCIN Stimulates contraction of the uterine smooth muscle to help expel the infant during childbirth Promotes ejection of the milk from the mammary glands (breasts) during breast-feeding Oxytocin is concerned with releasing or ejection of milk, while prolactin (from the anterior pituitary) is concerned with synthesis & production of milk. 27 II. ANTERIOR PITUITARY HORMONES 28 ANTERIOR PITUITARY HORMONES Many are tropic hormones Different cell populations within the anterior pituitary secrete six major peptide hormones: 1. Growth hormone (GH, somatotropin) 2. Thyroid-stimulating hormone (TSH, thyrotropin), stimulates the secretion and growth of the thyroid gland 3. Adrenocorticotropic hormone (ACTH, adrenocorticotropin), stimulates the growth and secretion of hormones from the adrenal cortex. 4. Follicle-stimulating hormone (FSH), stimulates growth and development of the ovarian follicles in females and sperm production in males. 5. Luteinizing hormone (LH), stimulates ovulation and luteinization (female) and stimulates testosterone secretion in the male. 6. Prolactin (PRL), enhances breast development in females, milk productipon 29 Functions of the anterior pituitary hormones 30 HYPOTHALAMIC HORMONES OR FACTORS Secretion by the anterior pituitary is controlled by hormones called hypothalamic releasing and hypothalamic inhibitory hormones (or factors) transported through hypothalamic-hypophysial portal vessels Hypothalamus receives signals from many sources in the nervous system & in turn controls the secretion the pituitary hormones 31 HYPOTHALAMIC-HYPOPHYSEAL PORTAL SYSTEM Venous blood flows directly from one capillary bed through a connecting vessel to another capillary bed (without passing through the heart). 32 GROWTH HORMONE (GH) 33 ACTIONS OF GH i. Metabolic actions ii. Growth-promoting actions on: Soft tissues Skeleton 34 ACTIONS OF GH i. Metabolic actions: Breakdown of triglyceride fat stored in adipose tissue increased blood f.a levels Decreases glucose uptake by muscles increases blood glucose levels Muscles use f.a for energy, reserving glucose for nervous tissue 35 ACTIONS OF GH ii. Growth-promoting actions on soft tissues Increasing the number of cells (hyperplasia) stimulating cell division preventing apoptosis Increasing the size of cells (hypertrophy) stimulates synthesis of proteins inhibits protein degradation promotes the uptake of amino acids by cells 36 ACTIONS OF GH Growth-promoting actions on skeleton (bone) iii. 1. 2. Growth in bone thickness (stimulates osteoblasts under periosteum) Growth in bone length (stimulates osteoblasts at epiphyseal plate) Hyaline cartilage in growing bone (before puberty) Plate/line (bone) in adults (after puberty) 37 SOMATOMEDINS Growth hormone exerts its growth-promoting effects indirectly by stimulating somatomedins. Somatomedins are referred to as insulin-like growth factors (IGF) The major source of circulating IGF is the liver IGF synthesis is stimulated by GH IGF is also produced locally by most other tissues. Growth 38 Increases after the onset of deep sleep CONTROL OF GH SECRETION Weak Strong 39 ABNORMAL GROWTH-HORMONE SECRETION GH Hyposecretion (deficiency) GH Hypersecretion (excess) 40 GROWTH HORMONE DEFICIENCY In childhood; results in dwarfism: In short stature poorly developed muscles (reduced muscle-protein synthesis) excess subcutaneous fat (less fat mobilization). adulthood; relatively few symptoms: reduced skeletal muscle mass and strength (less muscle protein) decreased bone density (less osteoblast activity during ongoing bone remodeling). 41 GROWTH HORMONE EXCESS In childhood before the epiphyseal plates close, gigantism : rapid growth in height without distortion of body proportions. After adolescence after epiphyseal plates close, acromegaly : person cannot grow taller, but the bones can become thicker (hands, feet, lower jaw…) and the soft tissues can continue to grow 42 THYROID HORMONES 43 STRUCTURE OF THE THYROID GLAND Formed of 2 lobes (Rt & Lt) in the neck just below the larynx, on either side of & anterior to the trachea. Composed of large numbers of closed follicles (the functional units) Follicles are filled with colloid (secretory substance) and lined with cuboidal epithelial cells (secrete into the interior of the follicles) The major constituent of colloid is thyroglobulin (glycoprotein containing the thyroid hormones) 44 THYROID HORMONES 1. Triiodothyronine (T3) 2. Tetraiodothyronine or thyroxine (T4) 3. Calcitonin Thyroid Hormone = Tyrosine + Iodine 45 THYROID HORMONES T3 & T4 50 milligrams of iodine are required each year for the formation of adequate quantities of thyroid hormone. Both are secreted from the Follicular cells Both can be stored in thyroid gland for couple of months Secretion: T4 >>> T3 Peripherally: most T4 is converted into T3 Activity: T3 >>> T4 46 SO, T3 is the major biologically active form of thyroid hormone at the cellular level, even though the thyroid gland secretes mostly T4. THYROID HORMONES Calcitonin Important for calcium metabolism reduces blood Ca2+ – increases Ca2+ deposition in bone Secreted from Parafollicular cells (or C-cells) 47 THYROID HORMONES EFFECTS (T3 & T4) Effect on metabolic rate and heat production: Increased metabolic activity (O2 consumption) Increased heat production (calorigenic) Sympathomimetic effect: Increase target cell responsiveness to catecholamines increase heart rate and the force of heart contraction. Effect on growth: stimulate GH secretion promote the effects of GH on the synthesis of new structural proteins and on skeletal growth Large amounts of the secreted hormone convert glycogen into glucose and stimulates protein degradation. Effect on nervous system: Necessary for normal development Normal CNS activity in adults 48 CONTROL OF THYROID HORMONE SECRETION 49 ABNORMALITIES OF THYROID FUNCTION Hypothyroidism Hyperthyroidism Goiter 50 ABNORMALITIES OF THYROID FUNCTION 1. 2. Hypothyroidism: thyroid hormone deficiency Cretinism : hypothyroidism from birth: Growth retardation Mental retardation Myxedema: In severe cases, development of edematous appearance throughout the body Symptoms: lowered basal metabolic rate, excessive weight gain, bradycardia, cold intolerance and the quick onset of fatigue. 51 ABNORMALITIES OF THYROID FUNCTION Hyperthyroidism: thyroid hormone excess Most common cause; Graves’ disease, body produces thyroid-stimulating immunoglobulin (TSI) which targets TSH receptors on thyroid cells Symptoms: exophthalmos (bulging eyes), elevated metabolic rate, high heart rate, heat intolerance 52 ABNORMALITIES OF THYROID FUNCTION Goiter Enlarged thyroid gland Becomes palpable and usually highly visible Occurs whenever either TSH or TSI excessively stimulates the thyroid gland 53 ADRENAL HORMONES 54 ADRENAL GLANDS Aldosterone (Mineralocorticoid) Cortisol (Glucocorticoid) Sex hormones 55 Catecholamines (Epinephrine+Norepinephrine) ALDOSTERONE 56 ALDOSTERONE EFFECTS Site of aldosterone action is on the distal and collecting tubules of the kidney Promotes Na+ retention osmotic H2O retention increased ECF volumes increased blood pressure Enhances K+ elimination 57 REGULATION OF ALDOSTERONE SECRETION Na+ deprivation Increase Plasma K+ Decreased ECF volume Renin Angiotensin II Aldosterone Aldosterone secretion is increased by: Activation of the renin-angiotensin system Direct stimulation of the adrenal cortex by a rise in plasma K+ concentration 58 CORTISOL 59 CORTISOL EFFECTS Metabolic effects stimulates hepatic gluconeogenesis inhibits glucose uptake and use by many tissues stimulates protein degradation in many tissues, especially muscle facilitates lipolysis Permissive actions permits the catecholamines to induce vasoconstriction Adaptation to stress Stress is one of the major stimuli for increased cortisol secretion Increased pool of glucose, amino acids, and fatty acids is available for use in stressful situations Anti-inflammatory and immunosuppressive effects Pharmacological effect (at higher than normal concentrations) Suppresses the body’s response to the disease Useful in allergic disorders and organ transplant rejections 60 CONTROL OF CORTISOL SECRETION highest in the morning lowest at night o ACTH from the anterior pituitary stimulates the secretion of cortisol from the adrenal cortex. o ACTH secretion is triggered by CRH from the hypothalamus. o Negative feedback from cortisol in the blood to the hypothalamus and the anterior pituitary regulates the level of cortisol in the blood. 61 ABNORMALITIES OF THE HORMONES OF THE ADRENAL CORTEX 62 ALDOSTERONE HYPERSECRETION Causes: E.g., Conn’s syndrome hypersecreting adrenal tumor made up of aldosterone-secreting cells (primary hyperaldosteronism ) The secondary hyperaldosteronism is due to the high activity of the renin-angiotensin mechanism. 63 CORTISOL HYPERSECRETION (CUSHING’S SYNDROME) due to increased amounts of CRH or ACTH, adrenal tumors, or ACTH-secreting tumors. The main symptom of this condition is excessive gluconeogenesis. mobilization of fat from the lower part of the body, with concomitant extra deposition of fat in the thoracic and upper abdominal regions “buffalo hump” “moon face” 64 ADRENOCORTICAL INSUFFICIENCY o o E.g., addison’s disease: autoimmune destruction of the cortex by production of cortex–attacking antibodies, affect all layers and so all cortical hormones Symptoms: hypotension, hypoglycemia, potassium retention and sodium depletion. There is poor response of the subject to stress and hypoglycemia pituitary or hypothalamic abnormality affects cortisol only 65 THE ENDOCRINE PANCREAS 66 ISLETS OF LANGERHANS Somatostatin Exocrine portion (acinar & duct cells) Glucagon 67 Insulin INSULIN Energy-giving foods in the diet, especially excess amounts of carbohydrates increases insulin secretion Insulin affects carbohydrate, fat, and protein metabolism 68 INSULIN ACTIONS Actions on carbohydrates o Facilitates glucose transport into most cells o Stimulates glycogenesis (Glucose Glycogen) o Inhibits glycogenolysis (Glycogen Glucose) o Inhibits gluconeogenesis (amino acids Glucose) Actions on fat o Enhances the entry of fatty acids from the blood into adipose tissue cells for storage as triglycerides Actions on protein o Promotes transport of amino acids from the blood into muscles and other tissues for protein synthesis 69 Lack of Effect of Insulin on Glucose Uptake and Usage by the Brain o o o Most of the brain cells are permeable to glucose and can use glucose without insulin Brain cells use only glucose for energy Hypoglycemic shock; progressive nervous irritability that leads to fainting, seizures, and even coma 70 GLUCOSE TRANSPORT BETWEEN THE BLOOD AND CELLS Glucose transporter (GLUT), Six forms (GLUT1-GLUT6) Most important GLUT4 (skeletal muscle and adipose tissue cells) GLUT4 is present on cell membrane upon insulin secretion only Although skeletal muscles have GLUT4: Resting depend on insulin Exercising free from insulin dependence, good for diabetes mellitus 71 DIABETES MELLITUS 72 DIABETES MELLITUS The most common of all endocrine disorders Due to inadequate insulin action Types o o lack of insulin secretion (type I) decreased sensitivity of the tissues to insulin (type II) 73 DIABETES MELLITUS The most prominent features of diabetes mellitus is elevated blood-glucose levels, or hyperglycemia Symptoms: • • • Polyphagia, excessive hunger and food consumption Polydipsia, excessive thirst Polyuria, increased urine output 74 TYPES OF DIABETES MELLITUS 75 CONSEQUENCES OF LOW INSULIN ACTIVITY Glucosuria. Excess urination also occurs. This can lead to circulatory failure, renal failure, and dehydration. Increased lipolysis. Fatty acids are mobilized from triglycerides. Liver use of fatty acids leads to ketosis. Acidosis develops and can depress brain function. Increased protein catabolism. This can reduce growth and lead to the wasting of skeletal muscles. Long-term complications of diabetes mellitus include degenerative disorders of the vascular and nervous systems. 76 GLUCAGON In general, glucagon actions are opposite to those of insulin Secretion increases during the postabsorptive state Pancreatic α cells increase glucagon secretion in response to a fall in blood glucose. Catabolic effects on energy stores The major site of action of glucagon is the liver 77 GLUCAGON ACTIONS Carbohydrates: Decreasing glycogen synthesis, promoting glycogenolysis, and stimulating gluconeogenesis Fat: Promoting fat breakdown and inhibiting triglyceride synthesis Proteins: Inhibiting hepatic protein synthesis and promotes degradation of hepatic protein, not muscle proteins The growth hormone, cortisol, epinephrine, and glucagon are insulin antagonists. They increase blood glucose. 78 ENDOCRINE CONTROL OF CALCIUM METABOLISM 79 REGULATION OF CALCIUM METABOLISM Plasma Ca++ levels are under the regulation of three hormones: o o o Parathyroid hormone (from parathyroid glands) Calcitonin (from thyroid gland) Vitamin D Regulation of Ca ++ metabolism depends on hormonal control of exchanges between the ECF and three other compartments: o o o Bone Kidneys Intestine 80 DISTRIBUTION OF CALCIUM IN THE BODY % Ca++ bone & teeth intracellularly extracellularly Half of the plasma Ca ++ is bound to plasma proteins the other half is free to leave the plasma and participate in chemical reactions 81 IMPORTANCE OF CALCIUM Neuromuscular excitability Hypocalcemia (decreased blood Ca++) overexcitability Hypercalcemia (increased blood Ca++) depressed neuromuscular excitability Affect Na+ permeability 82 BONE (THE LARGEST CALCIUM RESERVOIR) Bone continuously undergoes remodeling; bone deposition (formation) and bone resorption (removal) normally go on concurrently [Osteoblasts vs. Osteoclasts] Mechanical stress favors bone deposition 83 REGULATION OF CALCIUM METABOLISM 1. Parathyroid hormone (from parathyroid glands) 2. Calcitonin (from thyroid gland) 3. Vitamin D 84 1. PARATHYROID HORMONE (PTH) Increases plasma Ca++ levels via: o o o Increasing bone resorption Increasing kidney reabsorption Increasing intestinal absorption (via Vitamin D) Chief (principal) cells secrete PTH PTH also lowers phosphate ions in the blood. 85 REGULATION OF CALCIUM METABOLISM Calcitonin (from thyroid gland) 2. Lowers plasma Ca++ levels via increasing Ca++ deposition in bone Vitamin D 3. Its synthesis is stimulated by PTH in the kidney It increases plasma Ca++ levels mainly via increasing intestinal absorption Stimulates bone reabsorption. 86 Stimulates reabsorption of Ca++ and P043- by the kidney VITAMIN D (OR CHOLECALCIFEROL) Hormone or vitamin ? Activation of vitamin D PTH 87 THE END 88