How to recognize the different faces of Hypertension
advertisement

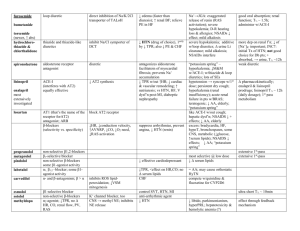
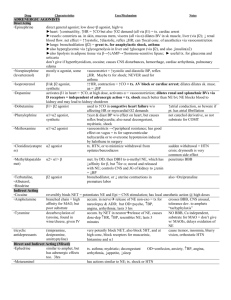
How to recognize the different faces of Hypertension Reena Kuriacose, MD. FACP. March 26,2012 Disclosures • No conflict of interest • Not a specialist • Statistical data varied Resistant hypertension • • • • BP above goal in spite of > 3 anti HTN meds All of these in optimal doses Resistant HTN = Refractory HTN Uncontrolled HTN = Resistant HTN Inadequate Rx Pseudo resistance Pseudo resistance • Attributed to other factors: - Inaccurate measurement - Poor adherence to Rx - White coat syndrome 20-30% (also more in resistant HTN: 37-44%) • Suboptimal Rx: Only 18-27% uncontrolled get Rx with at least 3 anti HTN meds Difficult to control HTN • • • • • • • • Higher baseline Left Ventricular Hypertrophy Older age Obesity- lifestyle and diet AA race Chronic kidney disease Diabetes Medications and herbal supplements Resistant HTN • Prevalence: Not known- 8.9-16% • Pt with ≥ 3 BP meds 1994: 14% to 2004: 24% • 5–20% HTN- specific underlying disorder I. Intravascular volume • ↑ Na ↑ vascular vol ↑ cardiac output • Overtime ↑ Peripheral resistance • Non chloride Na salts have no effect on BP • NaCl dependent HTN: - Intrinsic renal disease: ↓ capacity to excrete Na - ↑ Mineralocorticoid: ↑ tubular Na reabsorption - ↑ Neural activity to kidney: ↑ tubular Na reabsorption ESRD 80% volume dependent and respond to dialysis II. Autonomic Nervous System • Adrenergic receptors: α- activated by NE more than epinephrine β- activated more by epinephrine than NE • α₁ - vasoconstriction,↑ Renal Na reabsorption • α₂ - inhibit NE release • β₁ - ↑ rate and strength of cardiac contraction ↑ CO; ↑ renin release from kidney • β₂ - vasodilatation • Tachyphylaxis – sustained high levels of catecholamines ↓ response (orthostatic hypotension in pheo) • C/c ↓ catecholamines temporary hypersensitivity to sympathetic stimuli (clonidine withdrawal) • Sympathetic outflow: ↑ Obesity and OSA III. Renin-Angiotensin-Aldosterone • Angiotensin II Vasoconstriction Atherosclerosis • Aldosterone Na retention ↓ NaCl in distal asc loop of Henle ↓ pr. In afferent renal arteriole β₁ stimulation of renin secretion Pharmacological blockade of a. ACE receptor b. Angiotensin II receptor ↓K ----------- ↓ Secondary Hypertension • Severe or resistant hypertension • An acute rise in BP developing in a patient with previously stable values • Malignant or accelerated hypertension • < 30 years in non-obese, -ve FH, no other risk factors • >50 years Secondary Hypertension Resistant HTN with an identifiable cause: 1. 2. 3. 4. 5. 6. 7. Primary Aldosteronism Renal Artery Stenosis Chronic Kidney Disease OSA Pheochromocytoma Cushing’s Syndrome Aortic Coarctation Primary Aldosteronism • 10 – 20% of resistant HTN • Peak: 30–60 years • Unexplained hypokalemia- 37% > 50% Normokalemic @ presentation Unprovoked hypokalemia : 40-50% primary aldosteronism • Renal Mag wasting mild hypomagnesemia Primary Aldosteronism • ↑ Aldosterone ↑ Na, ↓ Renin ↑ K excretion • ↓ K ↓ Aldosterone synthesis correct K before eval for hyperaldosteronism Primary Aldosteronism • • • • • Resistant hypertension Spontaneous or thiazide-induced hypokalemia Serum K <3.1 mmol/L Incidentaloma FH of primary hyperaldosteronism Primary Aldosteronism • Adrenal adenoma: 60–70% Unilateral < 3cm • Unilateral/ bilateral adrenal hyperplasia • Adrenal carcinoma or an ectopic malignancy e.g., ovarian arrhenoblastoma- rare Primary Aldosteronism • PAC:PRA ratio (ratio ≥ 20:1) • Plasma aldosterone concentration (PAC) (>416 pmol/L) (>15 ng/dL)) • Sensitivity 90% , Specificity 91% for aldosterone-producing adenoma • Plasma renin activity (PRA) ↓ • 24 hr urine Na excretion, Creatinine clearance, aldosterone excretion Primary Aldosteronism • Medications that alter renin and aldosterone levels:Diuretics (especially spironolactone)- should be discontinued 4 weeks before ACE inhibitors, ARBs, β -blockers, Clonidine • Calcium channel and α-receptor blockers can be used Primary Aldosteronism • Confirmed by demonstrating : - Failure to suppress plasma aldosterone to isotonic saline - Failure to suppress aldosterone to oral NaCl load/ fludrocortisone/ captopril Primary Aldosteronism • High-resolution CT (90%) or MRI scanning • Bilateral adrenal venous sampling for plasma aldosterone (sensitivity 95% and specificity 100%) Primary Aldosteronism • Hyperplasia- Aldosterone receptor antagonist • Pts not willing for surgery Medical Rx (avoid extensive w/u) Renal Artery Stenosis • Atherosclerotic disease: 2/3 – older males OR • Fibromuscular dysplasia: 1/3- younger females • Renal artery stenosis: 1–2% of hypertensive patients 10-45% of refractory HTN • Prevalence 60% in >70 years Renal Artery Stenosis • < 20; > 50 years • HTN is resistant to ≥ 3 drugs • Epigastric / renal artery bruits • ↓ Renal perfusion pr → ↑ renin (over time secondary renal damage) Renal Artery Stenosis • Atherosclerotic disease of the aorta or peripheral arteries: - 15–25% of patients with symptomatic PVD in legs renal artery stenosis • Abrupt deterioration in kidney function (30%) after administration of ACE inhibitors • Episodes of pulmonary edema are associated with abrupt surges in BP Renal Artery Stenosis • BP meds can effectively control BP in many patients with renovascular HTN • Screening is not recommended unless plan is to intervene if a significant stenotic lesion is found: * Failure of medical therapy to control BP * Intolerance to medical Rx * Progressive renal failure * Young pt- to avoid life long Rx Renal Artery Stenosis • No ideal screening test for renal vascular HTN • Magnetic resonance angiographyatherosclerotic • Spiral CT with CT angiography • Duplex Doppler ultrasonography- operator dependant • Renal arteriography, the definitive diagnostic test (suspicion is sufficiently high ) ---------------------------------------* Renal insufficiency limits use of contrasts OSA • OSA seen in 71-85 % of resistant HTN referred for sleep study • 45% OSA without HTN develop HTN in 4 years • Blunted/ No ↓ in nighttime BP • >50% OSA HTN (independent of obesity) OSA • Screen if: Obesity + snoring + daytime sleepiness • CPAP (> 5.6 hr/night) Decreases both systolic and diastolic hypertension Pheochromocytoma • < 0.1% of all patients with hypertension • < 0.3% of Secondary hypertension • Incidence: 2-3/ million / yr autopsy: 250–1300/ million • Episodic HTN(90%) HA (80%) Diaphoresis (70%) Palpitation (60%) Anxiety (50%) Tremor (40%) • 90% in adrenals; 98% in Abdomen Pheochromocytoma • Hyperglycemia 35% • ↑ RBC • ↑ Ca • Leukocytosis • Occa ↑ ESR • PRA may be ↑ ed by catecholamines • Meds: Tricyclic antidepressants, Antidopaminergic agents, Metoclopramide, and Naloxone- can ppt HTNsive crisis Pheochromocytoma • • • • Plasma fractionated free metanephrines Used in high risk pts- FH or personal h/o pheo Sensitivity - 96% ; Specificity - 85% N levels = end of w/u • ↑ levels - Physical or emotional stress Sleep apnea MAO inhibitors,levodopa Pheochromocytoma • 24-hour urinary collection for catecholamines and metanephrines - Sensitivity - 87.5% ; Specificity of 99.7% - 2.2 mcg of total metanephrine /mg creatinine > 135 mcg total catecholamines /gm creatinine - Total u. metanephrine >1300mcg/24hr • Lab values varies- Slightly +ve tests not significant • 2-3 times above Normal • VMA is not required Pheochromocytoma • Noncontrast CT - followed by CT with nonionic contrast • MRI scanning • CT/ MRI - sensitivity ~ 90% for adrenal pheochromocytoma • Less sensitive - recurrent tumors, metastases, and extra-adrenal paragangliomas • I¹³¹ metaiodobenzyl guanidine if CT/MRI -ve Cushing’s syndrome • • • • 80% of spontaneous Cushing syndrome HTN ↑ WBC > 11,000/mm3 Hyperglycemia Hypokalemic metabolic alkalosis : Cortisol renal mineralocorticoid receptor. Cushing’s syndrome • 40% of cases are due to Cushing "disease,“ • ACTH hypersecretion by the pituitary- benign pituitary adenoma (98% in ant pituitary) • 10% nonpituitary ACTH-secreting neoplasms (eg small cell lung Ca) ↑ K & ↑ pigmentation • 15% ACTH source that cannot be initially located Cushing’s syndrome • 30% of cases- autonomous secretion of cortisol by the adrenals independently of ACTH • Benign adrenal adenomas (small) cortisol • Adrenocortical carcinomas (large) cortisol + androgens Cushing’s syndrome • Tests for diagnosis: - 24 hr Urinary free cortisol level - 1mg dexamethasone suppression test - Evening serum and salivary cortisol level Cushing’s syndrome • Urine Cortisol: - 24-hour urine collection >3-4 times upper limit (>200 µg/24hr) 3 N urine free cortisol – excludes • ↑ Free Urine cortisol: high fluid intake; preg, Carbamazepine and fenofibrate Cushing’s syndrome • Dexamethasone suppression test: 1 mg @11 pm cortisol @ 8 am; a cortisol level < 5 mcg/dL or < 2 mcg/dL • Phenytoin, Phenobarbital, Primidone, Rifampin, Estrogens (preg / OC) - lack of dexamethasone suppressibility false +ve • 8% of pituitary Cushing disease- also have suppression Cushing’s syndrome • Midnight serum cortisol level > 7.5 mcg/dL: - Same time zone for at least 3 days - Fasting for at least 3 hours - Indwelling IV line • Late-night salivary cortisol test: consistently > 0.25 mcg/dL (7.0 nmol/L) Cushing’s syndrome • Confirmation: - Low dose Dexa suppression test: Dexa 0.5mg q6hrX 48hrs - Cortisol > 55.2nmol/L (2 µg/dL) Cushing syndrome Etiology of Cushing’s • To differentiate ACTH dependant vs ACTH independent • Plasma or serum ACTH: < 5pg/mL = adrenal tumor > 10-20 pg/mL = pituitary or ectopic ACTHsecreting tumors. Etiology of Cushing’s • To differentiate Pituitary ACTH vs ectopic ACTH: - 8mg Dexamethasone suppression test @ 11pm: OR - 48-hr Dexamethasone suppression test: 2mg q 6hr X 8 doses - Cortisol suppression <50% of baseline = Pituitary ACTH - Sensitivity 80%; Specificity 70-80% - ↓ of 90% in U free cortisol ~ 100% specific for ant pit disease Cushing’s syndrome • MRI of the pituitary- pituitary lesion ~ 50% • Selective catheterization of the inferior petrosal sinus veins +/- CRH adm • CT scan: chest (lungs, thymus) abdomen (pancreas, adrenals)- 60% lesions found • 111In-octreotide (OCT, somatostatin receptor scintigraphy) scan: occult tumors • Non-ACTH-dependent Cushing syndrome- CT scan of the adrenals Coarctation of Aorta • 1-8/1000 live births • 30 % Subsequent HTN after surgical correction • Less severe lesions diagnosed in young adulthood Coarctation of Aorta • Diminished and delayed femoral pulses • Systolic pr gradient b/w R arm and legs / L arm • Blowing systolic murmur - posterior L interscapular areas • Chest x-ray and transesophageal echocardiography Other causes: • Renal: Polycystic kidney disease, Renin secretory tr, obstructive uropathy • Adrenal: 17α hydroxylase defi, 11β hydroxylase dehydrogenase defi • Preeclampsia/ Eclampsia • Neuro: psycogenic, polyneuritis, a/c ↑ICP • Hyperthyroidism (systolic HTN) Hypothyroidism (Mild diastolic HTN) ↑ Ca, acromegaly • Mendelian forms