BLOOD COMPONENTS
advertisement

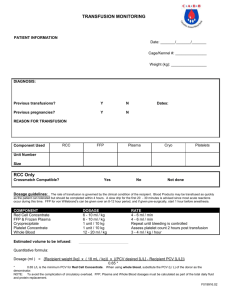
BLOOD COMPONENTS – PROCESSING, QUALITY ASSURANCE, STANDARDISATION Vesna Libek MD, PhD Blood transfusion specialist Head of Blood Transfusion Service Deputy manager CHC Zemun Belgrade Lecturer in Blood transfusion education department at Belgrade Medical University SERBIA Shenzhen, 2015 There is totally 81 million blood units transfused all over the world / per year P.J.L Carson., Carless: The evidence base for red blood cell transfusions. ISBT Science Series (2013) 8,89-92 Over 20 million blood units are collected in Europe from 13 million blood donors per year Project DOMAINE ( Donor Managment in Europe) Segmentation of blood donor population in blood donor types Veldhuizen I., Follea G., de Kort W.: Donor cycle and donor segmentation: new tools for improving blood donor management Vox Sanguinis(2013) 105, 28-37 Production- blood processing Allogenic and autologous whole blood donations Collection of components by apheresis Voluntary nonremunerated blood donor Fixed-site blood-collections Mobile blood collection Whole blood donation High-quality blood components meeting European guidelines can be prepared by using automated devices. Think of Critical control points for the donation process: Selection of blood donor Collection of the donation Handling and storage of the donation Transport of the donation to the processing center Distribution of blood component Avoid them with new technologies that automate the critical control points as far as possible During this process, following Guide to the preparation, use and quality assurance of blood components, 17th Edition is unavoidable PRINCIPLES: up-to-date useful information STANDARDS: mainly adherent to European Pharmacopeia and European Directives must be applied Relevant legislative & regulatory references 2001/83/EC “ community code relating to medicinal products for human use” 2002/98/EC “standards of quality and safety for the collection, testing, processing, storage and distribution of human blood and blood components 2004/33/EC “Eligibility of donors ...Quality and safety requirements for blood 2005/61/EC “…traceability requirements and notification of serious adverse reactions and events” 2005/62/EC “… Community standards and specifications relating to a quality system for blood establishments” PE 005-3 PIC/S GMP GUIDE FOR BLOOD ESTABLISHMENTS - 2007 GOOD PRACTICE GUIDELINES FOR BLOOD ESTABLISHMENTS AND HOSPITALS BLOOD BANKS required to comply with EU DE 2005/62 /CE - 15.11.2013 EDQM Guide to the preparation, use and quality assurance of blood components. Recommendation n. R(95)15. 17th Edition - 2013 WHO guidelines on good manufacturing practices for blood establishments -Technical Report Series, No. 961, 2011 Annex 4 Feuropean Pharmacopeia 8th Ed. Each blood establishment must develop and maintain QS based on EU Directive 2003/94/EC Good Manufacturing Practices (GMP) and complies with the requirements identified in Directive 2005/62/EC and its Annex. QUALITY MEANS: Quality system - organizational structure, responsibilities, processes, procedures and resources required to maintain high quality products and ⁄ or services. In blood transfusion chain setting- quality system provides a framework in a supply chain setting from a donor’s vein to a patient’s vein through the collection, processing, testing, distribution and administration of high quality, safe and effective blood and blood products.\ Quality system considers: quality management, blood component recall, quality assurance, external and internal auditing and issuance of blood components continuous quality improvement, personnel, premises Control of equipment and documentation, electronic data are important part of QS. collection, processing, testing, release, storage, distribution, Non conformities and corrective and preventive measures are included. Quality control testing of components are done following the recommended percent of all produced components. Strengers P.:ISBT Working Party on Quality Management. Transfusion Today, 96:4-5, 2013. A quality assurance programs - ensure that there are processes in place, to control and monitor all critical steps the application of quality assurance to every part of the manufacturing process from donor selection through to dispatch of the components to the hospitals. quality assurance can ensure consistency of product, reliable results, effective risk-based decision making and reduction in wastage through minimization of errors. Quality assurance therefore provides a strong basis for donor, product and staff safety. QM considers: Self inspection to improve some field of work as well as Regulatory inspection by Competitive authorities or state accreditation body Seidl C.:Standards, criteria and trainig requirements for improving quality managment. Transfusion Today, 96:6-7, 2013. Quality policies Quality procedures SOPs Records Structure of controlled document system For all working procedures SOPs (Standard Operative Procedures), which represent the exact steps in working process- need to be written. Effective, streamlined SOPs based on principles of good practice that comply with relevant regulation. European Project addressing the safety of blood transfusion EU-Optimal Use of Blood Project cofounded by the European Commission The EU-Q-Blood-SOP Project cofounded by the European Commission The European Commission, Public Health Program Blood Quality Project EQUAL The main goal of the Project - “Good Quality Management” (QM) in Blood Transfusion Services On the Basis of the Directive 2002/98/EC of Europian Comission (Blood Directive) Through the Project the Manual for EU Standard Operating Procedures was writen www.equal-blood.eu C. Seidl. European perspective of quality management in blood establishments - The EuBIS manual and training guide. XXXIth (ISBT) in joint cooperation with the 43rd Congress of the DGTI, Berlin, 2010. Continuously improving the quality of processing procedures and the quality of final components EDQM, WHO Harmonization of definitions connected to QM QM include human resources too Strengers P.:ISBT Working Party on Quality Managment. Transfusion Today, 96:4-5, 2013. C. Seidl. The EUBIS standards and criteria for the inspection of blood establishments Introduction and overview of the EuBIS manual and training guide. XXXIth (ISBT) in joint cooperation with the 43rd Congress of the DGTI, Berlin, 2010. Equivalent recognition of inspections of blood establishments among all Member States through the development and implementation of commonly accepted criteria and standards leading to comparable quality systems and inspection procedures. EUBIS: Enable that blood components are collected and prepared to a consistently high standard of safety across Europe. Define requirements for the quality management system for blood establishments based on the Directive 2005/62/EC Develop pan European standards and criteria for the inspection of blood establishments (GMP guidelines, implementing the Directive 2002/98/EC and its technical annexes). Establish a common benchmark system for deviations and improvements. Develop a training program for inspectors Seidl C, Brixner V, Müller-Kuller T, Sireis W, Costello P, Cermakova Z, Delaney F, McMillan Douglas A, Nightingale M, van Galen JP , O’Connell M, Siegel W, Sobaga L, de Wit J, Seifried E. Levels of quality management of blood transfusion services in Europe. Vox Sang 2008.; 3 (1) : 54-62 Project co-funded by the European Commission, DG Sanco EUBIS - Standards and Criteria developed based on the European Blood legislation with cross-reference to common used European and International standards defined by its survey in Annex I of the Grant Agreement (Vox Sanguinis, Science Series Vol (3), Seidl et al. 2008). Project “Optimal USE of Blood” - Improve safety for the donor reducing the unnecessary bleeding of donors - Improve safety for the patient improving the transfusion process, reducing the unnecessary transfusion of blood. - Improve effectiveness of health services -blood components to be used in the most therapeutically beneficial way for patients. - Improve efficiency of health services reducing inefficient use of resources. To summarize the current status in routine preparation process of blood components Critical parameters during the donation process and the period before separation Temperature control Storage time and temperature before separation Phagocytosis and self-sterilization Leucodepletion Red cell concentrates Platelet concentrates Additive solutions Agitation Storage lesion Cold storage of platelets Storage period of PCs Therapeutic plasma Pathogen inactivation Production of cellular blood components from undifferentiated cells in vitro Henschler R, Müller M.M, Pfeiffer H.U, Seifried E, Sireis W.: Production of standard blood components. ISBT Science Series (2010) 5,190-195 Following standards for collection of blood and blood components: premises for donor sessions, procedures and equipment used at blood donation sessions, pre-donation checks, labelling, venipuncture, bleeding and mixing, handling of filled blood bags following special requirements for Apheresis Not less important is having the repository of archive samples. Collection of blood, Initial step in preparing standardized blood components, proper mixing with the anticoagulant continuously at all phases of the bleeding is important. From blood donation through dividing tubes and small pre donation bag, from initial blood bag and then towards producing different blood components in everyday work, depends on well-chosen equipment. The plastic - need to be tolerant to temperatures required for blood steam sterilization and plasma freezing Clear - to allow visual assessment and processing Strong enough - to tolerate centrifugal processing and pressure infusion Polyvinyl chloride (PVC) , plasticized with di-2-ethylhexyl phthalate (DEHP) –safety? The size, and thickness of platelet bags and the fracture resistance of plasma bag Plastic bags (DEHP free, PVC free) for platelet storage with better gas diffusion capabilities are widely available. Modern bags are also sized to prevent overdrawing With the adoption of the ambient overnight hold of whole blood before processing the importance of the plasticizer in the primary collection bag may increase. Prowse C.V., de Korte D., Hess J.R., van der Meer P.F.: Commercially available blood storage containers. Vox Sang 2014, 106:1-13. Either to store whole blood (WB) units up to 24 h before processing, the WB is actively chilled to 22±2ºC Usually by placing the WB bags under cooling plates filled with butane-1,4-diol The WB is rapidly cooled from a post collection temperature of about 34ºC to 22±2ºC within 2-3h Thibault L., Beausejour A., Jacques A., Ducas E., Tremblay M.: Overnight storage of whole blood: cooling and transporting blood at room temperature under extreme temperature conditions. Vox Sang 2014; 106: 127-136 Processing of blood Blood components may be prepared either during collection of whole blood with further processing through centrifugation or during collection using apheresis technology. Component separation after the initial centrifugation of whole blood Separation after initial filtration T/B Quadruple bag Commonly used quality measures for fresh cellular components Tests for platelet quality Measuring platelet activation state • CD62P expression • Annexin V binding • Extent of shape change • Morphology score • Swirl Measuring platelet metabolic activity • Glucose • Lactate • pH Tests of red cell concentrate quality Measuring red cell metabolism • 2,3- DPG • ATP and other nucleotides • Glucose Measuring red cell integrity • Osmotic fragility • Potassium • Morphology • CD47 level • Annexin V binding • Per cent haemolysis at outdate • The condition of centrifugation determines the composition of the desired component. • The choice of initial separation step as well as using initial filtration strongly influences the choice of methods for further processing. • Together with methods of freezing plasma, irradiation of blood components, pathogen reduction and different additive solution we can also produce modified components using appropriate equipment. Different factors influence the possible stock period of components: Composition of conservers, additive solutions, post production manipulation for instance- irradiation Williamson L., Devine D.: Challenges in the management of the blood supply Lancet 2013 (381):1866-1875. The separation of blood components from whole blood collections can be automated by a different devices producing standardized blood components, good quality control and increased work efficiency. Processing of blood components carried out using appropriate and validated procedures including measures to avoid risk of bacterial contamination. The labelling system for the collected blood, blood components and samples must unmistakably identify the type of the content and must be the link to obtain traceability of the donation. There must be the safe system for realizing components after all mandatory requirements priory being fulfilled. Procedures for storage and distribution need to keep blood component quality during whole storage period. All processes for irradiation and leucodepletion must also be standardized. Red cell components can be processed like: Red cells RC buffy coat removed, RC in additive solution, RC buffy coat removed in additive solution, RC leucocyte depleted, RC leucocyte depleted in additive solution, RC apheresis, RC washed and RC cryopreserved. Automatic separators allows even simultaneously separation of two blood units and whit the T/B quadruple blood bags we came closer to full automation with shortening separation period. Immediately transferred data to the PC and stored in electronic form and as printed copy, enables haemovigilance. The quality of samples from tubing segments is not representative of the quality of the corresponding RBC unit. Segments are not suitable surrogates with which to assess RBC quality. Segments from red blood cell units should not be used for quality testing Jayme D.R. Kurach1,2,3, Adele L. Hansen1,2,3, Tracey R. Turner1,2,3,Craig Jenkins1,2,3, Jason P. Acker1,2,3,* Transfusion Volume 54, Issue 2, pages 451–455, February 2014 QC of RBC components RBCs without BC In additive solution RBCs leucocytedepleted RBCs leucocytedepleted in AS Red blood cells RBCs without BC RBCs in additive solution Volume (mL) 280±50 250±50 Depends on AS Depends on AS To be defined for the system used To be defined for the system used Hematocrit 0,65-0,75 0,65-0,75 0,50-0,70 0,50-0,70 0,50-0,70 0,50-0,70 Hemoglobin (g/unit) ≥ 45 ≥ 43 ≥ 45 ≥ 43 ≥ 40 ≥ 40 Special demands - Residual leucocyte content / unit <1,2x109 per unit - Residual leucocyte content / unit <1,2x109 per unit Residual leucocyte content / unit <1 x106 per unit Residual leucocyte content / unit <1 x106 per unit Haemolysis at the end of storage(% of RC mass <0,8 <0,8 <0,8 <0,8 <0,8 <0,8 Volume (mL) Washed RBCs RBCs cryopreserved Apheresis RBCs To be defined for the system used > 185 ml To be defined by the system used Hematocrit 0,65-0,75 0,65-0,75 0,65-0,75 (0,50-0,70 with AS) Hemoglobin (g/unit) ≥ 40 ≥ 36 ≥ 40 Special demands Protein content final supernatant < 0,5 g / unit Residual leucocyte content / unit <1 x106 per unit Haemolysis at the end of storage(% of RC mass <0,8 Residual leucocyte content / unit <1 x109 per unit Osmolarity < 340 mOsm/L Sterile Haemoglobin supernatant < 0,2 g /per unit <0,8 Improve product quality through improved technology Gravitational separation of cells based on their density Two methods for the ultimate preparation of platelet concentrates PRP production ( soft spin hard spin) “Buffy coat” production (hard spin several BC pooled together soft spin) Development of additive solutions Devine D.V., Howe D. : Processing of whole blood into cellular blood components and plasma. ISBT Science Series 2010 (5):78-82. Pooling BC by the system Pooling BC by the chain method Transfusion medicine in Germany: Current Status and Perspectives. Frankfurt 2010 (ISBT) Platelet component can be prepared as single unit from PRP (platelet rich plasma) or from buffy coat. Platelets can be pooled, produced directly from whole blood derived buffy coats or after pooling 4 to 6 single units of platelets. Platelets can be also produced as: pooled leucocyte depleted, pooled in additive solution, pooled leucocyte depleted in additive solution, or platelets pooled pathogen reduced and platelets donated by apheresis either leucocyte depleted, in additive solution, or pathogen reduced. There are also platelets cryopreserved. Pooled platelet concentrate (from 4-6 blood units) – 240-360 X109 Plt in 250-300 ml of plasma or additive solution Apheresis platelets 200-400 X109 Plt in 200-300 ml of plasma from one donor Devine D.v.; Howe D.: Processing of whole blood into cellular components and plasma. ISBT Science Series (2010)5,78-82 Many of activation processes are calcium dependent Avoid Plt activation with introduction of leucoreduction filters Plt activation aggregates Reduction of the ionized Ca++ level with citrate based anticoagulants inhibited Plt activation Collection and storage of platelets Preserving Plt functional capacity to respond when transfused Preventive measures for aggregates formation: lowering pH Resting period before further processing Van der Meer P.F.& al. Aggregates in platelet concentrates. Vox Sanguinis (2015)108,96-100. Pathogen reduction treatment (PRT) leads to an increase of platelet metabolism and activation independent of the length of the initial rest times. PCs resuspended in autologous plasma - stored at maximum up to day 5. mixture of plasma and PAS improves pH and platelet metabolism but not platelet activation. Prolonged shelf-life for up to 7 days may be possible. Janetzko K, Hinz K, Marschner S, Goodrich R, Klüter H: Evaluation of different preparations procedures of pathogen reduction technology (Mirasol®) treated platelets collected by plateletpheresis. Transfus Med Hemother 2009;36:309-317. Janetzko K, Hinz K, Marschner S, Goodrich R, Klüter H: Pathogen reduction technology (Mirasol®) treated single donor platelets resuspended in a mixture of autologous plasma and PAS. Vox Sang 2009;97:234-239. Pathogen inactivation Increase the standard of care Pooled product based on solvent detergent treatment Single donor based on: methylene blue amotosalen riboflavin Recent advances in blood component processing technology Rebecca Cardigan (Jun 1, 2014; 53446) Prolonged life time of Platelet concentrates to 7 days in some countries if they are tested for bacterial contamination or if they are pathogen reduced Williamson L., Devine D.: Challenges in the management of the blood supply Lancet 2013 (381):1866-1875. Platelet concentrates in electrolytic medium instead of plasma supernatant Less post transfusion reactions Better cell quality Prolonged life time to 10 days on agitators in incubators Additional additives for better PC quality: better energetic metabolism, reduction of metabolic stress, increase the stability of cells - post transfusion improve recovery Heaton W.A. Costs and benefits of PAS platelets: A mix of science,quality, and value . TRANSFUSION 2013;53:25972602. Leuco reduced Plt concentrates in small volumes with 6% DMSO frozen and kept on -80ºC For alloimunised patients and for military purposes During frost–defrost procedures there is lost of 23% Plt count Hornsez et al. Freezing of buffy coat-derived, leucoreduced platelet concentrates in 6% dimethyl sulfoxide. Transfusion (2008) 48:2508-2514. QC of Plt components Plt pooled pathogen reduced > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt Minimum 2 x1011 Minimum 2 x1011 Plt recovered pooled > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt Minimum 2 x1011 Minimum 2 x1011 Per unit Per unit < 1 x106 per final unit < 0,3 x109 per final unit < 1 x106 per final unit > 6,4 > 6,4 > 6,4 Platelet content per final unit pH measured (+22ºC) at the end of the recommended shelf-life Plt recovered pooled LD In additive solution Plt recovered single unit Volume (mL) Residual leucocytes per final unit a. Prepared from BC b. Prepared from PRP Plt recovered pooled In additive solution Plt recovered pooled leucocyte depleted > 60 x109 a. b. < 0,05 x109 < 0,2x109 > 6,4 Minimum 2 x1011 < 1 x109 per final unit (either BC pooled or pooling of single Plt units) > 6,4 Per unit < 1 x106 per final unit > 6,4 Volume (mL) For use in neonates and infants: Minimum 0,5 x1011 Per unit pH measured (+22ºC) at the end of the recommended shelf-life > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt > 40 mL per 60 x109 of Plt Standard unit: Minimum 2 x1011 Standard unit: Minimum 2 x1011 Standard unit: Minimum 2 x1011 > 40 mL per 60 x109 of Plt Per unit Residual leucocytes per final unit Plt apheresis LD in AS Plt apheresis Standard unit: Minimum 2 x1011 Platelet content per final unit Plt apheresis In additive solution Plt apheresis pathogen reduced Plt apheresis leucocyte depleted < 0,3 x109 > 6,4 Per unit Per unit Per unit For use in neonates and infants: Minimum 0,5 x1011 For use in neonates and infants: Minimum 0,5 x1011 For use in neonates and infants: Minimum 0,5 x1011 Per unit Per unit Per unit Minimum 2 x1011 < 1 x106 per final unit < 0,3 x109 per final unit < 1 x106 per final unit < 1 x106 per final unit > 6,4 > 6,4 > 6,4 > 6,4 Plt cryopreserved 50 – 200 mL More than 40% of the prefreeze platelet content Plasma, Fresh Frozen (FFP) Plasma, Fresh Frozen is a component for transfusion or for fractionation prepared either from Whole Blood or by apheresis, frozen within a period of time and to a temperature that will adequately maintain the labile coagulation factors in a functional state. • Plasma, Fresh Frozen used as Human plasma for fractionation must comply with the specifications of the European Pharmacopoeia monograph Human plasma for fractionation (Ph. Eur. monograph 0853). • Plasma, Fresh Frozen (FFP) used for clinical transfusion must comply with the specifications given in the monograph of the R 95(15) Guide (Part D, Paragraph 1). Preparation a. From whole blood •hard spin centrifugation, •preferably within 6 hours (no > 18 hours if the unit is refrigerated). •Whithin 24 h if whole blood has been rapidly cooled between + 20 ºC and + 24 ºC •Freezing must be completed within one hour to a temperature below – 30 ºC. The plasma core temperature reaches -30°C within less than 1 hour. b. By apheresis •The freezing process must commence within six hours of completion of the procedure and completed within one hour to a temperature below – 30 ºC. •If plasma is maintained between + 20 °C and + 24 °C immediately after collection can be held at that temperature for up to 24 hours prior to freezing. c. Quarantine FFP • This FFP is released once the donor has been retested, at least for HBsAg, anti-HIV and anti-HCV, with negative results after a defined period of time, designed to exclude the risk associated with the window period. • A period of six months is generally applied. This may be reduced if NAT testing is performed. QC of FFP FFP pathogen reduced. Volume (mL) F VIII Fibrinogen Residual cells Requirements Stated volume ± 10% Average not less than 50 IU F VIII per 100 mL Average (after freezing and thawing):≥ 60% of the potency of the freshly collected plasma unit Red cells:< 6,0 x109 /L Leucocytes: < 0.1 x109 /L Platelets: < 50 x109 /L If leucocyte depleted: < 1 x106 /L Frequency of control All units Every 3 months 10 units in the first month of storage Every 3 months 10 units in the first month of storage 1% of, all units with a minimum of 4 units per month 1% of, all units with a minimum of 10 units per month Leakage No in any part of container All units Visual changes No abnormal color or visible clots. All units • When there is cryoprecipitate prepared, then there is also FFP cryoprecipitate depleted produced. Cryoprecipitat Volume (mL) F VIII Fibrinogen Von Willebrand factor Requirements 30 – 40 mL ≥ 70 IU per unit ≥ 140 mg per unit > 100 IU per unit Frequency of control All units Every 2 months : a. A pool of 6 units of mixed blood groups during their first month of storage b. A pool of 6 units of mixed blood groups during their last month of storage 1% of, all units with a minimum of 4 units per month Every 2 months : a. A pool of 6 units of mixed blood groups during their first month of storage b. A pool of 6 units of mixed blood groups during their last month of storage LABELLING ISBT 128 LABEL STANDARD UNIT (CDM: UNIQUE WORLD NUMBER) TYPE OF PRODUCT BLOOD GROUP EXP.DATE The computer system of blood establishment or hospital blood bank includes: hardware, software, peripheral devices and documentation (e.g. SOPs, manuals). Such blood bank information system could consist of different parts, modules, connected to donation process, filing process, production management and laboratory part. These systems are the core of the supply chain management, which records and monitors all processes from blood donation to post-transfusion follow-up in adherence to international standards. It also consists of warning, guidance and decision support tools, which enables the adoption of processes that meet international standards. Production of blood components in EU Production by BC method High % of leucofiltration Some countries doesn’t produce cell components of first time blood donation Quarantine FFP Some countries use only man FFP or nulliparous FFP in therapy High percentage of apheresis PC NAT testing for HBV, HCV, HIV Testing for bacterial contamination of PC Some of member states use only virus inactivated FFP for all patients or some group of patients Blood components are typed in Rh system and Kell sistem Production - statistic All WB (whole blood ) donations are separated in blood components: RBC concentrates, plasma concentrates and BCs (buffy coats) 20% of plasma used as therapeutic – FFP (after 4 months of quarantine storage) 80% of plasma for further fractionation Most apheresis procedures – double apheresis 40% of collected BCs for manufacturing pooled random Plt concentrates (comprised of 4 BCs) Since 2001, RC concentrates and Plt concentrates are 100% leukodepleted Irradiation for medical purpose individually for red cells and Plt concentrates Pathogen reduction (Plt concentrates, FFP) Washed erythrocyte concentrates in rare cases Transfusion medicine in Germany: Current Status and Perspectives. Frankfurt 2010 (ISBT) The administration of blood and blood components involves more than 70 steps and each of these may be subject to error. Standard protocols for the administration of blood are essential to minimize the potential for error. These protocols should be in place in each institution and should conform to standard practice. A quality management system should exist in each institution. This should include an active transfusion committee, a process to correct protocols and practice when deficiencies are identified, participation in local and regional audit and in the national haemovigilance program. Biological variations between blood donors influence the component production itself Component processing can not completely optimize the quality of products Blood components are highly concentrated but they are not completely free of other blood elements Williamson L., Devine D.: Challenges in the management of the blood supply Lancet 2013 (381):1866-1875. Future steps To follow the influence of specific blood donor characteristics on processed blood components The production of blood components from hematopoietic steam cells in laboratory 1. Mountford J, Olivier E, Turner M. Prospect for the manufacture of red cells for transfusion. Br J Haematolog 2010; 149:22-34. 2. Reems JA, Pineault N, Sun S. In vitro megakaryocyte production and platelet biogenesis: state of the art. Transf Med Rev 2010; 24:33-43. 3. Giarratana MC, Rouard H, Dumont A, et al. Proof of principle for transfusion of in vitro-generated red blood cells. Blood 2011;118: 5071-79. • Blood and blood components are biological products • Automatisation = standardisation vesna.libek@gmail.com 谢谢!