Chapter 22: The Lymphatic System
advertisement

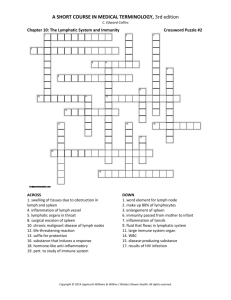
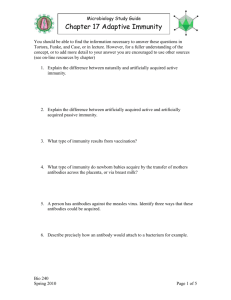
Chapter 22: The Lymphatic System Biology 142 A&P R.L. Brashear-Kaulfers Pathogens • Microscopic organisms that cause disease: – – – – viruses bacteria fungi parasites • Each attacks in a specific way The Lymphatic System Protects us against disease • Lymphocytes: • Lymphatic system cells respond to: – environmental pathogens – toxins – abnormal body cells, such as cancers What is the difference between nonspecific and specific defense, and the role of lymphocytes in the immune response? Specific Defenses • Lymphocytes: – part of the immune response • Identify, attack, and develop immunity to a specific pathogen • Immunity- The ability to resist infection and disease The Immune System • All body cells and tissues involved in production of immunity: – not just lymphatic system Nonspecific Defenses • Block or attack any potential infectious organism • Cannot distinguish one attack from another PLAY Immunity: Nonspecific Defenses What are the major components of the lymphatic system and their functions? Organization of the Lymphatic System Figure 22–1 4 Parts of the Lymphatic System 1. Lymph: – – a fluid similar to plasma does not have plasma proteins 2. Lymphatic vessels (lymphatics): – network that carries lymph from peripheral tissues to the venous system 3. Lymphoid tissues and lymphoid organs: – found throughout the body 4. Lymphocytes, phagocytes, and other immune system cells Function of the Lymphatic System • To produce, maintain, and distribute lymphocytes**Lymphocyte Production: - Lymphocytes are produced: – in lymphoid tissues (e.g., tonsils) – lymphoid organs (e.g., spleen, thymus) – and in red bone marrow ** Lymphocytes Distribution: – detect problems – travel into site of injury or infection Lymphocyte Circulation • From blood to interstitial fluid (lymph) through capillaries • Returns to venous blood through lymphatic vessels The Circulation of Fluids • From blood plasma to lymph and back to the venous system • Also transports hormones, nutrients, and waste products Lymphatic Vessels • Are vessels that carry lymph • Lymphatic system begins with smallest vessels: lymphatic capillaries (terminal lymphatics) • Lymphatic Capillaries• Differ from blood capillaries in 4 ways: – – – – start as pockets rather than tubes have larger diameters have thinner walls flat or irregular in section Lymphatic Capillaries Endothelial cells loosely bound together with overlap Overlap acts as one-way valve: allows fluids, solutes, viruses, and bacteria to enter prevents return to intercellular space Figure 22–2 Lacteals • Are special lymphatic capillaries in small intestine • Transport lipids from digestive tract Lymphatic Vessels and Valves Figure 22–3 Lymph Flow • From lymphatic capillaries to larger lymphatic vessels containing one-way valves • Lymphatic vessels travel with veins Lymphatic Ducts and the Venous System Figure 22–4 The Lymphatic System • Is divided into: 1) Superficial lymphatics - located in: – skin – mucus membranes – serous membranes lining body 2) Deep lymphatics- Are larger vessels that accompany deep arteries and veins Superficial and Deep Lymphatics • Join to form large lymphatic trunks • Trunks empty into 2 major collecting vessels: – thoracic duct – right lymphatic duct The Inferior Thoracic Duct • Collects lymph from: – left bronchiomediastinal trunk – left subclavian trunk – left jugular trunk • Empties into left subclavian vein The Right Lymphatic Duct • Collects lymph from: – right jugular trunk – right subclavian trunk – right bronchiomediastinal trunk • Empties into right subclavian vein Lymphedema • Blockage of lymph drainage from a limb • Causes severe swelling • Interferes with immune system function Why are lymphocytes important, and how are they distributed in the body? • Lymphocytes • Make up 20–30% of circulating leukocytes • Most are stored, not circulating 3 Classes of Circulating Lymphocytes 1. T cells: thymus-dependent Make up 80% of circulating lymphocytes 2. B cells: bone–marrow derived • Make up 10–15% of circulating lymphocytes • Differentiate into plasma cells- Produce and secrete antibodies (immunoglobin proteins) 3. NK cells: – natural killer cells 3 Main Types of T Cells 1. Cytotoxic T cells-Attack cells infected by viruses Produce cell-mediated immunity 2. Helper T cells- Stimulate function of T cells and B cells 3. Suppressor T cells-Inhibit function of T cells and B cells Regulatory T Cells • Are helper and suppressor T cells • Control sensitivity of immune response Other T Cells • Inflammatory T cells • Suppressor and inducer T cells Antigens • Targets which identify any pathogen or foreign compound Immunoglobin Proteins (Ig’s) Also called antibodies (Ab) • The binding of a specific antibody to its specific target antigen initiates antibodymediated immunity: - A chain of events which destroys the target compound or organism Natural Killer (NK) Cells • Also called large granular lymphocytes • Make up 5–10% of circulating lymphocytes • Responsible for immunological surveillance • Attack: – foreign cells – virus-infected cells – cancer cells Lymphocyte Distribution • Tissues maintain different T cell and B cell populations • Lymphocytes wander through tissues: – enter blood vessels or lymphatics for transport – can survive many years Production and Distribution of Lymphocytes Figure 22–5 Lymphopoiesis • Lymphocyte production involves: – bone marrow – thymus – peripheral lymphoid tissues • Hemocytoblasts : In bone marrow, divide into 2 types of lymphoid stem cells Lymphoid Stem Cells • Group 1: – remain in bone marrow – produce B cells and natural killer cells • Group 2: – migrate to thymus – produce T cells in environment isolated by blood-thymus barrier T Cells and B Cells • Migrate throughout the body: – to defend peripheral tissues • Retain their ability to divide: – is essential to immune system function Differentiation • B cells differentiate: – with exposure to hormone interleukin-7 • T cells differentiate: – with exposure to several thymic hormones • Interleukin-7 - A cytokine produced by stromal cells in bone marrow What are the structures and functions of lymphoid tissues and organs? Lymphoid Tissues : Connective tissues dominated by lymphocytes Lymphoid Nodules Figure 22–6 Lymphoid Nodule • Areolar tissue with densely packed lymphocytes • Germinal center contains dividing lymphocytes Distribution of Lymphoid Nodules • • • • Lymph nodes Spleen Respiratory tract (tonsils) Along digestive and urinary tracts Mucosa-Associated Lymphoid Tissue (MALT) • Lymphoid tissues associated with the digestive system: – aggregated lymphoid nodules: • clustered deep to intestinal epithelial lining • Appendix: – mass of fused lymphoid nodules The 5 Tonsils • In wall of pharynx: – left and right palatine tonsils – pharyngeal tonsil (adenoid) – 2 lingual tonsils Lymphoid Organs • • • • • Lymph nodes Thymus Spleen Are separated from surrounding tissues By a fibrous connective-tissue capsule Lymph Nodes • Range from 1–25 mm diameter Figure 22–7 Afferent Lymphatic Vessels • Carry lymph: – from peripheral tissues to lymph node Efferent Lymphatic Vessels Leave lymph node at hilus • Carry lymph to venous circulation Lymph from Afferent Lymphatics • Flows through lymph node in a network of sinuses: • From subcapsular sinus: – contains macrophages and dendritic cells • Through outer cortex: – contains B cells within germinal centers • Through deep cortex: – dominated by T cells • Through the core (medulla): – contains B cells and plasma cells – organized into medullary cords • Into hilus and efferent lymphatics Lymph Node • A filter: – purifies lymph before return to venous circulation • Removes: – debris – pathogens – 99% of antigens Antigen Presentation • First step in immune response • Extracted antigens are “presented” to lymphocytes: – or attached to dendritic cells to stimulate lymphocytes Lymphoid Functions • Lymphoid tissues and lymph nodes: – distributed to monitor peripheral infections – respond before infections reach vital organs of trunk Lymph Nodes of Gut, Trachea, Lungs, and Thoracic Duct • Protect against pathogens in digestive and respiratory systems Lymph Glands • Large lymph nodes at groin and base of neck • Swell in response to inflammation Lymphadenopathy • Chronic or excessive enlargement of lymph nodes may indicate infections, endocrine disorders, or cancer The Thymus Figure 22–8 The Thymus • Located in mediastinum • Deteriorates after puberty: – diminishing effectiveness of immune system • Divisions of the Thymus Thymus is divided into 2 thymic lobes • Septa divide lobes into smaller lobules A Thymic Lobule • Contains a dense outer cortex • And a pale central medulla Thymus Hormones • Thymosins • Promote development of lymphocytes Lymphocytes • Divide in the cortex • T cells migrate into medulla • Mature T cells leave thymus by medullary blood vessels Reticular Epithelial Cells in the Cortex • Surround lymphocytes in cortex • Maintain blood-thymus barrier • Secrete thymic hormones that stimulate: – stem cell divisions – T cell differentiation Reticular Epithelial Cells in the Medulla • Form concentric layers (Hassall’s corpuscles) • The medulla has no blood–thymus barrier: – T cells can enter or leave bloodstream The Spleen Figure 22–9 3 Functions of the Spleen 1. Removal of abnormal blood cells and other blood components by phagocytosis 2. Storage of iron recycled from red blood cells 3. Initiation of immune responses by B cells and T cells: – in response to antigens in circulating blood Structure of the Spleen • Attached to stomach by gastrosplenic ligament • Contacts diaphragm and left kidney • Splenic veins, arteries, and lymphatic vessels: – communicate with spleen at hilus Structure of the Spleen • Inside fibrous capsule: – Red pulp: contains many red blood cells Contains elements of circulating blood plus fixed & free macrophages – White pulp: resembles lymphoid nodules Trabecular Arteries • Branch and radiate toward capsule • Finer branches surrounded by white pulp • Capillaries discharge red blood cells into red pulp Splenic Circulation • Blood passes through: – network of reticular fibers • Then enters large sinusoids (lined by macrophages): – which empty into trabecular veins Spleen Function • Phagocytes and other lymphocytes in spleen: – identify and attack damaged and infected cells – in circulating blood Body Defenses • Provide resistance to fight infection, illness, and disease • 2 categories of defenses: • nonspecific defenses = Always work the same way , against any type of invading agent • specific defenses = Protect against specific pathogens • Depend on activities of lymphocytes • Specific resistance (immunity): – develops after exposure to environmental hazards 7 Types of Nonspecific Resistance 1. 2. 3. 4. 5. 6. 7. Physical barriers Phagocytic cells Immunological surveillance Interferons Complement Inflammation Fever Nonspecific and Specific Defenses • Operate together to provide resistance to infection and disease The 7 Nonspecific Defenses Figure 22–10 The 7 Nonspecific Defenses • Physical Barriers -Keep hazardous materials outside the body • Phagocytes -Attack and remove dangerous microorganisms • Immunological Surveillance -Constantly monitors normal tissues: – with natural killer cells (NK cells) • Interferons -Trigger production of antiviral proteins in normal cells Antiviral proteins: – do not kill viruses – block replication in cell The 7 Nonspecific Defenses • Complement (C) Proteins -Form the complement system Complements action of antibodies • Inflammation -Triggers a complex inflammatory response • Fever -A high body temperature: – increases body metabolism – accelerates defenses – inhibits some viruses and bacteria PLAY Immunity: Complement What are the components and mechanisms of each nonspecific defense? Physical Barriers • • • • Outer layer of skin Hair Epithelial layers of internal passageways Secretions that flush away materials: – sweat glands, mucus, and urine • Secretions that kill or inhibit microorganisms: – enzymes, antibodies, and stomach acid 2 Classes of Phagocytes • Microphages: neutrophils and eosinophils • Leave the bloodstream • Enter peripheral tissues to fight infections • Macrophages: large phagocytic cells derived from monocytes • Distributed throughout body • Make up monocyte–macrophage system (reticuloendothelial system) Activated Macrophages • Respond to pathogens in several ways: – – – engulf pathogen and destroy it with lysosomal enzymes bind to pathogen so other cells can destroy it destroy pathogen by releasing toxic chemicals into interstitial fluid 2 Types of Macrophages • Fixed macrophages - also called histocytes: Microglia: – found in central nervous system Kupffer cells: – found in liver sinusoids • Stay in specific tissues or organs: – e.g., dermis and bone marrow • Free macrophages -Travel through blood stream • Special free macrophages: – alveolar macrophages (phagocytic dust cells) 3 Functional Characteristics of Free Macrophages and Microphages • Move through capillary walls (emigration) • Are attracted or repelled by chemicals in surrounding fluids (chemotaxis) Phagocytosis begins: – when phagocyte attaches to target (adhesion) – and surrounds it with a vesicle Immunological Surveillance is carried out by Natural killer (NK) cells Natural Killer Cell Function Figure 22–11 NK Cell Function • Identifies and attaches to abnormal cell (non-selective) • Golgi apparatus in NK cell: – forms perforin vesicles • Vesicles release perforin (exocytosis) • Perforin lyses abnormal cell membrane NK Cells attack: cancer cells and cells infected with viruses 1) Cancer Cells -with tumor specific antigens: – are identified as abnormal by NK cells – some cancer cells avoid NK cells (immunological escape) 2) Viral Infections : Cells infected with viruses: – present abnormal proteins on cell membranes – allow NK cells to identify and destroy them Interferons • Proteins (cytokines) released by activated lymphocytes and macrophages• Cytokines - Chemical messengers released by tissue cells: – to coordinate local activities – to act as hormones to affect whole body 3 Types of Interferons 1. Alpha interferons: – – produced by leukocytes stimulate NK cells 2. Beta interferons: – – secreted by fibroblasts slow inflammation 3. Gamma interferons: – – secreted by T cells and NK cells stimulate macrophage activity Complement Activation Complement: Plasma contains 11 special complement (C) proteins: that complement antibody action Figure 22–12 Complement Activation • Complements work together in cascades • 2 pathways activate the complement system – classical pathway – alternative pathway The Classical Pathway • Fast method • C1 binds to antibody molecule attached to antigen (bacterium) • Bound protein acts as enzyme: – catalyzes chain reaction The Alternative Pathway • Slow method • Exposed to antigen: – factor P (properdin) – factor B – and factor D interact in plasma • ** Both pathways end with: – conversion of inactive complement protein (C3) – to active form (C3b) 4 Effects of Complement Activation 1. Stimulation of inflammation 2. Attraction of phagocytes 3. Enhancement of phagocytosis by opsonization: – complements working with antibodies (opsonins) 4. Destruction of target cell membranes: – 5 complement proteins join to form membrane attack complex (MAC) Inflammation • Also called inflammatory response • A localized response • Triggered by any stimulus that kills cells or injures tissue Cardinal Signs and Symptoms • • • • Swelling (tumor) Redness (rubor) Heat (calor) Pain (dolor) 3 Effects of Inflammation 1. Temporary repair and barrier against pathogens 2. Retards spread of pathogens into surrounding areas 3. Mobilization of local and systemic defenses: – and facilitation of repairs (regeneration) Inflammation and Tissue Repair Figure 22–13 Inflammation and Tissue Repair • Injured cells release: – prostaglandins – proteins – potassium ions • Changes interstitial environment and stimulates mast cells • Mast cells release: – histamine (increases capillary permeability) – heparin (inhibits clotting Inflammation and Tissue Repair • Increased blood flow: – raises local temperature – causes area to swell, redden, and become painful • Blood clot forms around damaged area, isolating it • Complements: – break down bacteria – attract phagocytes Inflammation and Tissue Repair • Activated neutrophils attack debris and bacteria • Phagocytes and foreign proteins: – activate body’s specific defense system • Macrophages clean up pathogens and cell debris • Fibroblasts form scar tissue Products of Inflammation • Necrosis: – local tissue destruction in area of injury • Pus: – mixture of debris and necrotic tissue • Abscess: – pus accumulated in an enclosed space Fever - A maintained body temperature above 37°C (99°F) • Pyrogens - Any material that causes the hypothalamus to raise body temperature: – circulating pathogens, toxins, or antibody complexes • Endogenous Pyrogens : Interleukin-1 (IL1) – pyrogen released by active macrophages – a cytokine Forms of Immunity Figure 22–14 Specific Defenses • Specific resistance (immunity): – responds to specific antigens – with coordinated action of T cells and B cells T Cells • Provide cell-mediated immunity • Defends against abnormal cells and pathogens inside cells B Cells • Provide antibody-mediated immunity • Defends against antigens and pathogens in body fluids Forms of Immunity • 1) Innate Immunity: – present at birth • 2) Acquired Immunity: – after birth Active: – antibodies develop after exposure to antigen Passive: – antibodies are transferred from another source Active Immunity • Naturally acquired: – through environmental exposure to pathogens • Induced: – through vaccines containing pathogens Passive Immunity • Naturally acquired: – antibodies acquired from the mother • Induced: – by an injection of antibodies 4 Properties of Immunity 1. Specificity- Each T or B cell: – responds only to a specific antigen, ignores all others 2. Versatility-The body produces many types of lymphocytes: – – each fights a different type of antigen (Ag) active lymphocyte clones itself to fight specific Ag 3. Memory-Some active lymphocytes (memory cells): – – stay in circulation provide immunity against new exposure 4. Tolerance- Immune system ignores “normal” antigens What are the differences between cell-mediated (cellular) immunity and antibody-mediated (humoral) immunity? The Immune Response Figure 22–15 (Navigator) The Immune Response • 2 main divisions: – cell mediated immunity (T cells) – antibody mediated immunity (B cells) PLAY Immunity: Cell-Mediated Immunity What are the types of T cells and their functions in the immune response? What are the types of T cells and their functions in the immune response? 1) Cytotoxic T Cells= also called Tc cells • Attack cells infected by viruses • Responsible for cell-mediated immunity 2) Helper T Cells= also called Th cells • Stimulate function of T cells and B cells 3) Suppressor T Cells = also called Ts cells • Inhibit function of T cells and B cells Antigens and MHC Proteins PLAY Antigens and MHC Proteins Figure 22–16a (Navigator) Antigen Recognition • T cells only recognize antigens that are bound to glycoproteins in cell membranes Antigen Presentation Figure 22–16b MHC Proteins • The membrane glycoproteins that bind to antigens • Genetically coded in chromosome 6: – the major histocompatibility complex (MHC) – differs among individuals 2 Classes of MHC Proteins • Class I: found in membranes of all nucleated cells • Pick up small peptides in cell and carry them to the surface: – T cells ignore normal peptides – abnormal peptides or viral proteins activate T cells to destroy cell • Class II: found in membranes of antigen-presenting cells (APCs) – – – – found in lymphocytes Antigenic fragments: from antigenic processing of pathogens bind to Class II proteins inserted in cell membrane to stimulate T cells Antigen-Presenting Cells (APCs) • Responsible for activating T cells against foreign cells and proteins Phagocytic APCs : • Free and fixed macrophages: – in connective tissues • Kupffer cells: – of the liver • Microglia: – in the CNS Pinocytic APCs • Langerhans cells: – in the skin • Dendritic cells: – in lymph nodes and spleen What are the mechanisms of T cell activation and the differentiation of the major classes of T cells? An Overview of the Immune Response Figure 22–15 (Navigator) Antigen Recognition • Inactive T cell receptors: – recognize Class I or Class II MHC proteins – recognize a specific antigen • Binding occurs when MHC protein matches antigen CD Markers • Also called cluster of differentiation markers: – in T cell membranes – molecular mechanism of antigen recognition – more than 70 types: • designated by an identifying number CD3 Receptor Complex • Found in all T cells CD8 Markers • Found on cytotoxic T cells and suppressor T cells • Respond to antigens on Class I MHC proteins CD4 Markers • Found on helper T cells • Respond to antigens on Class II MHC proteins • CD8 or CD4 Markers - Bind to CD3 receptor complex • Prepare cell for activation Costimulation • For T cell to be activated, it must be costimulated: – by binding to stimulating cell at second site – which confirms the first signal 2 Classes of CD8 T Cells • Activated by exposure to antigens on MHC proteins: – one responds quickly: • producing cytotoxic T cells and memory T cells – the other responds slowly: • producing suppressor T cells Activation of Cytotoxic T Cells Also called killer T cells Seek out and immediately destroy target cells Figure 22–17 (Navigator) Actions of Cytotoxic T Cells 1. Release perforin: – to destroy antigenic cell membrane 2. Secrete poisonous lymphotoxin: – to destroy target cell 3. Activate genes in target cell: – that cause cell to die Slow Response • Can take up to 2 days from time of first exposure to an antigen, for cytotoxic T cells to reach effective levels Memory Tc Cells • Produced with cytotoxic T cells • Stay in circulation • Immediately form cytotoxic T cells: – if same antigen appears again Suppressor T Cells • • • • Secrete suppression factors Inhibit responses of T and B cells After initial immune response Limit immune reaction to single stimulus Activation of Helper T Cells Helper T Cells Activated CD4 T cells divide into: active helper T cells: secrete cytokines memory T cells: remain in Figure 22–18 4 Functions of Cytokines 1. Stimulate T cell divisions: – – produce memory T cells accelerate cytotoxic T cell maturation 2. Attract and stimulate macrophages 3. Attract and stimulate NK cells 4. Promote activation of B cells Pathways of T Cell Activation Figure 22–19 KEY CONCEPT • Cell-mediated immunity involves close physical contact between activated Tc cells and foreign, abnormal or infected cells • T cell activation usually involves: – antigen presentation by phagocytic cell – costimulation by cytokines from active phagocytes • Tc cells may destroy target cells through local release of cytokines, lymphotoxins, or perforin What are the mechanisms of B cell activation and the differentiation of plasma cells and memory B cells? B Cells • Responsible for antibody-mediated immunity • Attack antigens by producing specific antibodies • Millions of populations, each with different antibody molecules PLAY Immunity: Antibody-Mediated Immunity B Cell Sensitization • Corresponding antigens in interstitial fluids bind to B cell receptors • B cell prepares for activation • Preparation process is sensitization B Cell Sensitization and Activation During PLAY sensitization, antigens are: taken into the B cell, processed, reappear on surface, bound to Class II MHC protein Figure 22–20 (Navigator) Helper T Cells • Sensitized B cell is prepared for activation, but needs helper T cell activated by same antigen B Cell Activation • Helper T cell binds to MHC complex: – secretes cytokines that promote B cell activation and division B Cell Division • Activated B cell divides into: – plasma cells -Synthesize and secrete antibodies into interstitial fluid Memory B cells- Like memory T cells remain in reserve to respond to next infection Antibody Structure What is the structure of an antibody, and what types of antibodies are found in body fluids and secretions Figure 22–21a, b Antibody Structure • 2 parallel pairs of polypeptide chains: – 1 pair of heavy chains – 1 pair of light chains • Each chain contains: – constant segments – variable segments-Determine specificity of antibody molecule 5 Heavy-Chain Constant Segments • Determine 5 types of antibodies: – – – – – IgG IgE IgD IgM IgA Binding Sites • Free tips of 2 variable segments: – form antigen binding sites of antibody molecule – which bind to antigenic determinant sites of antigen molecule Antibody Function •Antigen–Antibody Complex = An antibody bound to an antigen Figure 22–21c, d A Complete Antigen • Has 2 antigenic determinant sites • Binds to both of antigen binding sites of variable segments of antibody • Exposure to a complete antigen leads to: – B cell sensitization – immune response A Hapten • Also called partial antigen • Must attach to a carrier molecule to act as a complete antigen Dangers of Haptens • Antibodies produced attack both hapten and carrier molecule • If carrier is “normal”: – antibody attacks normal cells – e.g., penicillin allergy 5 Classes of Antibodies Table 22–1 5 Classes of Antibodies • • • • Also called immunoglobins (Igs) Are found in body fluids Are determined by constant segments Have no effect on antibody specificity 7 Functions of Antigen–Antibody Complexes 1. Neutralization of antigen binding sites 2. Precipitation and agglutination: – formation of immune complex 3. Activation of complement 4. Attraction of phagocytes 5. Opsonization: – increasing phagocyte efficiency 6. Stimulation of inflammation 7. Prevention of bacterial and viral adhesion KEY CONCEPT • Antibody-mediated immunity involves the production of specific antibodies by plasma cells derived from activated B cells • B cell activation usually involves: – antigen recognition, through binding to surface antibodies, costimulation by a Th cell • Antibodies produced by active plasma cells bind to target antigen and: – inhibit its activity or destroy it – remove it from solution – promote its phagocytosis by other defense cells Primary and Secondary Responses • Occur in both cell-mediated and antibody-mediated immunity Figure 22–22 Primary and Secondary Responses to Antigen Exposure • First exposure: – produces initial response (Primary) • Next exposure: – triggers secondary response – more extensive and prolonged – memory cells already primed The Primary Response • • • • • Takes time to develop Antigens activate B cells Plasma cells differentiate Antibody titer slowly rises Peak response: – can take 2 weeks to develop – declines rapidly • IgM: – is produced faster than IgG – is less effective The Secondary Response • Activates memory B cells: – at lower antigen concentrations than original B cells – secrete antibodies in massive qualities Effects of Memory B Cell Activation • IgG: – rises very high and very quickly – can remain elevated for extended time • IgM: – production is also quicker – slightly extended KEY CONCEPT • Immunization produces a primary response to a specific antigen under controlled conditions • If the same antigen appears at a later date, it triggers a powerful secondary response that is usually sufficient to prevent infection and disease Summary of the Immune Response • Specific and nonspecific defenses Figure 22–23 Body Responses to Bacterial Infection Figure 22–24 Combined Immune System Responses Figure 22–25 Combined Responses to Bacterial Infection • Neutrophils and NK cells begin killing bacteria • Cytokines draw phagocytes to area • Antigen presentation activates: – helper T cells – cytotoxic T cells • B cells activate and differentiate • Plasma cells increase antibody levels Combined Responses to Viral Infection • Similar to bacterial infection • But cytotoxic T cells and NK cells are activated by contact with virusinfected cells Summary: Cells of the Immune System Table 22–2 KEY CONCEPT • Viruses replicate inside cells, whereas bacteria may live independently • Antibodies (and administered antibiotics) work outside cells, so are primarily effective against bacteria rather than viruses • Antibiotics cannot fight the common cold or flu • T cells, NK cells, and interferons are the primary defense against viral infection What is the origin, development, activation, and regulation of normal resistance to disease? Immune System Development • Fetus can produce immune response or immunological competence: – after exposure to antigen – at about 3–4 months Development of Immunological Competence • Fetal thymus cells migrate to tissues that form T cells • Liver and bone marrow produce B cells • 4-month fetus produces IgM antibodies Before Birth • Maternal IgG antibodies: – pass through placenta – provide passive immunity to fetus After Birth • Mother’s milk provides IgA antibodies: – while passive immunity is lost Normal Resistance • Infant produces IgG antibodies through exposure to antigens • Antibody, B-cell, and T-cell levels slowly rise to adult levels: – about age 12 Hormones of the Immune System Table 22–3 6 Groups of Hormonal Cytokines 1. 2. 3. 4. Interleukins Interferons Tumor necrosis factors Chemicals that regulate phagocytic activities 5. Colony stimulating factors 6. Miscellaneous cytokines What are the origins of autoimmune disorders, immunodeficiency diseases, and allergies, and what are some examples of each? Immune Disorders • Autoimmune disorders- A malfunction of system that recognizes and ignores “normal” antigens Activated B cells make autoantibodies against body cells • Immunodeficiency diseaseThyroiditis Rheumatoid arthritis Insulin-dependent diabetes mellitus • Allergies - Immunodeficiency Diseases 1. Problems with embryological development of lymphoid tissues: – can result in severe combined immunodeficiency disease (SCID) 2. Viral infections such as HIV: – can result in AIDS 3. Immunosuppressive drugs or radiation treatments: – can lead to complete immunological failure Allergies • Inappropriate or excessive immune responses to antigens • Allergens: – antigens that trigger allergic reactions 4 Categories of Allergic Reactions • Type I: – immediate hypersensitivity • Type II: – cytotoxic reactions • Type III: – immune complex disorders • Type IV: – delayed hypersensitivity Type I Allergy (1) • Also called immediate hypersensitivity • A rapid and severe response to the presence of an antigen • Most commonly recognized type of allergy • Includes allergic rhinitis (environmental allergies) • Sensitization leads to: – production of large quantities of IgE antibodies – distributed throughout the body • Second exposure leads to: – massive inflammation of affected tissues Type I Allergy (2) • Severity of reaction depends on: – individual sensitivity – locations involved • Allergens in blood stream may cause anaphylaxis Anaphylaxis • Can be fatal • Affects cells throughout body • Changes capillary permeability: – produce swelling (hives) on skin • Smooth muscles of respiratory system contract: – make breathing difficult • Peripheral vasodilatation: – can cause circulatory collapse (anaphylactic shock) Antihistamine Drugs • Block histamine released by MAST cells • Can relive mild symptoms of immediate hypersensitivity Stress and the Immune Response • Glucocorticoids: – secreted to limit immune response – long-term secretion (chronic stress): • inhibits immune response • lowers resistance to disease Functions of Glucocorticoids • Depression of the inflammatory response • Reduction in abundance and activity of phagocytes • Inhibition of interleukin secretion Aging and the Immune Response • Immune system deteriorates with age, increasing vulnerability to infections and cancer 4 Effects of Aging on Immune Response 1. Thymic hormone production: – greatly reduced 2. T cells: – become less responsive to antigens 3. Fewer T cells reduce responsiveness of B cells 4. Immune surveillance against tumor cells declines Integration with Other Systems Nervous and Endocrine Systems Interact with thymic hormones Adjust sensitivity of immune Figure 22–27 Disorders of the Lymphatic System • 3 categories affect immune response: – disorders resulting from: • an insufficient immune response • an inappropriate immune response • an excessive immune response SUMMARY (1) • Divisions of the lymphatic system: – lymphatic vessels (lymphatics) – lymph – lymphoid tissues and organs • Types of lymphocytes: – T cells – B cells – NK cells • Lymphoid tissues and organs: – Nodules – MALT – spleen nodes thymus SUMMARY (2) • 7 nonspecific defenses: – – – – – – – physical barriers phagocytes immunological surveillance interferons complement inflammation fever SUMMARY (3) • Specific defenses: – cell-mediated immunity – antibody mediated immunity • Forms of immunity: – innate or acquired – active or passive • Properties of immunity: – specificity, versatility, memory, andtolerance SUMMARY (4) • T cells and cell-mediated immunity: – – – – – antigen presentation MHCs and APCs antigen recognition CD8 T cell activation CD4 T cell activation SUMMARY (5) • B cells and antibody-mediated immunity: – – – – – sensitization plasma cells and memory B cells antibody structure antigen–antibody complex 5 classes of immunoglobins SUMMARY (6) • Primary and secondary responses to antigen exposure • Hormones and the immune system: – interleukins, interferons, TNFs, and CSFs • Immune disorders • Effects of aging on the immune response