Immunology Stack
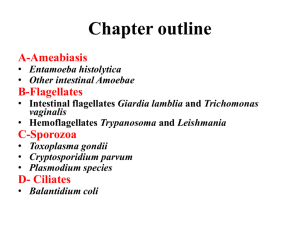
advertisement

Parasitic Protozoa Slackers Facts by Mike Ori Disclaimer The information represents my understanding only so errors and omissions are probably rampant. It has not been vetted or reviewed by faculty. The source is our class notes. The document can mostly be used forward and backward. I tried to mark questionable stuff with (?). If you want it to look pretty, steal some crayons and go to town. Finally… If you’re a gunner, buck up and do your own work. What are the three related sporozoans? Toxoplasmosis Cryptosporidium Plasmodia What is the definitive host for toxoplasmosis? What are the routes of acquisition for toxoplasmosis? 1. Ingestion of undercooked meat especially lamb and pork (vive la France) 2. Cat feces 3. Vertical Explain when toxo is a concern during transplant When a seropositive donor heart is transplanted into a seronegative recipient What results from post transplant infection Myocarditis What sx would you expect to see in aids pt Ring enhancing lesions in the brain Since toxo increases in aids pt, what type of immunity is likely to play a role in toxo control? Cell mediated immunity What is the source of toxo in aids pt Usually reactivated encysted (bradyzoites) organisms What is a common source of diarrhea in PT with low CD4+ counts? Cryptosporidium Describe the disease course in immunocompetent and immunocompromised pt Competent: incubation < 2 weeks with 1 week sx. Immunocompromised: long term diarrhea What is the treatment for cryptosporidium in immunocompromised pt Raise the CD4 count. What organism could cryptosporidium be mistaken for in “regular stains”? Candida How do you differentiate cryptosporidium from candida Crypto is acid fast, Candida is not Why is crypto hard to treat The organisms invades the ciliated surface and sits in an intracellular but extracytoplasmic location. This limits access to antimicrobial agents. Describe Girardia morphology Flagellated pear shaped organisms with two nuclei and a concave sucking disk Describe Giardia epidemiology Outdoorsy people that drink from streams without properly treating the water. What are girardia’s sx? Most are asymptomatic. Those that have sx experience loose foul smelling stools, abdominal ramps, bloating, weight loss. Explain how Girardia attaches to the host It uses its ventral sucking disk for attachment. How many nuclei does the encysted Giarardia have Quattro Which test is more sensitive, O and P or fluorescent antibodies, or ELISA O and P is not very sensitive especially if the small intestine is colonized. O and P is repeated three. Three tests are typically done. FA and ELISA are much more sensitive and usually yield results in one test. What is the string test? PT’s with small intestinal disease swallow the end of a string overnight in an effort to trap organisms in the string for detection. What is metabolically unique about anaerobic protozoans? They do not synthesize nucleotides Name three anaerobic protozoans Girardia, Entamoeba, Trichomonas Describe the SX with Entamoeba infection Bloody diarrhea When is Entamoeba infection not a clinical problem Entamoeba dispar is a frequent colonizer but is not known to cause disease. E. histolytica is only a problem if its invasive. What is the evidence for invasion with E. histolytica? RBC’s ingestion How are E. dispar and E. histolytica differentiated? By PCR What colon morphology is indicative of amoebiasis Inverted flask shaped ulcers. What is the reservoir for Entamoeba E. Histolytica = human What other organs are involved with Entamoeba and what are the findings Liver can be involved with anchovy paste filled cysts. Organisms will be on the periphery of the cyst. Describe the sx for trichomonas vaginalis in men and women Men are usually asymptomatic Women will usually have a foul smelling green discharge How is Trichmonas vaginalis transmitted? By sexual contact Women How is enamoeba transmitted? Food > water How is Girardia transmitted? Water > food What is the reservoir for Girardia in the wild Reservoir = beaver = reservoir builder What disease does plasmodium cause Malaria Name the plasmodium species P. vivax P. ovale P. malariae P. falciparum Which species is associated with the most deaths? P. falciparum What is the route of transmission for Plasmodium Anopheles What is the definitive host for malaria Mosquitoes What is injected into humans by said mosquito? A malaria sporozoite Where do the sporozoites go The liver What is a schizont The replicating malarial mass in a hepatocyte or RBC What is a malaria trophozoite? Something less than a schizont but more than a merizoite. Why does malaria fever come in 2-3 day intervals? The release of the merizoites from RBC’s is fairly well coordinated and occurs in a large burst. This exposes the organism to the immune system and causes a fever. The merizoites then go on to infect more RBC’s thus causing a cycle. When might the fever cycle degenerate? P. falciparum tends to degenerate. Multiple infection cycles also tend to degenerate What are the unique histological features of P. falciparum? Schizont forms tend to lodge in the microvasculature and so are not seen on routing blood smears. In addition, more ring forms and double infected RBC’s are seen in P. falciparum What is sequestration The action of retaining shizonts in the microvasculature. This prevents removal by the spleen. What is unique about the life cycle of P. vivax and P. ovale? They can have latent hepatic stages that can release merizoits months to years later. This is in contrast to P. falciparum and P. malariae which release all their merizoites from the liver in a single go. Which blood cells does P. vivax invade? It only invades reticulocytes. What is the role of receptors in malarial disease Merizoites interact with species specific receptors on the RBC surface. For instance P. vivax required Duffy and reticulocyte receptor Where are receptors located on merizoites In a special organelle called the rhoptry Explain the high incidence of sickle cell trait and the low incidence of Duffy in west Africa Sickle cell trait is protective for severe malaria. Absence of Duffy prevents P. vivax invasion of reticulocytes. Note there are other examples in the notes. Explain the belief that the immune response to malaria is incomplete Mortality is highest in naïve pt (children mostly in endemic areas). Adults can carry a high parasitemia with little sx and thus seem to be protected from severe disease. What are the run of the mill sx for malaria High fever (40-41c) Chills Headache What is the typical causative species for severe malaria? P falciparum What are the sx of severe malaria Cerebral malaria – seizures and coma due to cerebral sequestration Severe anemia (Hgb < 5) – falciparum can have very high infectivity General illness – prostration, hypoglycemia, lactic acidosis, ARDS What is chronic malaria Continuous parasitemia in contrast to recurring parasitemia What is the causitive agent for chronic malaria P. falciparum and P. vivax What are the methods to prevent malaria Repellents Mosquito netting Clothing Prophylactic pharmacology List the malaria time course Prepatent (hepatic) phase – 2 weeks Red cell phase – 2-3 days What is the vector for leishmania Sand flies What is an amastigote and a promastigote? A mastigote = amotile (I.e. no flagella) Promastigote = pretty good swimmer (flagellated) What cell is invaded by promastigotes Macrophages What is the result for the macrophage? Eventual lysis of the cell due to replication What are the three types of leishmaniasis? Cutaneous Mucocutaneous Visceral Diffuse cutaneous Describe cutaneous leishmaniasis Ulcerative lesions that eventually heal with no sequelae Describe mucocutaneous leishmaniasis Cutaneous lesions heal but later destruction of nasal and mucosal tissue occurs Describe visceral leishmaniasis Invasion of the liver and other visceral leading to death Describe diffuse cutaneous leishmaniasis Treatment resistant non-ulcerative lesions disseminated over the skin surface. Very tx resistant. Describe the African Trypanosoma brucei species ranges Roughly divided into east and west african What is the vector from Trypanosoma brucei The tsetse fly Describe the hosts for both species West = human East = big game animals with humans as incidental What are the stages of african trypanosomal disease 1. Bite/chancre 2. Hemolymphatic – Lymphadenopathy with relapsing fever 3. Meningoencephalitis – somnolence, coma, death Why does the immune system fail to clear trypanosomes The organisms express variant surface glycoproteins that cause antigenic variation Describe the progression of T.b rhodesiense and T.b. ghambiense Tbr is east african and is much more acute. Death occurs in months. Tbg is west african and is less acute. Death occurs on years How is tx complicated with CNS diease Tx of CNS disease relies on arsenic containing compounds which are toxic to the host. What is the vector for Trypanosoma cruzi The reduviid bug How is T. cruzi spread? The reduviid bug bites a victim causing a pruritis. The bug also deposits trypanosome laden feces near the bite. The host then scratches the bite, mechanically introducing the organism. The organism can also pass directly across mucosal surfaces. What is unique about the epithelial invasion of T. cruzi It invades epithelial cells at point of cell to cell junction. What are the sx of chagas disease Nerve destruction Muscle inflammation and hypertrophy Leading to dilated cardiomyopathy, arrhythmia, and GI tract dilation and esophageal impairment (dysphagia, odynophagia) What are the phases of chagas disease Acute Indeterminate Chronic What is Romana’s sign Periorbital edema caused by T cruzi entry across the eye mucosa. What is the cause of most deaths from chronic chagas disease? Cardiac disease What is meant by indeterminate disease Chagas disease may enter a latent phase that can lead to acute flares, continued latency, or chronicity. There is no way to predict the outcome. Which phases of chagas disease are treatable? Acute is treatable. Indeterminate and chronic do not benefit from treatment.