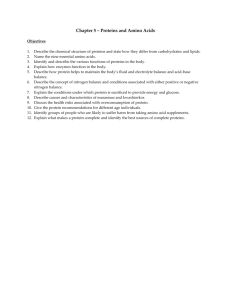
branched chain amino acid
advertisement

Ammonium 0. 1 – 1.5 g Buffering the urine 1 AMINO ACID METABOLISM • Amino acids are required for the synthesis of proteins, peptides, nucleotides, neurotransmitters, other amino acids • Free amino acids can be provided to cells either from the digestion of dietary proteins or the degradation of defective or aged cellular proteins • Amino acids are catabolized into components that can directly join energy production pathways or be changed to glucose, fatty acids or ketone bodies; this happens: when the amount of amino acids obtained from digestion and degradation is more than what is needed for biosynthesis during starvation or uncontrolled diabetes mellitus • The catabolism of amino acids produces: amino group – removed as urea carbon skeleton – seven types of intermediates 2 • o • • • • The digestion of proteins The digestion of proteins begins in the stomach and continues in the small intestine Please refer to the notes on enzymes for the types, activation and specificity of the proteases involved in the digestion Rennin (chymosin) is important in infants because it breaks a specific peptide bond in casein (a milk protein) curdling the milk and increasing transit time in the stomach Proteases can be endopeptidases or exopeptidases The endopeptidases are specific for different types of peptide bonds and produce fragments of varying sizes Exopeptidases take over the job: carboxypeptidase A and B – produced by the pancreas and cleave at the C-terminal brush border aminopeptidases – act on the N-terminal of oligopeptides yielding free amino acids and di- and tripeptides 3 4 • Digestive enzymes themselves are digested and contribute to the amino acid pool • Free amino acids are transported into intestinal epithelial cells by Na+ - dependent secondary transport • Di- and tripeptides enter the epithelial cells through symport with H+ the H+ gradient is maintained by the Na+ - H+ exchanger peptidases in the epithelial cells change the di- and tripeptides into free amino acids • Amino acids enter the portal vein by facilitated transport • Many cells use Na+ - dependent secondary transport and to some extent facilitated transport in order to absorb amino acids o premature activation of zymogens inside the pancreas 5 results in acute pancreatitis 6 • • • • • • Protein turnover The degradation and resynthesis of proteins The half-lives of eukaroytic proteins may vary from 30 seconds to many days ornithine decarboxylase – approx. 11 minutes; hemoglobin – lifespan of red blood cells; crystallin (lens protein) – life span of the organism Rapidly degraded proteins include those proteins that are defective due to wrong insertion of amino acids or damage accumulated during normal functioning, regulatory enzymes, A protein's half-life correlates with its N-terminal residue Proteins with N-terminal Met, Ser, Ala, Thr, Val or Gly have half lives greater than 20 hours Proteins with N-terminal Phe, Leu, Asp, Lys or Arg have half lives of 3 min or less 7 • PEST proteins having domains rich in Pro (P), Glu (E), Ser (S) and Thr (T) are more rapidly degraded than other proteins • There are two ways of intracellular degradation of proteins 1. lysosomal degradation - of endocytosed proteins or proteins undergoing autophagy • In autophagy, part of the cytoplasm may become surrounded by two concentric membranes • Fusion of the outer membrane of this autophagosome with a lysosomal vesicle results in the degradation of enclosed cytoplasmic structures and macromolecules • the enzymes responsible for the degradation are cathepsins autophagosome autophagic vacuole 8 (lysosome) 2. • • • ATP- dependent cytosolic degradation The ubiquitin – proteasome pathway Ubiquitin is a small protein having 76 amino acids only It is present in all eukaryotes (hence the name) and its amino acid sequence is highly-conserved • Ubiquitin marks proteins for death the carboxyl terminal of a ubiquitin forms an isopeptide bond with the ε-amino group of a lysine residue of a protein to be destroyed • Three enzymes, are involved in the attachment of ubiquitin: Initially the terminal carboxyl group of ubiquitin is joined in a thioester bond to a cysteine residue on Ubiquitin-Activating Enzyme (E1) ; this is an ATPdependent process 9 The ubiquitin is then transferred to a sulfhydryl group on a Ubiquitin-Conjugating Enzyme (E2) Ubiquitin-Protein Ligase (E3) then promotes the transfer of ubiquitin from E2 to the ε-amino group of a Lys residue of a protein recognized by that E3 • The substrate-specificity of this system comes from the various combinations of the types of E2 and E3 • More ubiquitins are added to form a polyubiquitin chain The terminal carboxyl of each ubiquitin is linked to the ε-amino group of a lysine residue (Lys 29 or Lys 48) of the adjacent ubiquitin A chain of 4 or more ubiquitins targets proteins for degradation in proteasomes 10 11 • The proteasome is a complex of multiple proteases • Constitutes nearly 1 % of cellular protein • It contains two main types of subcomplexes: a barrel-like core particle (20S) and regulatory 19S particles on both ends of the barrel the catalytic core particle and the regulatory particles make up the functional 26S proteasome • The 19 S particles may unfold proteins and translocate the unfolded proteins into the 20 S particle; energy from ATP is consumed in the process • The 19 S particles also cleave isopeptide bonds and free ubiquitin; ubiquitin is recycled • The protein is degraded by the 20 S particle and free amino acids are released into the cellular space 12 13 • Proteasomal degradation of particular proteins is an essential mechanism by which cellular processes are regulated, such as cell division, apoptosis, differentiation and development progression through the cell cycle is controlled in part through regulated degradation of proteins called cyclins that activate cyclin-dependent kinases • Inability to degrade proteins that activate cell division (or rapid degradation of those proteins that suppress tumor formation) can lead to cancer • Diseases like Alzheimer's, Parkinson’s , type II diabetes,… are associated with the deposition on tissues of non-degradable protein aggregates known as amyloid 14 The catabolism of amino acids The fate of amino acid nitrogen • α-amino groups are removed from amino acids mostly through transamination reactions the amino acid becomes a keto acid when it donates the amino group to α-ketoglutarate (changing it to glutamate) • All amino acids except lysine and threonine undergo transamination reactions • The enzymes involved are known as transaminases or aminotransferases • Pyridoxal phosphate (PLP) is the cofactor • The glutamate thus derived collects the amino groups and gives them off for biosynthesis or excretion 15 16 H C R COO EnzLysNH2 Enz (CH2)4 NH2 Amino acid HC P O O O N H CH3 Enzyme (Lys)-PLP Schiff base O EnzLysNH2 CH2 O H2 C P O NH2 R C CH3 Pyridoxamine phosphate H2 C P O HC O O OH N H R H C COO N+ α-keto acid O CH3 Amino acid-PLP Shiff base (aldimine) EnzLysNH2 COO O O O N H COO H H2 C P HC O O H H2 C H C N+ N+ O O O R H O O N H CH3 17 Amino acid-PLP Shiff base (aldimine) • Free ammonium can be released in different ways: A. The oxidative deamination of glutamate by glutamate dehydrogenase - the only enzyme that can use NAD+ or NADP+ as electron acceptor The reaction is reversible and takes place in the mitochondria B. Serine and threonine dehydratases release NH4+; histidine can be directly deaminated to give NH4+ C. Intestinal bacteria produce NH4+ from amino acids or urea; the ammonia enters the portal vein D. Glutamine and asparagine lose their side chain amino groups through deamidation E. The purine nucleotide cycle in the brain – aspartate is used as a substrate and fumarate and ammonium are18 released 19 • • • • • • • The urea cycle Nitrogen balance is the difference between the amount of nitrogen consumed and excreted per day Positive nitrogen balance in growing individuals Negative nitrogen balance during protein deficiency or starvation In healthy adults, the amount of nitrogen consumed and excreted is approximately equal Nitrogen is excreted in the form of urea, uric acid, ammonium, creatinine, hippurate, creatine Humans are ureotelic (excrete excess nitrogen mainly in the form of urea) ammonotelic (ammonia); uricotelic (uric acid) Ammonium made available in the liver from different sources enters the urea cycle 20 • Since the enzymes of the urea cycle are present in the liver only, amino groups from other tissues should be transported to the liver • Two mechanisms of transport: 1.the skeletal muscles export alanine synthesized from the transamination of pyruvate (glucose catabolism) by glutamate the amino group donated by glutamate was obtained from the breakdown of amino acids in the muscle 21 2. Glutamate can accept another amino group through an ATPdependent reaction catalyzed by glutamine synthetase Glutamine is used by most tissues to transport ammonium Glutamine travels to the liver, kidneys and the intestine and is deamidated the ammonium released by the deamidation is used as a buffer (in the kidneys) or enters the urea cycle in the liver; glutamine can be used as an energy source by the intestine 22 o The two nitrogen atoms of urea enter the urea cycle as NH4+ and as the amino N of aspartate 1. The synthesis of carbamoyl phosphate • The NH4+ and HCO3- (carbonyl C) that will be part of urea are incorporated first into carbamoyl phosphate The cleavage of 2 ATP molecules is needed to form the high energy carbamoyl phosphate Carbamoyl phosphate synthetase (CPS I) is a mitochondrial enzyme; the cytosolic isozyme is involved in pyrimidine synthesis • CPS I has an absolute requirement for the allosteric activator N-acetylglutamate • This derivative of glutamate is synthesized from acetyl-CoA and glutamate when cellular glutamate is high, signaling an excess of free amino acids due to protein breakdown or 23 dietary intake 2. The formation of citrulline • Carbamoyl phosphate reacts with ornitihine to give citrulline; catalyzed by ornithine transcarbamoylase 3. The entry of the second N • Citrulline leaves the mitochondria in exchange for the entry of ornithine from the cytosol • Citrulline reacts with aspartate producing argininosuccinate • Argininosuccinate synthetase requires the splitting of ATP to 24 AMP and PP + + Pi ornithine transcarbamoylase ATP AMP+ PPi argininosuccinate synthetase 25 4. The formation of arginine • Argininosuccinate lyase produces arginine and fumarate • The arginine produced by the urea cycle is enough for adults • The carbons of fumarate are those that were obtained from aspartate Fumarate be changed to oxaloacetate by enzymes of the citric acid cycle The oxaloacetate will receive an amino group from glutamate and be changed to aspartate; aspartate reenters the urea cycle The TCA and urea cycles constitute a bicycle: The Krebs bicycle 5. The production of urea and the regeneration of ornithine • The action of arginase produces urea and ornithine 26 • Urea travels to the kidneys and excreted through the urine argininosuccinase + 27 The urea cycle 28 The Krebs bicycle The stocihiometry of the urea cycle NH4++ CO2 + 3 ATP+ 2H2O→urea + fumarate + 2 ADP + AMP+ 4Pi 29 In addition to the allosteric effects of N-acetylglutamate, the synthesis of the enzymes of the urea cycle can be induced during periods of increased metabolism – protein rich diet or prolonged fasting Urea cycle abnormalities • Hereditary deficiency in any one of the urea cycle enzymes or liver cirrhosis lead to the increase in the blood of ammonia (hyperammonemia) or urea cycle intermediates • The total lack of any urea cycle enzyme is lethal • Elevated ammonia is toxic, especially to the brain • Why is ammonia toxic to the brain? Hypotheses: 1. High ammonia levels would drive glutamine synthetase; this would deplete glutamate – a neurotransmitter and precursor for the synthesis of GABA • Glutamine may exert osmotic effects leading to the swelling of the brain 30 2. Depletion of glutamate and high ammonia levels would drive the glutamate dehydrogenase reaction in the reverse direction; the resulting depletion of α-ketoglutarate, inhibits the production of energy The treatment of urea cycle defects • limiting protein intake to the amount barely adequate to supply amino acids for growth, while adding to the diet the αketo acids of essential amino acids • liver transplantation; gene therapy has also been tried • If the defect occurs after the synthesis of argininosuccinate, argininosuccinate can be used as a carrier for the removal of nitrogen (because it has incorporated both amino groups) the problem in this situation would be one of regenerating ornithine If arginase is not deficient, the intake of high amounts of arginine would provide ornithine 31 • If the defect occurs at a point before the synthesis of argininosuccinate, substances are used that form conjugates with amino acids and are excreted in the urine The body has to use ammonia to replace the excreted amino acids; ammonia levels decrease Drugs: Benzoic acid - reacts with glycine to give hippurate Phenylbutyrate - first changed to phenylacetate and then reacts with glutamine to produce phenylacetylglutamine • The most common defect is in ornithine transcarbamoylase • In the rare cases of arginase deficiency, arginine should be excluded from the diet • Deficiency of N-acetyl glutamate can be corrected by administering an analog, carbamoyl glutamate 32 33 • • • • • • The fate of the carbon skeleton of amino acids The deamination of most amino acids yields α- keto acids that, directly or via additional reactions, feed into major metabolic pathways Amino acids are grouped into two classes based on whether or not their carbon skeletons can be converted to glucose: glucogenic or ketogenic Carbon skeletons of glucogenic amino acids are degraded to pyruvate or a 4-C or 5-C intermediates of the Krebs cycle Glucogenic amino acids are a major carbon source for gluconeogenesis when glucose levels are low They can also be catabolized for energy production or converted to glycogen or fatty acids for energy storage Carbon skeletons of ketogenic amino acids are degraded to acetyl-CoA or acetoacetate 34 • Carbon skeletons of ketogenic amino acids can be catabolized for energy or converted to ketone bodies or fatty acids • leucine and lysine are strictly ketogenic • isoleucine, threonine, phenylalanine, tyrosine and tryptophan and both glucogenic and ketogenic • The remaining thirteen amino acids are glucogenic amino acids producing pyruvate can be considered ketogenic because pyruvate can be changed to acetyl-CoA • One carbon transfer is a common theme in amino acid metabolism • Three cofactors are used to transfer different one carbon groups between intermediates Tetrahydrofolate (THF); S-adenosylmethionine/SAM/adoMet; Vitamin B 12 (5’-deoxyadensoyl/methyl cobalamin) o Biotin is involved in the transfer of the most oxidized form of 35 carbon – CO2 36 • • • • • • Tetrahydrofolate Folic acid/folate/folacin is composed of a pteridine nucleus, para amino benzoic acid and one or more glutamic acid residues Once folic acid is absorbed by the intestine, it is converted to the biologically active form, tetrahydrofolate , by dihydrofolate reductase only one glutamic acid remains; 4 hydrogens added THF travels to the liver and glutamic acid residues are added Most of the THF is released into the bile and recirculates just like the bile acids The carbon units carried by THF are attached to N5 and/or N10 of the pteridine ring One carbon units carried by THF are: Most reduced: - CH3 (methyl) Intermediate: - CH2 - (methylene) Most oxidized: - CHO (formyl) - CHNH (formimino) 37 - CH = (methenyl) 38 • The collection of one carbon units attached to THF is known as the one – carbon pool • While they are still attached to THF, the one carbon units can be oxidized or reduced • The main source of carbon units for THF is the carbon removed during the conversion of serine to glycine producing N5, N10-methylene THF • Although THF can carry a methyl group at N5, the transfer potential of the methyl group is insufficient for most biosynthetic reactions; another cofactor is used as a carrier of methyl groups S-adenosyl methionine • It contains an activated methyl thioether group; donates methyl groups to oxygen or nitrogen • Its synthesis to be discussed under the synthesis of cysteine 39 • • • • • • Vitamin B 12 The unmodified form of vitamin B 12 is known as cobalamin It has a corrin ring similar to porphyrin but unlike porphyrin two of its pyrrole rings are joined directly (no bridges); cobalt takes the place of iron Cobalamin in the diet can be found in a free form or bound with proteins Free cobalamin is then bound by salivary or gastric secretions known as haptocorrins; protein-bound cobalamin is first freed of the proteins and then haptocorins bind it Haptocorin bound cobalamin is changed to free cobalamin in the intestine Cobalamin is then bound by intrinsic factor which assists in the absorption into the intestine; travels to the liver bound with transcobalamin II 40 • Vitamin B 12 is involved in two reactions in the body: 1. The intramolecular rearrangement of a proton during the formation of succinyl-CoA from propionyl-CoA the coenzyme form of vitamin B 12 used in this case is 5’- deoxy -adenosyl cobalamin – 5’- deoxyadenosine attached to cobalt 2.The regeneration of methionine (to be discussed) 41 methyl is attached to cobalt to give methyl cobalamin X = 5’- deoxyadenosine or methyl 42 43 • • • • Essential and non-essential amino acids Eleven amino acids are considered to be non-essential because they can be synthesized in the body arginine, cysteine, tyrosine and histidine are conditionally essential Arginine and histidine needed in the diet of children and pregnant women; in adults arginine from the urea cycle is enough and histidine is effectively recycled tyrosine and cysteine are synthesized from the essential amino acids phenylalanine and methionine, respectively; if these precursors are absent in the diet, then the products become essential The remaining essential amino acids are lysine, leucine, isoleucine, valine, tryptophan, threonine and histidine Except tyrosine and cysteine, essential amino acids can be synthesized from glucose and ammonia (or another amino acid) 44 Amino acids related with intermediates of glycolysis • In the synthesis of serine, 3-phosphoglycerate is sequentially oxidized, transaminated and dephosphorylated • In addition to the serine dehydratase reaction, serine can be changed to pyruvate through transamination followed by reduction and phosphorylation to give PEP (PEP then changed to pyruvate) • The main pathway of glycine synthesis is from serine – serine hydroxymethyl transferase catalyzes the reaction which involves PLP and N5, N10 methylene THF Glycine can be degraded by changing it to serine and then to pyruvate A second way for the degradation of glycine is the production of glyoxylate by D-amino acid oxidase D-amino oxidase is thought to act in the detoxification of D-amino acids from bacteria or cooked foodstuffs 45 46 47 • Glyoxylate can react with α- ketglutarate and be directed to energy production • It can also be oxidized to oxalate by hepatic lactate dehydrogenase • This oxalate, along with the oxalate obtained from the diet, contribute to the formation of kidney stones 3/4th of kidney stones is composed of calcium oxalate • The third and major approach to degrading glycine is by glycine cleavage enzyme Glycine degraded to NH4+, CO2 and –CH2– (carried by THF) If glycine cleavage enzyme is deficient, non-ketotic hyperglycinemia results; mental retardation and early death probably due to the increased inhibitory effects of glycine on the nervous system 48 • The carbon skeleton and the amino group of cysteine are derived from serine; the sulfur is transferred from methionine • The sulfur of methionine attacks the 5’ carbon of the ribose of ATP releasing all the three phosphates in the process; SAM (Ado met) is the product • SAM donates CH3 and becomes S-adenosylhomocysteine • The hydrolytic removal of the adenosine gives homocysteine • Serine reacts with homocysteine to give cystathionine – catalyzed by cystathionine-β –synthase • Cystathionine is cleaved by cystathionase to give cysteine and α- ketobutyrate (which will be changed to propionylCoA and then succinyl-CoA) • Homocysteine can be changed to methionine: N5-methyl THF donates CH3 to cobalamin to give methyl cobalamin; methyl cobalamin donates the CH3 to homocysteine and methionine will be formed 49 50 • Cysteine allostericaly inhibits cystathionase and represses the expression of the cystathionine -β-synthase gene • The deficiency of cystathionine -β-synthase or poor binding to its cofactor PLP would lead to increased amounts of methionine and homocysteine in the blood Homocysteine would then dimerize to homocystine that is excreted in the urine leading to homcystinuria excess homocysteine levels have been asssociated with mental retardation and atherosclerosis (homocysteine may damage the blood vessels and stimulate the proliferation of smooth muscle cells) • During the degradation of cysteine, the sulfur can be disposed of in two ways the production of sulfuric acid the formation of PAPS (activated sulfur) o The transamination of pyruvate yields alanine 51 Amino acids related to Krebs Cycle intermediates 1. α- ketoglutarate • Glutamate by transamination or glutamate dehydrogenase reaction • From glutamate glutamine is synthesized by amidation; glutamine synthetase is one of the only three enzymes of humans that can fix free ammonia to organic molecules – the other two enzymes are glutamate dehydrogenase and CPS I • An intermediate known as glutamate γ semialdehyde is synthesized from glutamate • Proline and ornithine (which is precursor to arginine) can be synthesized from or changed to glutamate and degraded through glutamate γ semialdehyde if arginine is consumed in protein synthesis, more ornithine would be synthesized from glutamate 52 53 54 • Although histidine is effectively recycled in humans, when degraded, five of its carbons give rise to glutamate Formiminoglutamate obtained from histidine is changed to glutamate by transferring the formimino group to THF 55 2. Oxaloacetate • Oxaloacetate is transaminated to aspartate and aspartate receives an amino group from glutamine and is changed to asparagine • Asparagine is broken down to aspartate and NH4+ by asparaginase and aspartate is transaminated back to oxaloacetate 3. Fumarate • the urea cycle and the purine nucleotide cycle change the 56 carbons of aspartate to fumarate • Fumarate can be obtained from the breakdown of tyrosine (meaning phenylalanine also can give fumarate) 4. Succinyl-CoA • Methionine, threonine, valine and isoleucine are degraded to propionyl-CoA that will be changed to succinyl-CoA methionine produces propionyl-CoA from αketobutyrate during the synthesis of cysteine Threonine dehydratase also gives off α-ketobutyrate • the main site of branched chain amino acid metabolism is the muscles • After transamination, the keto acids of all three amino acids (valine, isoleucine and leucine undergo oxidative decarboxylation; branched-chain α-keto acid dehydrogenase complex – an analog of the PDC complex 57 • The subsequent reactions from all three amino acids give the reduced equivalents NADH and FADH2 • Valine produces propionyl-CoA only • Isoleucine degradation gives acetyl-CoA in addition to propionyl-CoA • leucine produces acetyl-CoA and acetoacetate (purely ketogenic) • Defects in branched-chain α-keto acid dehydrogenase complex will lead to maple syrup urine disease; it can progress to mental retardation • Methylmalonyl CoA-mutase , an enzyme involved in the processing of propionyl-CoA to succinyl-CoA, can be deficient leading to methylmalonic acidemia (a rare but deadly disorder) 58 59 Amino acids that form acetyl-CoA and acetoacetate • Phenylalanine is hydroxylated to tyrosine by phenylalanine hydroxylase, a mixed function oxidase Tetrahydrobiopterin (BH4) is the cofactor used • Tyrosine is transaminated to p hydroxyphenylpyruvate • p hydroxyphenylpyruvate is decarboxylated to homogentisate by a dioxygenase • Homogentisate 1,2- dioxygenase converts homogentisate to maleylacetoacetate ; after two more steps, fumarate and acetoacetate are obtained • Phenylketonuria (PKU) results from the deficiency of phenylalanine hydroxylase in this case, a minor pathway of phenylalanine metabolism, transamination to give phenylpyruvate, becomes dominant phenylalanine and phenylpyuvate in the blood and urine Mental retardation ensues; exclude phenylanine from diet 60 61 Tyrosinemia III 62 • homgentisate accumulates when homogentisate 1,2dioxygenase is deficient: alcaptonuria Relatively benign; the urine turns black on standing Later in life, the accumulation of homogentisate on the joints may lead to arthritis Sir Archibald Garrod pioneered the study of inborn errors of metabolism based on his observations on alcaptonuria • Tyrosinemias I-III may result from the deficiencies of the other enzymes in tyrosine metabolism • Tryptophan produces alanine from the non-ring carbons and acetyl-CoA and formate from the ring structure • The ring could also be used in the synthesis of NAD+ and NADP+ - decreases the need for niacin in the diet • A minor pathway of threonine degradation in the liver can produce glycine and acetyl-CoA • Lysine degradation produces acetyl-CoA and acetoacetate63 64 65 The relation between THF, Vit B12 and SAM • N5-methyl THF is the most stable form of THF • The only reaction in which methyl is removed from THF is through transfer to vit B 12 during the synthesis of methionine • If vit B 12 is deficient, N5-methyl THF would accumulate and eventually most of the THF in the body would be found in the form of N5-methyl THF - “Methyl Trap” hypothesis reactions that utilize folate would be compromised • pernicious anemia has hematopoeitic and neurologic components • The hematopoeitic problems are thought to arise from a secondary deficiency of folate resulting from the primary deficiency in vit B 12 (absence of intrinsic factor) • The neurologic disorders are caused by the absence of the regenerating effect of vit B 12 on SAM; SAM is needed for methylation reactions in the nervous tissue and also, methylmalonyl-CoA competes with malonyl-CoA 66 67 Specialized products synthesized from amino acids o Most neurostransmitters are either amino acids or derivatives of amino acids Amino acids: glycine, glutamate, aspartate and γ aminobutyric acid (GABA) • GABA is the most important inhibitory neurotransmitter in the central nervous system • It is synthesized through the decarboxylation of glutamate • a characteristic feature of the production of biological amines is decarboxylation which requires PLP 68 • Histidine is decarboxylated to histamine Histamine is a mediator of allergic and other inflammatory reactions, stimulator of gastric acid production and an excitatory neurotransmitter in the brain • Dopamine (D), epinephrine (E) and norepinephrine (NE) are collectively known as catecholamines D and NE are excitatory neurotransmitters in the brain; E and NE are also secreted by the adrenal medulla and the peripheral nervous system the first step in the synthesis of catecholamines is the BH4 dependent hydroxylation of tyrosine to form 3,4-dihydroxyphehnylalanine (DOPA) DOPA is then decarboxylated to dopamine Dopamine undergoes vitamin C dependent hydroxylation to yield norepinephrine SAM methylates norepinephrine to epinephrine 69 70 • Parkinson’s disease is associated with low levels of dopamine in the brain L- Dopa is used for treatment in the late stages of the disease. Dopamine cannot cross the blood- brain barrier; once L-Dopa gets into the brain, it will be changed to dopamine • The decarboxylation of tyrosine may produce tyramine which binds to NE receptors and causes headaches and hypertension if present in high quantities cheese, beer, red wine,… contain high amounts of tyramine 71 • Tryptophan is converted to the neurotransmitters serotonin and melatonin in the pineal gland • Tetrahydrobiopterin-dependent hydroxylation and PLPdependent decarboxylation are involved • The conversion reactions are sensitive to light • Serotonin accumulates in the brain during the daytime and it is converted to N-acetylserotonin and then melatonin in the dark • Serotonin inhibits feeding and elevates the mood Prozac, an anti-depressant acts by inhibiting serotonin reuptake into the presynaptic neuron • Melatonin may be involved in male sexual maturation; it has roles in controlling the biological clock (cricadian rhythm) and serves as an anti-0xidant 72 73 • The catecholamines, tyramine and serotonin are inactivated by oxidative deamination catalyzed by monoamine oxidase (MAO) by methylation through the action of catechol – O – methyl transferase (COMT) • Histamine is first methylated by SAM and then acted upon by MAO followed by another oxidation step • GABA is inactivated by changing it back to glutamate and then α-ketoglutatrate • MAO produces H2O2 while degrading neurotransmitters • MAO inhibitors are used in the early stages of Parkinson’s disease and as antidepressants if people taking MAO inhibitors consume tryraminerich foods, the tyramine will not be degraded and this will lead to serious hypertension – the “cheese effect” 74 75 • Nitric oxide (NO) is produced from arginine • Nitric oxide synthase (NOS) catalyzes a five electron oxdiation of the guanidino nitrogen of arginine • Two successive monoxygenation reactions occur to generate the intermediate Nω–hydroxy-L-arginine • NOS has got five prosthetic groups: FMN, FAD, heme, BH4 , and Ca2+ - calmodulin • There are three tissue specific isozymes of NOS: neuronal (nNOS), endothelial (eNOS) and inducible (iNOS) • nNOS and eNOS activities are tightly regulated by Ca2+ • Ca2+ has no effect on iNOS, rather by cytokines; this is the isoform that is involved in the production of the NO that is produced by macrophages in order to kill microorganisms • The NO produced by nNOS and eNOS acts in low concentrations in the control of blood pressure, neurotransmission, learning and memory 76 • NO brings about vasodilation by activating guanylate cyclase which increases the cellular level of cGMP • Normally a phosphodiesterase terminates the action of NO by changing cGMP to GMP • Sildenafil (viagra) blocks a specific isozyme of phosphodiesterase and perpetuates the vasodilation 77 o Amino acids are also used in the synthesis of substances other than neurotransmitters • Arginine and glycine are involved in the synthesis of creatine • in the kidney, the guanidino group of arginine is transferred to glycine to give ornithine and guanidoacetate in the liver, SAM methylates guanidoacetate to creatine ATP then donates a phosphate group to creatine to give phosphocreatine Creatine phosphate is used as a donor of phosphate in the regeneration of ATP from ADP Phoshpocreatine or creatine can be non-enzymatically converted into the cyclic compound creatinine • the urinary creatinine excretion of a person is extremely constant from day to day and is proportional to the muscle mass. 95 % of the creatine in the body is found in the skeletal muscles and the remaining part in the heart, brain and testes 78 79 • Creatinine Clearance Test: compares the level of creatinine in urine (24 hrs.) with the creatinine level in the blood • it is used for assessing kidney function • Polyamines are positively charged molecules with multiple amino groups that are found in high concentrations in cells • The decarboxylation of ornithine produces putrescine • Putrescine then reacts with decarboxylated SAM (from methionine) and produces spermidine; spermidine is changed by the same process into spermine Increase in the number of amino groups • The decarboxylation of lysine and arginine would lead to cadaverine and agmatine , respectively • Polyamines may stabilize DNA by interacting with the negatively charged phosphate groups of nucleotides • They may also, to some extent, replace for cellular K+ and Mg2+ and control nucleic acid and protein synthesis 80 81 • Melanin is a family of polymeric pigments of different colors synthesized from tyrosine • tyrosinase catalyzes the conversion of tyrosine to DOPA and DOPA to dopaquinone • A number of intermediates follow from DOPA to finally produce polymerized melanin • Melanocytes produce melanin and carotene which blend and give rise to the color of the skin, hair and eyes • Melanin granules are uniformly distributed in melanocytes and offer protection by absorbing ultra violet rays • The deficiency of tyrosinase or other enzymes in the synthesis pathway of melanin leads to albinism lack of pigment in the skin, eyes and hair; sensitivity to sunlight 82 83 84