Musculoskeletal notes BETA
advertisement

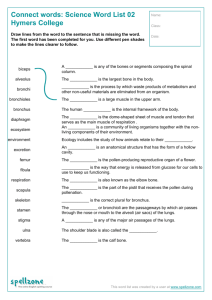
Giles Kisby GE Y1 Musculoskeletal Musculoskeletal: Spring Term: LECTURES: 07/03/14: Bone Development and Metabolism: Duncan Bassett Los (from booklet): Define bone structure. Explain the difference between intramembranous and endochondral ossification. Define the role of the osteoblast, osteoclasts and chondrocyte. Recall the bone remodeling cycle in adult bone. Define osteoporosis, list its common causes and outline treatment strategies that may be used. Define Paget’s disease and the bone pathology seen in this disorder. Los (from slides): 1. Contrasting endochondral and intramembranous ossification 2. Understand the role of chondrocyte, osteoblasts, osteoclasts and osteocytes 3. Describe the bone remodelling cycle 4. Contrast the affect of intermittent and continuous PTH on the skeleton 5. Define age related osteoporosis and list the common risk factors 6. Describe the causes of secondary osteoporosis 7. Describe DXA BMD analysis with particular reference to the T and Z scores 8. List the main medications used to treat osteoporosis and describe their action 9. Compare and contrast the uses of PTH and the bisphosphonates 10. Describe the skeletal consequences of long term glucocorticoid treatment 11. Describe the indications for treatment of Paget’s disease and the mechanism of action of the therapy Notes 1 Giles Kisby - GE Y1 Musculoskeletal Skeletal Physiology o Bone Structure Osteoid: is a protein mixture secreted by osteoblasts that forms the organic matrix of bone. Bone is formed when osteoid mineralizes There are two types of osseous tissue that form bones: Cortical bone = compact bone: Forms the cortex, or outer shell, of most bones Osteon: refers to the functional unit of most compact bone comprised of a central blood vessel [in a “Haversian canal”] and concentric rings of new bone encircling the vessel o Hydroxyapatite crystals [Ca10(PO4)6(OH)2] pack in between Type 1 collagen fibrils within and between each ring o Each ring is from successive remodelling cycles o Osteon structure limits fracture propagation o Collagen fibres orientated in all various directions within each ring o Type I collagen molecule: Triple helical collagen molecule 2x alpha 1 (COL1A1) and 1x alpha2 (COL1A2) o 200 non-collagenous proteins are also present in bone o Human bone is 60% mineralised: increased mineralisation increases stiffness but reduces flexibility o Cortical bone accounts for 80% of the total bone mass of an adult skeleton The microscopic difference between compact and cancellous bone is that compact bone consists of haversian sites and osteons, while cancellous bones do not. Also, bone surrounds blood in the compact bone, while blood surrounds bone in the cancellous bone Cancellous bone = trabecular bone = spongy bone: Filling the interior of the bone is the trabecular bone tissue (make the overall organ lighter and allow room for blood vessels and marro) Trabecular bone accounts for the remaining 20% of total bone mass but has nearly ten times the surface area of compact bone. Its porosity is 30–90% Compared to compact bone, cancellous bone has a higher surface area to mass ratio because it is less dense The primary anatomical and functional unit of cancellous bone is the trabecula. Cancellous bone is highly vascular and frequently contains red bone marrow where haematopoiesis, occurs. 2 Giles Kisby GE Y1 Musculoskeletal o Cancellous bone is typically found at the ends of long bones, proximal to joints and within the interior of vertebrae. Bone development: Long bones form by endochondral ossification Type II collagen is found in cartilage (tensile strength) Aggrecan (Aggrecan is the major proteoglycan in articular cartilage) is negative so draws in water for compressive strength CHONDROCYTES ARE THE ONLY CELLS FOUND IN HEALTHY CARTILAGE; undergo proliferation differentiation hypertrophy (chondrocytes can expand 10x just before they die; helps extend bone) death as they migrate out from center of the bone; this leaves a tunnel through which blood vessels can form; bone can then be laid down from these centers to form cortical bone from these centers (primary ossification center) o Sox9: Master transcriptional regulator in chondrocyte 3 Giles Kisby GE Y1 Musculoskeletal o FGF/FGFRs: Inhibit chondrocyte proliferation and differentiation o Indian hedgehog (Ihh): Promotes chondrocyte proliferation and induces PTHrP o PTHrP/PTHR1: Inhibit chondrocyte differentiation Secondary ossification center is at the epiphysis growth plate; the growth plate is supported by trabecular bone and will fuse with the ‘head’ bone only when growth is complete Achondroplasia: o Cause: Constitutively active FGF/FGFR3 signalling inhibits chondrocyte proliferation and differentiation Gain of function mutation FGFR3 o Most common form of dwarfism o Macrocephaly [head is abnormally large], frontal bossing, midface hypoplasia, small chest, rhizomelia [shortened limbs] Craniofacial bones by intramembranous ossification Fontanelles form Mesenchymal cells differentiate into osteoblasts Bone (osteoblasts) is formed directly without a cartilage scaffold o Osteoblasts, chondrocytes and adipocytes all derive from mesenchymal cells o Osteoblasts are formed from the mesenchymal cells in the context of Runx2, Osterix and high B-Catenin [other factors also have pos / neg roles: Wnt, BMPs and FGFs Systemic hormones: GH/IGF1, glucocorticoids, E2: Estradiol, PTH and 1,25(OH)2D] o Wnt signalling role: Promotes osteoblast differentiation, proliferation and mineralisation On absence of Wnt GSK3/APC/Axin degradation complex targets B-catenin for degradation by phosphorylation On presence of Wnt: Wnt binds Frizzled with coreceptors LRP5/6 and inhibits GSK3 Preventing B-catenin degradation B-catenin enters nucleus regulating target genes (but is not a TF itself) Negative regulation of Wnt signalling [ie these neg regulators are targets for new anabolic agents for treatment of osteoporosis]: 4 Giles Kisby GE Y1 Musculoskeletal Target Wnt: Wnt binding (WIF-1 , cereberus and sFRP) Target coreceptor: LRP5/6 degradation (Sclerostin (SOST gene in nature) and Dickkopf (Dkk)) Relavant info from endo: • PTH regulates calcium via PTHR1 in bone: • PTHR1 expressed in osteoblasts and osteocytes but NOT osteoclasts • PTH has anabolic and catabolic actions: • PTH can stimulate bone resorption or formation • Intermittent PTH (net trabecular formation) • Continuous PTH (net cortical resorption) • PTH increases osteoclast differentiation indirectly by action in osteoblasts • Increased expression of M-CSF/RANKL • Reduced expression of OPG 5 Giles Kisby GE Y1 Musculoskeletal • PTH regulates maturation of preosteoblasts • Intermittent PTH increases Runx2 • Continuous PTH represses Runx2 • PTH also increases bone formation by paracrine mechanisms: • Increased FGF release at osteocytes • Increased signalling for osteoblast lineage: Increased IGF-1 Increasing Wnt signalling Reduced inhibition of Wnt signalling: dec dickkopf and Sclerostin, the product of the SOST gene o Maintenance of adult bone Terminally differentiated osteoblasts act as Mechanosensors & regulators of bone remodeling The bone remodelling cycle: Functions: o Maintain homeostasis of Ca 2+ and PO4 o Repair damaged matrix and micro-fractures o Adapt to mechanical stress and strain Cells involved: o Osteocytes make up 90-95% of all adult bone cells o Osteoblasts 5% of all adult bone cells o Osteoclasts 1-2% of all adult bone cells Osteocytes regulate bone turnover o In response to bone loading state During bone loading osteocytes inhibit osteoclast resorption (via inc OPG and TGFB) Unloading, hypoxia or apoptosis initiates resorption (via inc RANKL) o In response to endocrine phosphate needs Low phosphate: Osteocyte Sclerostin binds LRP5 ( dec Wnt signaling and dec bone formation) Vs High phosphate: Osteocyte Matrix extracellular phosphoglycoprotein (MEPE) inhibits phosphate resorption Osteocyte Dmp1 and Phex decrease leading to inc FGF23 for increase to phosphate levels 6 Giles Kisby GE Y1 Musculoskeletal Osteoclasts o Development: Osteoclasts derive from the myeloid lineage; therefore: o Osteoclasts are multinucleated cells M-CSF regulates proliferation, survival and differentiation of precursors RANKL is key osteoclastogenic cytokine sufficient for differentiation OPG is a ‘decoy receptor’ (binds and blocks RANKL: ie physiological inhibitor of RANKL/RANK signaling) [RANK is on the osteoclast precursor] Denosumab acts like OPG therefore can be used as a drug to reduce bone resorption via dec osteoclast levels PTH, 1,25(OH)2D and pro-inflammatory cytokines increase RANKL expression and suppress OPG Function: Active osteoclasts are polarised cells: Attach to the bone surface via integrin α5β3 (this forms the sealing zone that degradatory components are secreted into; nb lacunae = an unfilled space; a gap, as created under site of osteoclast binding): Requires action of small GTPases (inhibited by bisphosphonates) Secrete hydrogen and chloride ions that dissolve bone mineral Matrix metalloproteinases (MMPs) and Cathepsin K degrade the collagen matrix: Cathepsin K inhibited by Cathepsin K inhibitors 7 Giles Kisby - GE Y1 Musculoskeletal Skeletal Pathology o Osteoporosis Traits: Increased bone resorption relative to formation Low bone mass Micro-architectural deterioration Fragility fractures Diagnosis of osteoporosis: Fragility fracture and decreased bone mineral density (BMD) Peak bone mass Achieved at 20 - 30 years of age major genetic component to peak bone mass Estrogens is critical in both male and females for peak bone mass Peak influenced by: Physical exercise, alcohol excess, smoking, eating disorders, systemic illness Increased progressive loss of bone mass occurs from 45 years of age; Mechanism: Estrogens deficiency at the menopause o More rapid loss in women due to estrogens deficiency at menopause o Increased expression of skeletal cytokines especially IL-6 inc [“pro-inflammatory cytokines”] o Reduced expression of OPG and thus increased osteoclastogenesis Investigation o Ca2+, Pi, ALP [high bone alkaline phosphatase in osteoporosis], Cre [looking for potential liver problem giving dec hydroxylase activity], PTH, 25-OH-vitD, DEXA, Urinary 8 Giles Kisby GE Y1 Musculoskeletal NTX [N-terminal telopeptide (NTx) molecules are mobilized from bone by osteoclasts and subsequently excreted in the urine] o DEXA = Dual-energy X-ray absorptiometry: assesses BMD (Bone mineral density) Results are interpreted according to the standard deviation from the mean to give T and Z score: a) Sex matched peak bone mass (T-score) [ie no. SD from those in 20s with a max BMD] b) Sex and age matched BMD (Z-score) [ie no. SD from those of same age as the person] WHO diagnostic criteria: Osteoporosis o T score ≤ - 2.5 lumbar spine, femoral neck or total hip Osteopenia o T score ≤ - 1.0 lumbar spine, femoral neck or total hip Treatment of age related osteoporosis o Simple advice: inc weight bearing exercise, dec smoking and alcohol o Optimise vitamin D status: Calcium and vitamin D supplementation o Antiresorptive agents: Bisphosphonates (impaired sealing zone attachment) Denosumab (monoclonal ab to RANKL) (OPG like activity) Selective estrogens receptor modulators (inc OPG, dec IL6) o Anabolic agents Strontium ranelate (now limited use due to cardiac risk) Teriparatide (PTH 1-34) (Intermittent PTH: intermittent use activates osteoblasts more than osteoclasts, which leads to an overall increase in bone) continuous PTH - decrease Runx2 Intermittent - increase runx2 9 Giles Kisby GE Y1 Musculoskeletal Secondary Osteoporosis Endocrine o Thyrotoxicosis (increased bone turnover) o Hyperprolactinemia (reduced gonadotrophins and sex hormones Eg E2!!) o Primary hyperparathyroidism (Increased resorption) o Hypogonadism (increased resorption due to low E2 etc) o Cushing’s Syndrome (impaired bone formation due to high cortisol) Nutritional [but not severe enough to give osteomalacia] o Vitamin D deficiency (impaired mineralisation) o Coeliac disease (impaired mineralisation) o Chronic liver disease [ie loss of liver vit d role] Iatrogenic o High dose glucocorticoids (Glucocorticoid induced osteoporosis) o GnRH agonists (eg for prostate cancer: after about ten days, a profound hypogonadal effect (i.e. decrease in FSH and LH) is achieved through receptor downregulation by internalization of receptors. Generally this induced and reversible hypogonadism is the therapeutic goal.) o Aromatase inhibitors (eg for Breast cancer) o Thyroid hormone excess (Excessive replacement or Thyroid cancer) o Anticoagulants and Anticonvulsants [mech is unknown] o Immunosuppression (inhibits calcineurin and NFAT to give dec IL2 so dec im response but calcineurin-NFAT signaling pathway helps to promote osteoblast differentiation) o Thiazolidinediones (PPARϒ agonists; as on prev diagram this is a inducer of the adipocyte lineage: dec osteoblastogenesis, inc adipogenesis) 10 Giles Kisby GE Y1 Musculoskeletal o Glucocorticoid induced osteoporosis in detail [Commonest iatrogenic cause of osteoporosis]: As prev, inhibits osteoblast differentiation and encourages osteoblast apoptosis: Also: Decreased osteoclastogenesis but prolonged survival Treatment o Bisphosphonates o Teriparatide Paget’s Disease Traits: Localised disorder of bone remodelling) Osteoclast abnormality: Increased osteoclast numbers Osteoblast abnormality: Disorganised rapid bone formation o Replacement by sclerotic bone o Bone marrow cavity replaced by vascular fibrous connective tissue o Increase in bone size and bone deformity Increased markers of formation and resorption o bALP: Bone alkaline phosphatase o P1NP: Procollagen type I N-terminal propeptide o uNTX: Urinary N-terminal telopeptide Aetiology Predominantly unknown Family history in 15% Declining in incidence: Reason for decline in frequency is unknown Clinical features Bone pain, joint pain, deformity, fracture 11 Giles Kisby GE Y1 Musculoskeletal increased temperature [high metabolic activity] Deafness (due to cranial nerve compression) Abnormal x-ray Complications Osteoarthritis due to deformity Cranial nerve palsy and spinal stenosis [abnormal narrowing (stenosis) of the spinal canal] Hypercalcaemia if are also immobilised (immobility is associated with hypercalcaemia in a variety of diseases, as here, but unknown mech Fracture Osteosarcoma (very rare) Diagnosis Raised alkaline phosphatase: ALP Abnormal x-ray (osteolysis, osteosclerosis and bone expansion) 99Tc bone scan: is far more sensitive than plain X-ray; is taken up in the areas of high turnover [Technetium-99m] Treatment: Bone pain is the indication for treatment Ensure patients are vitamin D and calcium replete Simple analgesia (NSAIDs) Physio/hydrotherapy Bisphosphonates: reduce pain, do not prevent deformity or deafness Zolendronic acid (Alk Phos normalises in 90%) Surgery for severe deformity or osteoarthritis 12 Giles Kisby GE Y1 Musculoskeletal 07/03/14: Connective tissue and articulations: Matthew Pickering Los (from slides/booklet): List the main components of the extracellular matrix Recall the principal type of collagen in bone and articular cartilage List the main collagen-cleaving enzymes (collagenases) Explain what is meant by synarthrosis, diarthrosis, amphiarthrosis Describe the structure of articular cartilage and synovium List the key features of the heritable collagen disorders: Osteogenesis imperfecta Marfan’s syndrome Ehlers-Danlos syndrome Notes - Extracellular matrix [ie are initially just looking generally at ECM during this lec] o ECM functions: Mechanical: tensile and compressive strength and elasticity Protection: buffering against extracellular change and retention of water Organisation: control of cell behaviour by binding of growth factors and interaction with cell-surface receptors o ECM contains: Proteins: Collagen Elastin Fibrillin Adhesin Proteoglycans: Are proteins bound to glycosaminoglycans (GAGs) o ECM contains: Proteins: Collagen o 20-30% of body mass: is the most abundant protein in the human body o Types I, II, III, V and XI are the most abundant o Bone = type I collagen o Cartilage = type II collagen 13 Giles Kisby GE Y1 Musculoskeletal o o o o o o o Triple helix: = tropocollagen 3 polypeptide chains twisted into right handed major helix Type 1 = 2x alpha 1 and 1x alpha2 Type 2 = 3x alpha 1 repeating triplet amino acid Glycine-X-Y 300nm long and 1.5nm wide During synthesis polypeptide chains are hydroxylated Enzymes: prolyl hydroxylase and lysine hydroxylase The enzymatic reactions need cofactors including VITAMIN C In vitamin C deficiency (scurvy) collagen becomes unstable Degradation: Collagenases binds to triple helical collagen, unwinds polypeptide chains and then cleaves -chains by peptide hydrolysis Certain Matrix metalloproteinases [eg 1/8/13/ gelatinases/stromelysins] are collagenases type 1 collagen 2x alpha 1, 1x alpha 2 bone, tendon, ligaments, skin, joint capsule/synovium, cornea/sclera [= type 5] type 2 collagen 3x alpha1 cartilage, intervertebral discs, vitreous humour [is the clear gel that fills the space between the lens and the retina of the eyeball] [= type 11] type 3 collagen blood vessels type 4 collagen basement membrane, lens capsule [ie is the basement membrane of the lens] 14 Giles Kisby GE Y1 Musculoskeletal Elastin o Present at ligaments, vessels and skin o Elastin is polymer of tropoelastin monomers [lysine residues in adjacent monomers cross link by forming desmosine] o Elastin = Fibres that can stretch when hydrated and return to original length after being stretched o Mutations in elastin gene cause autosomal dominant cutis laxa Cutis laxa is a group of disorders that share common finding of lax, redundant skin. skin does not recoil when stretched: ‘appears to have lost elasticity’ Fibrillin o o Present at ligaments, vessels and skin Is a glycoprotein that is essential for formation of elastic fibres: elastin must be deposited around a fibrillin core therefore loss gives similar phenotype to elastin deficiency o Fibrillin-1 mutations → Marfan’s syndrome o Fibrillin-2 mutations → Contractural arachnodactyly Adhesin o Is a group term: refers to cell-binding glycoproteins present in matrix and basement membranes o attach to cells via cell integrins o Include: Fibronectin in connective tissue Laminin in basement membrane Chondroadherin in cartilage Osteoadherin in bone 15 Giles Kisby GE Y1 Musculoskeletal Proteoglycans: Are glycoproteins containing one or more sulphated glycosaminoglycan (GAG) chains GAGs: are repeating polymers of disaccharides [N-acetyl glucosamine is usually one of the two repeating sugars; the chain is also usually sulfated]: [eg Heparan sulphate, Chondroitin sulphate, Keratan sulphate, Dermatan sulphate, Heparin] Proteoglycans may be: o Intra-cellular o Cell surface-associated o Secreted into ECM Intracellular proteogylcan - Serglycin Cell surface associated - betaglycan, syndecan Secreted into ECM - aggrecan, decorin, fibromodulin, lumican, biglycan Examples: o Aggrecan (in association with hyaluronan) is the major proteoglycan in articular cartilage Also: aggrecan molecules associate with central hyaluronic acid filament in cartilage o Hyalurinic acid (by itself) is the only non-sulphated GAG and is major component of synovial fluid where it has an important role in maintaining synovial fluid viscosity Synchondrosis, syndesmosis, secondary cart/symphysis, synovial - CLASSIFICATION OF JOINTS o Synarthrosis: suture lines of skulls where adjoining plates are separated by thin fibrous tissue o Amphiarthrosis: adjacent bones bound by flexible cartilage (‘fibro-cartilaginous joints’) e.g. pubic symphysis, sacro-iliac joints, intervertebral discs o Diarthrosis: synovial joints and include: Ball and socket e.g. hip joint Hinge e.g. inter-phalangeal joint Saddle e.g. first carpo-metacarpal joint Plane e.g. patello-femoral joint Synovium [=Synovial membrane] contains: macrophage-like phagocytic cells and fibroblast-like cells 16 Giles Kisby GE Y1 Musculoskeletal - ARTICULAR CARTILAGE o Components: Collagen II: 90% is type II: tensile strength Chondrocytes Proteoglycan monomers (aggrecan): compressive strength Is combo of chondroitin sulphate chains and keratan sulphate chains (ie on the protein) non-covalently linked aggrecan molecules associate with central hyaluronic acid filament Negatively charged chemical groups of GAGs attract water o Is an avascular and aneural structure o Weight-bearing properties of articular cartilage depend on intact collagen scaffold and high aggrecan content - OSTEOGENESIS IMPERFECTA o = ‘brittle bone disease’ o mostly due to autosomal dominant collagen type I mutations o variable phenotypic severity [Types I (good) – IV (bad) describe the severity] o Pathogenesis: Abnormal type I collagen results in bone fragility: osteopenia and fractures Diminished collagen in the sclera (of the eye) leads to increased translucency and apparent blueness of the sclera 17 Giles Kisby - GE Y1 Musculoskeletal EHLERS-DANLOS SYNDROMES Ehlers-danlos syndromes: o Majority are autosomal dominant disorders o Involve abnormalities in synthesis or enzymatic modification of collagen o [characterised by joint, tissue/skin laxity and arterial wall abnormality/estensibility] o Clinical features: Joint hypermobility Skin fragility (easy bruising) Hyper-extensibility in other organs e.g. Gorlin’s sign: hyperextensible tongue Arterial wall laxity → aneurysms o EDS type IV “= arterial form”: autosomal dominant defect in type III collagen found in blood vessels little skin and joint disease but arterial or bowel rupture o Not all are autosomal dominant disorders: EDS type VI (oculo-scoliotic) which is autosomal recessive in addition to skin and joint hyperextensibility, scoliosis and ocular globe rupture occur. 18 Giles Kisby - GE Y1 Musculoskeletal MARFAN’S SYNDROME o Autosomal dominant condition due to mutation in fibrillin-1 gene o characterised by ocular, skeletal, vascular, lung and skin abnormalities o Pathogenesis: Defect is due to fibrillin which forms constituent of extracellular microfibrils that form sub-structure for elastin Fibrillin important in elastic walls of arteries especially aorta, zonular fibres of the eye, ligaments, skin and lung parenchyma o Clinical features: Musculoskeletal tall stature, long thin extremities, arachnodactyly, dolichostenomelia (low ratio of upper to lower body segments) pectus excavatum [“hollowed chest”], scoliosis high arched palate Other ectopia lentis i.e. upward dislocation of the lens ascending aorta dissection (most common cause of death) mitral valve prolapse, aortic regurgitation cystic lung disease and spontaneous pneumothorax o “Patients are often unusually tall, their aorta is prone to rupture/displacement and they can have abnormalities of the skeleton and joints and lens. The product of the affected gene is unable to play its normal role in stabilising the elastic fibres that give connective tissue its strength and flexibility.” 19 Giles Kisby - GE Y1 Musculoskeletal OTHER SYNDROMES o Stickler syndrome type II collagen Autosomal dominant, ocular and joint disease o Alport’s syndrome type IV collagen o autosomal recessive Hereditary glomerulonephritis and deafness “This inherited kidney disease is characterised by dysfunctional glomerular filtering. The defective protein product of the affected gene cannot form its normal sheet-like structure in the basal lamina where it normally provides tensile strength. “ Dystrophic Epidermolysis bullosa type VII collagen Hereditary skin blisters Dominant or recessive forms 20 Giles Kisby GE Y1 Musculoskeletal - Junctional Epidermolysis Bullosa o “Characterised by extensive mucocutaeous blistering and recurrent infections. The protein product of the affected gene normally forms heterotrimeric molecules that are crucial in forming the 2-dimensional structure of the basal lamina.” o Laminin 5 or Type XVII collagen - Congenital Muscular Dystrophy o Heterogenous group of neuromuscular disorders characterised by muscle weakness and hypotonia. About half of these patients have mutations in a gene encoding of a key component of the basal lamina of skeletal muscle. o Laminin 2 21 Giles Kisby GE Y1 Musculoskeletal 07/03/14: ARTICULAR PATHOLOGY: Matthew Pickering Los (from slides/booklet): - Define what is meant by matrix metalloproteinase and give some examples of their substrates - Define what is meant by ADAMTS protease and understand that aggrecanases are important in the turnover of proteoglycan in articular cartilage - Recall that cathepsin K is important protease in bone matrix turnover - Define two abnormalities seen in the synovium of patients with rheumatoid arthritis - Explain the importance of the inflammatory cytokine, tumour necrosis factor-alpha (TNF-α) in rheumatoid arthritis pathology - Define two abnormalities seen in the cartilage and two abnormalities seen in the bone in the osteoarthritic joint From slides supplementary: - Summarise the pathogenesis, clinical features and management of rheumatoid arthritis - Explain the significance of a ‘rheumatoid factor’ - Explain the importance of anti-CCP antibodies in rheumatoid arthritis Notes - Overview o In brief: Connective tissue turnover is mediated by matrix proteinases through complex regulatory networks Rheumatoid arthritis and osteoarthritis represent the two major articular pathologies Rheumatoid is a disease of synovium whilst osteoarthritis is disease of articular cartilage o Connective tissue turnover and matrix proteinases Most of joint tissue is extra-cellular matrix and proteinases are key in extracellular matrix (ECM) degradation Proteases are numerous and combine to form complex regulatory networks o Articular pathology Rheumatoid arthritis Osteoarthritis - Connective tissue turnover o Cartilage and bone destruction is mediated by ECM degradation o Modulated by level of: Proteases MMP collagenases vs cartilage collagens ADAMTS aggrecanases vs cartilage proteoglycans Cathepsin K vs bone matrix [is in the acidic secretions of osteoclasts] 22 Giles Kisby GE Y1 Musculoskeletal o o o o Protease inhibitors Matrix synthesis Source of proteinases depends on pathological process: Osteoarthritis = chondrocyte (intrinsic) Rheumatoid arthritis = synovial cells (intrinsic), inflammatory cells (extrinsic), chondrocytes Infection = inflammatory cells (extrinsic), bacterial proteases (exogenous) MATRIX METALLOPROTEINASES Family of calcium-dependent zinc-containing endopeptidases Important functions include tissue remodelling and degradation of extracellular matrix (ECM) ECM substrates include: [all the main ECM components:] Collagen and gelatin (=hydrolysed collagen) Elastin Proteoglycans and Matrix glycoproteins Regulated by hormones, growth factors and cytokines Synthesised in zymogen form by many cell types Inhibited by ‘tissue inhibitors of matrix metalloproteinases’ (TIMPs) Certain MMPs are COLLAGENASES: MMP-1, -8, -13 (= collagenase -1, -2, -3): cleave fibrillar collagen at a single site to form fragments stromelysins and gelatinases degrade the collagen fragments [these are also MMPs] ADAMTS METALLOPROTEINASES ADAMTS = a disintegrin and metalloproteinase with thrombospondin motifs Are a family with diverse functions but note ADAMTS-4 and 5 are aggrecanases i.e. degrade aggrecan, the major human cartilage proteoglycan CATHEPSIN K Important in turnover of matrix of long bone Active against helical type I collagen Cysteine protease most active at acidic pH; are highly expressed by osteoclasts; secretions of the osteoclast is acidic; Cathepsin K-deficient osteoclasts cannot degrade bone protein matrix Human deficiency results in skeletal dysplasia (Pycnodysostosis) 23 Giles Kisby - GE Y1 Musculoskeletal Articular pathology o Rheumatoid arthritis Chronic autoimmune disease characterised by pain, stiffness and symmetrical synovitis (inflammation of the synovial membrane) of synovial (diarthrodial) joints PATHOGENESIS There is an excess of pro-inflammatory vs. anti-inflammatory cytokines (‘cytokine imbalance’); immune cells recruited Neovascularization occurs The synovium becomes a proliferated mass of tissue (pannus) Treatment: Anti TNFα antibodies: TNFα is the dominant pro-inflammatory cytokine so mAbs against this are used o But use is linked to inc TB infection risk Interleukin-6 and interleukin-1 blockade: now available in clinic Anti-B cell antibodies: We can deplete B cells in rheumatoid arthritis by parenteral (intravenous) administration of an antibody against a B cell surface antigen (are vs CD20) o But use linked to hepatitis B reactivation DENOSUMAB: monoclonal antibody against RANKL. RANKL (“receptor activator of nfKB ligand”) is important in bone destruction in rheumatoid arthritis: o Produced by T cells and synovial fibroblasts in rheumatoid arthritis o Acts to stimulate osteoclast formation (osteoclastogenesis) o Upregulated by: IL-1, TNF-a IL-17, PTH-rp o Binds to RANK on osteoclast precursors; action antagonized by OPG too ‘DMARDS’: disease- modifying anti-rheumatic drugs o may induce remission (not cure) and prevent joint damage o eg methotrexate, sulphasalazine [and its metabolite 5-ASA nb given that ulcerative colitis produces arthritic symptoms, the benefits may be a product of unrecognized ulcerative colitis] o all have significant adverse effects Glucocorticoid therapy (‘steroids’, ‘prednisolone’) but: o preference is to avoid long-term use because of side-effects o useful as short-term treatment options e.g. to control flare of disease or inflammation of single joint Key features: Chronic arthritis o Polyarthritis - swelling of the small joints of the hand and wrists is common o Symmetrical 24 Giles Kisby GE Y1 Musculoskeletal o o Early morning stiffness in and around joints May lead to joint damage and destruction - ‘joint erosions’ on radiographs o Swan-neck deformity [PIP hypext; DIP hypflex] o Boutonnière (‘button-like’) deformity [PIP hypflex] Extra-articular disease can occur o Fever, weight loss [due to the immune complexes] o Subcutaneous rheumatoid nodules [are associated with Rheumatoid factor] central area of fibrinoid necrosis [fibrin-rich necrotic material middle layer of macrophages and fibroblasts Outer layer of connective tissue o Others rare e.g. vasculitis, episcleritis, Amyloidosis Rheumatoid ‘factor’ may be detected in blood o = IgM autoantibody against Fc portion of IgG [misnomer: should really be called rheumatoid ‘antibody’ not ‘factor’] Will deposit elsewhere Antibodies to citrullinated protein antigens (ACPA) o Antibodies to citrullinated peptides are highly specific for rheumatoid arthritis and also associated with smoking = Anti-cyclic citrullinated peptide antibody ‘anti-CCP antibody’ [=ACPA] o Citrullination of peptides is mediated by enzymes termed Peptidyl arginine deiminases (PADs): perform Arg Citrulline citrullinated peptides present in high concentrations in neutrophils and monocytes Primary site of pathology is in the synovium [the synovium becomes a proliferated mass of tissue (pannus)]; synovium includes: o Tenosynovium surrounding tendons o Bursas o Synovial joints Wrists Knees Ankles Metacarpophalangeal joints (MCP) 25 Giles Kisby GE Y1 Musculoskeletal Proximal interphalangeal joints (PIP) Metatarsophalangeal joints (MTP) Important genetic component Specific HLA-DRβ gene variants mapping to amino acids 70-74 of the T cell DRβ-chains are strongly associated with rheumatoid arthritis = the ‘shared epitope’ nb in the ‘shared epitope’ hypothesis: a common region of the beta chain on the T cells is thought to be integral to presenting autoimmunological peptides. Important environmental component Smoking: contributes 25% of population-attributable risk and interacts with ‘shared epitope’ to increase risk Radiographic abnormalities Early o Juxta-articular osteopenia Later o Joint erosions at margins of the joint Later still o Joint deformity and destruction 26 Giles Kisby - GE Y1 Musculoskeletal Osteoarthritis o Chronic slowly progressive disorder due to failure of articular cartilage that typically affects joints of the hand (especially DIP, PIP), spine and weight-bearing hips and knees o Caused by: (see pic) Excessive loading on joints Abnormal cartilage o o Cartilage changes in osteoarthritis reduced proteoglycan reduced collagen chondrocyte changes e.g. apoptosis Bone changes in osteoarthritis Proliferation of superficial osteoblasts results in production of sclerotic bone [pathologic thickening of the bone] e.g. subchondral sclerosis 27 Giles Kisby GE Y1 Musculoskeletal o Focal superficial necrosis resulting from focal stress on sclerotic bone New bone formation at the joint margins (termed osteophytes) Osteophytes at the PIPJ are called Bouchard's nodes Osteophytes a the DIPJ are called Heberden's nodes Schlerosis, cysts, osteophytes, narrowing 28 Giles Kisby GE Y1 Musculoskeletal 14/03/14: Energy pathways in muscle and the Metabolic Myopthies: (Federico Roncaroli) Los (from slides/booklet): - - - - Recognise the bioenergetics of muscle contraction Summarise the role of creatine phosphate, creatine kinase and myokinase as a short term energy source Summarise the role of anaerobic glycolysis i.e. the break-down of glucose to lactate and pyruvate and conversion of ADP to ATP (mainly type II fibres that have few mitochondria and many glycogen granules) as an intermediate-term energy source Summarise the role of oxidative phosphorylation i.e. aerobic process that generates ATP from fat, carbohydrate and protein (type I fibres are suited to this as thay have many mitochondria and lipid droplets) as a long term energy source Distinguish the different types of metabolic myopathy Summarise the key types of primary metabolic myopathies i.e. (1) glycogen storage disorders, (2) lipid disorders and (3) mitochondrial disorders (NB detailed knowledge of individual syndromes is not required) Summarise the common glycogen storage disorders: Myophosphorylase deficiency (also termed: McArdle’s syndrome, glycogen storage disorder type V) (NB detailed knowledge of individual syndromes is not required) Notes [lec was v. poor] - - - Primary muscle disease o Genetic o Non genetic Secondary muscle disease: muscle involvement in a systemic condition o Autoimmune o Cancer o Infection ESSENTIAL CONCEPTS o Energy pathways are aimed to reconstitute ATP from ADP ATP is the immediate source of energy: binds myosin and allows sarcomeric contraction and release of actin o Acetyl-CoA is the essential molecule of all pathways o Muscle fibres need energy for contraction o Slow and fast twitch fibres have different metabolic requirements [ie low but long term requirements vs high but short term requirements] 29 Giles Kisby GE Y1 Musculoskeletal Slow fibres use/have: (run marathons) low glycogen high lipids [They are the major source of energy for muscle after long exercise when glycogen is exhausted; Their hydrolysis produces Acetyl-CoA] more mitochondria oxidative phosphorylation: o aerobic process that generates ATP from fat, carbohydrate and protein o long term energy source Fast fibres use/have: (run 100m) High glycogen level [Synthesised from glucose by Glycogen synthase] Few mitochondria anaerobic glycolysis, o the break-down of glucose to lactate and pyruvate o intermediate-term energy source - Creatine kinase reaction [ ], Adenylate kinase reaction [ADP ⇔ ATP + AMP] o Nb Adenylate kinase = myokinase; don’t confuse with Myophosphorylase From wiki; not from the course: [note that the twitch category reflects the properties of the diff myosin isoforms: one key difference between slow and fast twitch fibres is the ability of myosin ATPase, to speed up 30 Giles Kisby GE Y1 Musculoskeletal the cross bridge action. There is a small structural difference between FT and ST myosin ATPase, which is enough to cause a difference in cross bridging recycling rates] - METABOLIC MYOPATHIES o Usually infantile and adult forms – Infants are usually more severely affected o They usually present with muscle dysfunction induced by exercise rhabdomyolysis may become mildly symptomatic during childhood and emerge late in life o heterogenous group of disorders characterised by anomalies of energy production: a huge array of the enzymes of the diverse pathways may be the root cause of the myopathy - Types of myopathy: o Congenital o Dystrophies [degeneration due to disease or malnutrition] o Metabolic / mitochondrial o Inflammatory o Neurogenic - Key types of primary metabolic myopathies: [(NB detailed knowledge of individual syndromes is not required)] o (1) glycogen storage disorders, Myophosphorylase deficiency = McArdle’s syndrome Is a glycogen storage disorder type V Myophosphorylase is the muscle isoform of the enzyme glycogen phosphorylase: o Cytosolic enzyme o Removes glucose residues from α-(1,4)-linkages within glycogen molecules o Product of reaction: Glucose-1-phosphate. (NOT Glucose) CLINICAL FEATURES o Exclusively myopathic o Presents with cramps and myoglobinuria following exercise o No respiratory impairment (unlike other myopathies) Autosomal recessive PYGM gene mutation on ch11[“phosphorylase, glycogen, muscle”] 80 known types of mutation: No protein expression or unstable protein (ie wholly dysfunctional) 31 Giles Kisby GE Y1 Musculoskeletal o o Acid maltase deficiency = Pompe’s disease = alpha-glucosidase deficiency Is a glycogen storage disorder type II Defect of acid 1-4 alpha glucosidase [GAA gene; “glucosidase, alpha; acid”] o Lysosomal enzyme o Hydrolyses linear α1-4 glucosidic linkages on carbohydrates o Catalytic site: Asp-518 Clinical features o Children: Muscle weakness and respiratory impairment; especially severe in infants Common cardiac involvement o Widespread accumulation of glycogen (eg positive in white blood cells) [excessive accumulation of glycogen within lysosome-derived vacuoles in nearly all types of cells. Excessive quantities of free extralysosomal glycogen also have been described] o Increase in acid phosphatase activity at lysosomes o Focal expression of MHC class I antigen (misdiagnosed as possible myositis) o The enzyme may retain some functionality; exact symptoms depend of type of mutation Subtle changes in adults Is classed as an autosomal recessive mutation to acid alpha-glucosidase GAA gene (2) lipid disorders Result from defects of: transport or endogenous triglycerides catabolism or beta-oxidation Various clinical presentation: progressive myopathy with muscle weakness or recurrent episodes of rhabdomyolysis causing intolerance to exercise PATHOLOGICAL FEATURES Accumulation of lipid droplets Fibre necrosis in some patients presenting with rhabdomyolysis e.g. carnitine deficiency syndrome (3) mitochondrial disorders Presumably oxidative phos is defective etc Eg Impairment of respiratory chain eznymes 32 Giles Kisby - GE Y1 Musculoskeletal Diagnosis techniques: o Examination [weakness, wasting (gait, winging, ptosis), pain] o Biopsy [BUT: if good may still be a myopathy, if bad may still be in normal range] o MRI o Genetic analyses o Blood tests o EMG [electromyography], NCV [nerve conduction veloicity] (these are for analysing nerve problems eg MG diagnosis) o Blood: CK (not raised in all myopathies; only if muscle cell membranes are damaged), lactate, inflam markers - Neuropathy results in distal weaknes of muscle e.g. gripping - Muscle problem results in proximal weakness- e.g. shoulders, problems standing 33 Giles Kisby GE Y1 Musculoskeletal 14/03/14: Molecular basis of muscle contraction (Valentina Caorsi) Los (from slides/booklet): Recall the actin-myosin cross-bridging cycle. Recall the organisation of individual myocyte and motor unit. Explain the processes involved in depolarisation and intracellular calcium flux. Distinguish the structure of the thin and thick filaments in muscle. Notes - The contractile Unit: the Sarcomere o Many in parallel per cell o When end to end will form a myofibril; myofibrils continuous between myocytes positioned end to end o A band = all myosin o I band = actin ONLY o actin is the major component of thin filaments troponin and tropomyosin etc will also contribute to the light filaments actin filaments made by polymerisation of G-actin Thin filament length: 1.1 µm: Ie shorter than thick filaments Length regulated by nebulin and tropomodulin o myosin forms the thick filaments are single molecules but the tails of many diff myosins can interlink as in muscle myosin molecules are composed of a head, neck (= essential light chain + regulatory light chain), and tail domain Titin is a large elastic and extensible protein that links the thick filaments to the Z-line, thus ensuring that the thick filaments remain centred in the sarcomere. Thick filaments length: 1.6µm Ie longer than thin filaments 34 Giles Kisby GE Y1 Musculoskeletal 35 Giles Kisby GE Y1 Musculoskeletal - Cross-bridges Cycle detail: o See below: o thin filament moves toward the centre of the sarcomere o Step size is small: sliding produced by one cycle is only about 1% of the sarcomere length - Motor Unit o Is the Motor Neuron + all the muscle fibres it innervates o 1 motor unit has muscle fibres of all the same type [ie slow vs fast; is because type is determined by signalling from the nerve]] Ie fast vs slow etc is not just determined by glycogen reserves etc but also determined by the isoforms of myosin present; these will all be of the same type within a motor unit o Muscles of a motor unit will contract simultaneously (all or none fashion) o number of muscle fibres 1 motor unit innervates can vary smaller motor units present in the eye for sensitive movements o Number of motor units that are in a muscle can vary More present at sensitive muscles eg eye muscles o When a muscle grows only the number of actins and mosins etc within individual sarcomeres/myofibrils increases; the number of sarcomeres/myofibrils stays the same as does the number of motor units 36 Giles Kisby - - GE Y1 Musculoskeletal Latent period: - Intention to move Movement: o Intention to move o Activity in cerebral cortex basal ganglia, cerebellum o Motor cortex firing o Impulses in descending motor pathways o Motoneuron Excitation o Impulse propagation to axon terminal o Neuromuscular transmission o Impulse propagation along muscle fiber plasmalemma o Impulse into T-tubules o voltage-gated DHPRs mechanically linked to RyR of SR inducing Ca2+ release o Troponin binds Ca2+; tropomyosin moves out myosin binding sites on actin o Cross-bridges engagement o Movement Contraction: o Cross bridge cycle occurring o Isotonic No change in tension: tension in the muscle remains constant; Muscle is changing in length Concentric tension rises to meet the resistance, then remains the same as the muscle shortens Eccentric muscle lengthens due to the resistance being greater than the force the muscle is producing o Isometric Tension rises then remains constant but no shortening occurs o How force is varied in vivo Frequency of action potentials Recruitments of motor units 37 Giles Kisby GE Y1 Musculoskeletal Filament overlap Velocity of contraction Frequency of action potentials: o Temporal Summation occurs if a second stimulus is applied before completion of relaxation Additional influx of Ca2+ promotes a second contraction which is added to the first Stronger overall force results o Tetanus is rapid multiple stimulations which will fuse into a smooth continuous total contraction Abundant intracellular calcium provides continually available binding sites on actin for cross-bridge cycling The maximum force achievable will result from the tetanus due to maximal Ca2+ release Fatigue will eventually occur as ATP is exhausted /Ca escapes through PM Recruitments of motor units: o o o Greater percent of motor neurone pool recruited with an increasing force requirement Henneman's size principle states that in order to move a load motor units are recruited from smallest to largest This also equates to slow FFR FF 38 Giles Kisby GE Y1 Musculoskeletal Filament overlap: o o o Maximum force is achieved at intermediate overlap When overlap is too great the filaments become constrained / not enough space in the sarcomere for the filaments to move into upon further movement When overlap is too little there are too few heads engaged to achieve maximum force Aside: at heart the pericardial sac will prevent overextension therefore the force is just seen to increase with length / preload Velocity of contraction: o o The greater the velocity in the flexion direction the weaker the force will be The greater the velocity in the opposite direction to the flexion direction the stronger the force will be until a maximum is reached (muscle acting as brake); [is because more crossbridges can be attached as are not needing to reel in the weight] 39 Giles Kisby GE Y1 Musculoskeletal - “hence bodybuilders do exercises beyond their strength where are acting as brake” Relaxation: o Once the membrane has repolarised, the calcium channels in the sarcoplasmic reticulum close. o The sarcoplasmic Ca-ATPase [SERCA] pumps calcium back into the reticulum, causing a decrease in calcium concentration in the cytoplasm. o This causes calcium dissociation from troponin, resulting in inactivation of myosin binding sites on actin, and hence muscle relaxation. 40 Giles Kisby GE Y1 Musculoskeletal 14/03/14: Molecular basis and features of the muscular dystrophies: (Matthew Pickering) Los (from slides/booklet): Define muscular dystrophy. Explain how muscular dystrophies may be inherited. Give one example of X-linked, autosomal recessive and autosomal dominant muscular dystrophy. Explain how these conditions manifest clinically (NB detailed knowledge of individual syndromes is not required). Explain the histological differences between myopathy and dystrophy. Explain the significance of an elevated blood level of creatine kinase (also termed creatine phosphokinase and referred to commonly by physicians as ‘CK’ or ‘CPK’). Notes - Disorder of neurons = neuropathy : typically distal dysfunction (hands / feet) Disorders of skeletal muscle = myopathy : typically proximal dysfunction (shoulders / hips): o GENETIC Muscular dystrophies [the focus of this lec] o Dystrophies (or muscular dystrophies) are a subgroup of myopathies characterized by muscle degeneration and regeneration. Clinically, muscular dystrophies are typically progressive, because the muscles' ability to regenerate is eventually lost, leading to progressive weakness e.g. Duchenne muscular dystrophy eg Beckers muscular dystrophy eg Limb-girdle dystrophy Metabolic myopathies defects of glycogen metabolism: e.g. myophosphorylase deficiency defects in lipid metabolism: e.g. carnitine deficiency syndrome Mitochondrial myopathies o complex multisystem disorders o myopathy is common Congenital myopathies a cause of ‘floppy infant’ ACQUIRED Autoimmune inflammatory myopathies polymyositis dermatomyositis Toxin / drug induced alcohol steroid myopathy (glucocorticoids) Endocrine: Cushing’s syndrome 41 Giles Kisby GE Y1 Musculoskeletal Thyroid disease Acquired metabolic myopathy K, Mg, Ca, P abnormalities due to diet etc vitamin D deficiency uraemia, hepatic failure - Creatine phosphokinase o Abundant in heart, skeletal muscle and brain and raised in blood when: Skeletal muscle pathology All types of muscular dystrophies (nb usually normal in neurogenic muscle disease) Rhabdomyolysis [lysis of skeletal muscle cells] o Alcohol o Crush injury o Drugs Muscle injury o trauma, o surgery, o intra-muscular injections Autoimmune inflammatory muscle diseases o Dermatomyositis o Polymyositis Myocardial infarction Some cases of brain injury e.g. stroke o CRE: = creatinine blood test measures the level of creatinine in the blood. Creatinine is a waste product that forms when creatine breaks down; creatine, creatinine and CPK will all be raise in muscle injury as above - Muscular dystrophies: o = Inherited group of disorders characterized by muscle wasting and weakness o Genetic heterogeneity o Clinical heterogeneity e.g. childhood vs. adult onset e.g. cardiac vs respiratory involvement o X-linked dystrophies Duchenne muscular dystrophy X linked recessive = 2/3; sporadic = 1/3 most common muscular dystrophy; considered a mainly proximal muscle weakness problem mutations in the dystrophin gene on Xp21(locus 21 on X) 42 Giles Kisby GE Y1 Musculoskeletal o mutations result in severe reduction or absence of dystrophin in skeletal and cardiac muscle o many diff mutations possible; typically are out of frame o one third have no family history i.e. de novo mutations relatively high o Dystrophin is an intracellular protein linking intracellular actin of sarcomeres with the ECM; dystrophin loss gives loss of protection against contraction induced damage to the cell (so muscular dystrophy results) o Absence of dystrophin results in muscle fibre damage, abnormal intra-cellular calcium entry, cell death dystrophin isoforms are expressed in brain (therefore deficiency results in mental retardation in ~30%) Clinical features o Young onset: symptoms typically occur before age of 6 years o progressive muscle weakness: initially legs and pelvis (Gower’s sign: difficulty rising from the floor) abnormal gait wheelchair bound by teenage years o spinal scoliosis o muscle contractures [muscle and its tendons shorten, resulting in reduced flexibility] in the legs due to fibrosis of damaged muscle fibres 43 Giles Kisby GE Y1 Musculoskeletal o o o respiratory insufficiency due to respiratory muscle weakness feeding difficulties in late stages mortality in late teenage years / early twenties [eg due to cardiomyopathy] o mental retardation in ~30% Diagnosis o Examination Clinical signs as above o Creatine phosphokinase (CPK) massive elevation (since birth) 10-100x normal range o Molecular genetic testing screen for commonest mutations in 90% genotype-phenotype correlation can be deduced o Muscle biopsy In a dystrophy Muscle fibre degeneration and regeneration Fibres of all sizes randomly arranged in muscle fascicle Accumulation of fibrous tissue and fat within the muscle In a atrophy changes are due to motor neurone damage; this only affects fibres belonging to the motor units whose axon has been damaged (ie observe healthy muscle next to wasted motor units) 44 Giles Kisby GE Y1 Musculoskeletal Management o Corticosteroids o Management of complications; examples: Spinal fusion for scoliosis Non-invasive ventilation Feeding aids, gastrotomy ACE inhibitors for cardiomyopathy o Experimental gene therapy approaches Beckers muscular dystrophy X linked recessive Less common and less severe than Duchenne muscular dystrophy o ‘patient walking in their teens’ Many due to ‘in-frame’ dystrophin gene mutations so less dysfunction o partial expression of truncated but functional protein o Heterogeneity of presentation due to the exact nature of the mutation As with other dystrophies: Hypertrophic proximal weakness (ie the hypertrophy is the fibrosis / lipid deposition) Cardiomyopathy common (two thirds of cases) o Malignant hyperthermia on exposure to muscle relaxants (e.g. suxamethonium) and halogenated inhaled anaesthetics (e.g. isoflurane) o Ie due to the overstimulation causing excessive ATP use and thus heat generated Autosomal dystrophies Limb-girdle muscular dystrophy Ie name indicates is a proximal dystrophy has dominant and recessive forms o Autosomal dominant (LGMD1) form o Autosomal recessive (LGMD2) form Complex group of disorders as diverse clinical features o Nomenclature based on the deficient protein is commonly used: E.g. laminin → ‘laminopathy’, Eg. dysferlin → ‘dysferlinopathy’ Muscle biopsy key investigation o Dystrophic changes o Absence of specific muscle protein Raised CPK 45 Giles Kisby GE Y1 Musculoskeletal 21/03/14: Musculoskeletal examination and synovial fluid analysis: Matthew Pickering Los (from booklet): Define and perform the GALS (Gait, Arms, Legs, Spine) examination Define the following commonly used rheumatological terms: arthritis, arthralgia, subluxation, synovitis Distinguish the pattern of joint disease in Rheumatoid arthritis, Osteoarthritis and Reactive Arthritis Summarise the importance of arthrocentesis and its general contraindications and potential complications Summarise the clinical features of gout Describe the crystals seen within the synovial fluid in gout Recognise the role of synovial fluid examination in septic arthritis Notes Nb Crepitus = grating, crackling or popping sounds and sensations experienced under the skin and joints - Definitions: o Arthritis - refers to definite inflammation of a joint(s) i.e. swelling, tenderness and warmth of affected joints o Arthralgia - refers to pain within a joint(s) without demonstrable inflammation by physical examination o Dislocation - articulating surfaces are displaced and no longer in contact o Subluxation - Partial dislocation o Valgus deformity - lower limb deformity whereby whereby distal part is directed away from the midline e.g. hallux valgus o Varus deformity - lower limb deformity whereby whereby distal part is directed towards the midline e.g. varus knee with medial compartment osteoarthritis 46 Giles Kisby GE Y1 Musculoskeletal NOTE: - ‘sero-negative spondyloarthropathies’: [each are expanded upon later]: DHTK: (NB detailed knowledge of these conditions is not required): Seronegative spondyloarthropathy (or seronegative spondyloarthritis) is a group of diseases involving the axial skeleton and having a negative serostatus. "Seronegative" refers to the fact that these diseases are negative for rheumatoid factor o Ankylosing spondylitis a chronic inflammatory disease of the axial skeleton with variable involvement of peripheral joints and nonarticular structures. AS is a form of spondyloarthritis, a chronic, inflammatory arthritis spinal fusion; enthesopathy; HLA-B27 o Reiter’s syndrome = reactive arthritis develops in response to an infection in another part of the body lower limb asymmetric oligoarthritis with axial involvement o Arthritis associated with psoriasis (psoriatic arthritis) psoriasis = chronic relapsing/remitting immune-mediated skin disease characterized by red, scaly patches, papules, and plaques, which usually itch o Arthritis associated with gastrointestinal inflammation (enteropathic synovitis) - GALS EXAMINATION: o Gait o Arms o Legs o Spine - GALS EXAMINATION: 47 Giles Kisby GE Y1 Musculoskeletal o o o o Gait Arms Legs Spine smoothness and symmetry of leg, pelvis and arm movements normal stride length ability to turn quickly Look for normal girdle muscle bulk and symmetry Look to see if there is full extension at the elbows Are shoulder joints normal? Examine hands palms down with fingers straight Observe supination, pronation, grip and finger movements Test for synovitis at the metacarpo-phalangeal joints (MCP joints) Look for knee or foot deformity Assess flexion of hip and knee Look for knee swellings Test for synovitis at the metatarso-phalangeal joints (MTP joints) Inspect soles of the feet Is paraspinal and shoulder girdle muscle bulk symmetrical? Is the spine straight? Are the iliac crests level? Is the gluteal muscle bulk normal? Are there popliteal swellings? Are the Achilles tendons normal? Are there signs of fibromyalgia? Are spinal curvatures normal? Is lumbar spine and hip flexion normal? Is cervical spine normal? Then, after the GALS screen should perform a detailed examination of any abnormal joint(s) identified in the GALS screen: - The fundamentals aspects of locomotion to examine are: o the nature of the joint abnormality o the extent (distribution) of the joint involvement o Any other features of diagnostic importance - The fundamentals aspects of locomotion to examine are: o the nature of the joint abnormality Is there inflammation? Swelling Warmth 48 Giles Kisby GE Y1 Musculoskeletal Erythema Loss of function Tenderness Is there irreversible joint damage? Joint deformity Crepitus Loss of joint range or abnormal movement Is there a mechanical defect? May due to inflammation, degenerative arthritis or trauma identified by: o painful restriction of motion in absence of features of inflammation o instability Examples: Swelling is present in: GOUT o Acute gout is a good example of arthritis o Tissue deposition of monosodium urate (MSU) crystals occurs to give: Gouty arthritis Tophi (aggregated deposits of MSU in tissue) eg ear o Commonly affects the metatarsophalangeal joint of the big toe (‘1st MTP joint’) Gout is known as podagra when it involves the big toe o Abrupt onset o Extremely painful o Joint red, warm, swollen and tender Swelling is present in: ENTHESOPATHY: o = pathology at the enthesis i.e. the site where ligament or tendon inserts into bone o examples include: 49 Giles Kisby GE Y1 Musculoskeletal plantar fasciitis Achilles tendinitis ANKYLOSING SPONDYLITIS REACTIVE ARTHRITIS Joint deformity may occur in: ANKYLOSING SPONDYLITIS o It is a chronic inflammatory disease affecting: Sacroiliac joints and spine: May lead to spinal fusion and deformity Entheses resulting in chronic enthesopathy Non-axial joints – usually hips and shoulders o Strong association with HLA-B27 o Rheumatoid factor is negative: It is part of a group of conditions termed ‘sero-negative spondyloarthropathies 50 Giles Kisby GE Y1 Musculoskeletal o the extent (distribution) of the joint involvement determine number of joints involved: polyarthritis > 4 joints involved oligoarthritis 2-4 joints involved monoarthritis single affected joint note if involvement is symmetrical note the size of the involved joints is there axial involvement? Examples: rheumatoid arthritis o bilateral o symmetrical o involvement of large and small joints reactive arthritis o lower limb (predominantly) asymmetrical oligoarthritis o axial involvement gout o inflammation of the first metatarsophalangeal joints [*****************] 51 Giles Kisby GE Y1 Musculoskeletal o Any other features of diagnostic importance Examples: RHEUMATOID ARTHRITIS o SUBCUTANEOUS NODULES GOUT o TOPHI – subcutaneous deposits of uric acid Systemic lupus erythematosus o MALAR RASH 52 Giles Kisby - GE Y1 Musculoskeletal SYNOVIAL FLUID ANALYSIS o Used to test for Infection crystal arthritis [different crystals] Gout o Needle shaped birefringence negative o Monosodium Urate Pseudogout o Brick shaped birefringence positive o o o Calcium pyrophosphate dihydrate (CPPD) crystals normally: Colourless or pale yellow transparent viscous film covering synovium and cartilage with few cells Synthesized by synovial lining cells of synovium Two types of synovial lining cells: “type A” = macrophage-like “type B” = fibroblast-like: secrete the hyaluronic acid which results in the increased viscosity of synovial fluid [Synovial fluid is viscous fluid rich in hyaluronic acid] synovium collagen is Type I collagen 53 Giles Kisby GE Y1 Musculoskeletal o Abnormal increase in synovial fluid volume is termed ‘synovial effusion’ osteoarthritis due to abnormal mechanical stimulation with damage to cartilage and bone synovitis, gout, rheumatoid arthritis due to inflammation septic arthritis due to infection ie bacteria in joint due to injury, impaired defence etc 54 Giles Kisby GE Y1 Musculoskeletal 21/03/14: Rheumatoid arthritis, Osteoarthritis and Reactive arthritis: (Matthew Pickering) Los (from booklet): Define the term ‘reactive arthritis’ and summarise how it may present. Recognise that ‘reactive arthritis’ is part of a family of inflammatory arthritic syndromes termed ‘seronegative spondyloarthroapthies’ (NB detailed knowledge of these conditions is not required). Summarise the pathogenesis, clinical features and management of rheumatoid arthritis. Explain the importance of anti-CCP antibodies in rheumatoid arthritis. Notes - REACTIVE ARTHRITIS o 20 – 40 YRS o URETHRITIS o sterile inflammation in joints Reactive arthritis is distinct from infection in joints (septic arthritis) o occurs following/after infection especially urogenital (e.g. Chlamydia trachomatis) and gastrointestinal (e.g. Salmonella, Shigella, Campylobacter infections) infections Symptoms follow 1-4 weeks after infection and this infection may be mild o Reactive arthritis may be first manifestation of HIV or hepatitis C infection o Important extra-articular manifestations include: Enthesopathy Skin inflammation Eye inflammation o Associated with HLA-B27 o M>F [“males more likely to have HIV”] o musculoskeletal symptoms of reactive arthritis ARTHRITIS – ie joints Asymmetrical Oligoarthritis (<5 joints) Lower limbs typically affected: large joints ENTHESITIS – ie tendons Heel pain (Achilles tendonitis) Swollen fingers (dactylitis) Painful feet (metatarsalgia due to plantar fasciitis) SPONDYLITIS – ie spine Sacroiliitis (inflammation of the sacro-iliac joints) Spondylitis (inflammation of the spine) o Treatment: Non steroidal: NSAIDs Steroidal: intra-articular corticosteroid therapy 55 Giles Kisby - GE Y1 Musculoskeletal o Rheumatoid arthritis vs. Reactive arthritis: o Septic arthritis vs. Reactive arthritis OSTEOARTHRITIS o Chronic slowly progressive disorder o Cartilage changes reduced proteoglycan reduced collagen chondrocyte apoptosis o failure of articular cartilage that typically affecting joints of the hand (especially those involved in pinch grip), spine and weight-bearing joints (hips and knees) Joints of the hand Distal interphalangeal joints (DIP) o Osteophytes at the DIP joints are termed Heberden’s nodes Proximal interphalangeal joints (PIP) o Osteophytes at the PIP joints are termed Bouchard’s nodes First carpometacarpal joint (CMC) 56 Giles Kisby GE Y1 Musculoskeletal o o Spine Weight-bearing joints of lower limbs knees and hips First metatarsophalangeal joint (MTP) Caused by: Excessive loading on joints Abnormal joint components Radiographic features Joint space narrowing Subchondral bony sclerosis Proliferation of superficial osteoblasts Osteophytes new bone formation at the joint margins Subchondral cysts focal superficial necrosis Radiographic changes in Rheumatoid Arthritis vs. Osteoarthritis: [Osteopenia refers to bone density that is lower than normal] 57 Giles Kisby GE Y1 Musculoskeletal o - Management physiotherapy Weight loss Exercise Analgesia Joint replacement The following Los are covered in the ‘ARTICULAR PATHOLOGY LECTURE’: o Summarise the pathogenesis, clinical features and management of rheumatoid arthritis. o Explain the significance of a ‘rheumatoid factor’. o Explain the importance of anti-CCP antibodies in rheumatoid arthritis. 21/03/14: The Connective Tissue Disorders: (Matthew Pickering) Los (from booklet): Summarise the pathogenesis and clinical features of systemic lupus erythematosus (SLE). Recognise the importance of autoantibody measurement in the assessment of connective tissue disease and list the important antibodies associated with (1) systemic lupus erythematosus (SLE), (2) scleroderma, (3) Sjogren’s syndrome and (4) polymyositis. List the key features of: (NB detailed knowledge of these conditions is not required) Sjogren’s syndrome, scleroderma polymyositis Explain what is meant by the term ‘overlap syndrome’ in the setting of connective tissue disease. 58 Giles Kisby GE Y1 Musculoskeletal Notes Nb Arthralgia and arthritis is typically non-erosive (though not in RA) - Key conditions o Systemic Lupus Erythematosus (SLE) o Sjögren’s syndrome o Autoimmune inflammatory muscle disease Polymyositis Dermatomyositis o Systemic sclerosis (= scleroderma) o Overlap syndromes - Raynaud’s phenomenon o Raynaud’s phenomenon is most commonly isolated and benign condition but can be associated with some of the above conditions (cf for further info) o Painful o Is Intermittent vasospasm of digits on exposure to cold o Typical colour changes – white blue red: Vasospasm leads to blanching of digit Cyanosis as static venous blood deoxygenates Reactive hyperaemia then occurs (transient increase in organ blood flow that occurs following a brief period of ischaemia) 59 Giles Kisby - GE Y1 Musculoskeletal SYSTEMIC LUPUS ERYTHEMATOSUS o Prototypic autoimmune disease: B cell hyper-reactivity making autoantibodies o o o Associated with HLA-DR3 [same as the secondary HLA cause of coeliac (behind HLADQ2)] Clinical manifestations: Malar rash – erythema that spares the nasolabial fold Photosensitive rash Mouth ulcers Hair loss Raynaud’s phenomenon (see above) Arthralgia and sometimes arthritis Serositis (vs serous tissues: pericarditis, pleuritis, less commonly peritonitis) Renal disease – glomerulonephritis (‘lupus nephritis’) Cerebral disease – ‘cerebral lupus’ e.g. psychosis Laboratory manifestations: Haematological: Haemolytic anaemia Lymphopenia Thrombocytopenia [relative decrease of platelets in blood] Immunological Antinuclear antibodies o Likely accessed by antibodies by translocation of nuclear antigens to membrane surface in apoptosis and then impaired clearance of apoptotic cells o Eg Anti-Ro Anti-La Anti-Sm Anti-RNP Anti-Scl-70 Anti-ds-DNA antibodies o Also some non nuclear!: Anti-tRNA synthetase antibodies Anti-double-stranded DNA antibodies o Correlate with disease activity Complement consumption o Low C4 and C3 due to the Abs activating complement Sick lupus patient commonly has Low complement levels & High serum levels of anti-ds-DNA antibodies 60 Giles Kisby - GE Y1 Musculoskeletal SJÖGREN’S SYNDROME: sjögren’s syndrome o F>M o Autoimmune exocrinopathy lymphocytic infiltration of especially exocrine glands and sometimes of other organs (extra-glandular involvement) Exocrine gland pathology results in: Dry eyes (xerophthalmia) Dry mouth (xerostomia) Parotid gland enlargement o Commonest extra-glandular manifestations are: non-erosive arthritis Raynaud’s phenomenon o Termed ‘secondary’ Sjögren’s syndrome if occurs in context of another connective tissue disorder e.g. SLE o Associated with autoantibodies: Antinuclear antibody Anti-Ro (ie as does SLE) Anti-La (ie as does SLE) Rheumatoid factor 61 Giles Kisby - GE Y1 Musculoskeletal INFLAMMATORY MUSCLE DISEASE o Proximal muscle weakness due to autoimmune-mediated inflammation o o o o o Either with (=“ dermatomyositis”) or without (=“polymyositis”) a rash Skin changes in dermatomyositis: Lilac-coloured (heliotrope) rash on eyelids, malar region and naso-labial folds [nb these folds are spared in SLE] Red or purple flat or raised lesions on knuckles (Gottron’s papules) Subcutaneous calcinosis (ie calcium deposits) Mechanic’s hands (fissuring and cracking of skin over finger pads) Associated with autoantibodies: Antinuclear antibody (ie as does SLE) Anti-tRNA synthetase antibodies (ie as does SLE) Elevated CPK, abnormal electromyograpghy, abnormal muscle biopsy (polymyositis = CD8 T cells; dermatomyositis = CD4 T cells in addition to B cells) Associated with malignancy (10-15%) and pulmonary fibrosis 62 Giles Kisby - GE Y1 Musculoskeletal SYSTEMIC SCLEROSIS = scleroderma o Raynaud’s phenomenon o Thickened skin: fibrotic skin Signs: Dermal fibrosis cutaneous calcinosis telangiectasia [small dilated blood vessels near the surface of the skin or mucous membranes] o Skin changes may be limited or diffuse Diffuse systemic sclerosis Fibrotic skin everywhere including proximal to elbows or knees (excluding face and neck) Anti-topoisomerase-1 (=anti DNA gyrase = anti-Scl-70) antibodies Pulmonary fibrosis, renal (thrombotic microangiopathy) involvement Short history of Raynaud’s phenomenon Limited systemic sclerosis Fibrotic skin hands, forearms, feet, neck and face Anti-centromere antibodies Pulmonary hypertension Long history of Raynaud’s phenomenon 63 Giles Kisby GE Y1 Musculoskeletal - OVERLAP SYNDROME o When features of more than 1 connective tissue disorder are present e.g. SLE and inflammatory muscle disease we can use the term “overlap syndrome” o When incomplete features of a connective tissue disease are present we can use the term “undifferentiated connective tissue disease” o overlap syndromes include “mixed connective tissue disease” (‘MCTD’): - Mixed Connective Tissue Disease means Anti-U1-RNP antibody present (ie also in SLE [TRUE]) o Associated with features of seen in SLE, scleroderma, rheumatoid arthritis, and polymyositis Nb no autoantibodies for: - Osteoarthritis Gout Reactive arthritis Ankylosing Spondylitis psoriatic arthritis enteropathic synovitis 64 Giles Kisby GE Y1 Musculoskeletal Revision lecture put up by lecturer (can also use slides direct to test self): - List the key features of rheumatoid arthritis o Morning stiffness in and around joints o Symmetrical polyarthritis typically involving the small joints of the hand and/or wrists o Subcutaneous nodules o Rheumatoid factor o Joint erosions on radiographs - Define rheumatoid factor o Antibodies that recognize the Fc portion of IgG as their target antigen o typically IgM antibodies i.e. IgM anti-IgG antibody ! - What substance makes synovial fluid viscous? o Hyaluronic acid: a non-sulphated glycosaminoglycan - Define Reactive Arthritis o Sterile inflammatory synovitis following an infection whose extra-articular manifestations may include: Enthesopathy Skin inflammation Eye inflammation 65 Giles Kisby GE Y1 Musculoskeletal - List two infections associated with Reactive Arthritis o Urogenital infections E.g. Chlamydia trachomatis o Enterogenic infections E.g. Salmonella, Shigella, Campylobacter infections o Reactive arthritis may be first manifestation of HIV or hepatitis C infection - Define and give two examples of an enthesopathy o Inflammation where a ligament, tendon, fascia or capsule insert into bone. Examples include: Achilles tendonitis (painful heel) inflammation at insertion of Achilles tendon into calcaneum Plantar fasciitis (painful feet) inflammation at insertion of plantar fascia Dactylitis (swollen digits) inflammation at insertion of capsule and ligaments in digits Spondylitis (spinal inflammation) in Ankylosing Spondylitis inflammation where the outer part (annulus fibrosis) of the intervertebral disc inserts into the vertebral body 66 Giles Kisby GE Y1 Musculoskeletal [see above for ans] - In a single statement summarise the key pathological finding in osteoarthritis o Irreversible loss of articular cartilage - Define (i) proteoglycan and (ii) glycosaminoglycan and give one example of each o glycoproteins containing sulphated glycosaminoglycan chains e.g. Aggrecan o [GAGs: are repeating polymers of disaccharides] repeating polymers of disaccharides e.g. Hyaluronic acid (= hyaluronate) disaccharides are: glucuronic acid and N-acetyl glucosamine UNSULFATED!! Keratan sulphate disaccharides are: galactose and N-acetyl glucosamine Chondroitin sulphate disaccharides are: glucuronic acid and N-acetyl galactosamine - What is the major (i) collagen and (ii) proteoglycan found in articular cartilage? o Type II collagen o Aggrecan 67 Giles Kisby - GE Y1 Musculoskeletal List the major HLA association for each of the following diseases o Ankylosing Spondylitis & Reactive Arthritis HLA-B27 “there be average of 2 words in ‘Ankylosing Spondylitis’ and ‘Reactive Arthritis’ and 7 syllables (Ankylosing spondylitis = 8, Reactive Arthritis = 6, average = 7) so HLA-B27” o SLE HLA-DR3 “SLE has 3 letters so HLA-DR3” o Rheumatoid arthritis HLA-DR4 “U will remember that U is fourth letter in rheumatoid so HLA-DR4” 68 Giles Kisby GE Y1 Musculoskeletal 69