Introduction
advertisement

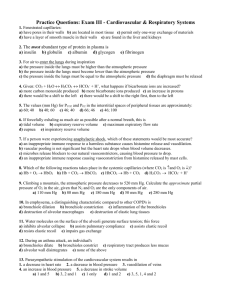
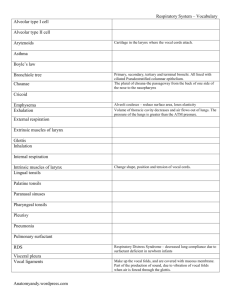
The Respiratory System • Cells continually use O2 & release CO2 • Respiratory system designed for gas exchange • Cardiovascular system transports gases in blood • Failure of either system – rapid cell death from O2 starvation Nose -- Internal Structures Pseudostratified ciliated columnar with goblet cells lines nasal cavity -warms air due to high vascularity -mucous moistens air & traps dust -cilia move mucous towards pharynx •entrance – external nares • two nasal cavities with bony outgrowths = nasal conchae (superior, middle, inferior) • nasal cavities separated by nasal septum and nasal bone •superior most region of the cavity – site for olfactory epithelium - olfactory receptors for odors (smell) • lacrimal glands drain into nasal cavities • nasal cavities communicate with cranial sinuses (air-filled chambers within the skull) • nasal cavities empty into the nasopharynx upper portion of the pharynx •connection between nasal cavity and nasopharnyx – internal nares •functions: warm, moisten, and filter incoming air Eustacian tube With tubal tonsil The Pharynx Nasopharynx • From internal nares to soft palate – Anatomical Landmark: openings of auditory (Eustachian) tubes from middle ear cavity – adenoids or pharyngeal tonsil in roof • Oropharynx Laryngopharynx • • • Extends from epiglottis to cricoid cartilage Anatomical Landmark: the epiglottis Common passageway for food & air & ends as esophagus inferiorly Passageway for air only • From soft palate to epiglottis – Anatomical Landmark: behind the uvula – palatine tonsils found in side walls, lingual tonsil in tongue • Common passageway for food & air Tortora & Grabowski 9/e 2000 JWS 23-5 The Larynx • triangular box = “voicebox” • top of the larynx is a hole = glottis • covered with the epiglottis • contains the vocal cords - mucosal folds supported by elastic ligaments •Epiglottis---leaf-shaped piece of elastic cartilage • filters, moistens, vocal production –during swallowing, larynx moves upward bringing the glottis up to the epiglottis –epiglottis bends slightly to cover glottis • Laryngeal cartilages: • 1. thyroid cartilage (Adam’s apple) • 2. cricoid cartilage • 3. arytenoid cartilage – for the attachment of true vocal cords and arytenoideus muscles Tortora & Grabowski 9/e 2000 JWS 23-6 Vocal Cords • False vocal cords (ventricular folds) found above the true vocal cords • True vocal cords attach to arytenoid cartilages • True vocal cord contains both skeletal muscle and an elastic ligament (vocal ligament) • When intrinsic muscles of the larynx contract they move the artytenoid cartilages & stretch the true vocal cords tighter • When air is pushed past the tightened vocal ligament, sound is produced Larnyx and Vocal Cords • true vocal cords vibrate upon passage of air > speech • thickness determines frequency of vibration and timber of sound thicker the cords – slower they vibrate – lower the pitch thinner the cords – faster they vibrate – higher the pitch • thickness also controlled by testosterone • pitch can also be controlled by tightening the vocal cords voluntarily -arytenoideus muscle and the intrinsic muscles of the true vocal cords can alter the “tightness” of the cords tighter the cords – faster they will vibrate 23-8 Tortora & Grabowski 9/e 2000 JWS 23-9 Trachea • • • • flexible cylindrical tube - Size is 5 in long & 1 in diameter sits anterior (in front of) the esophagus splits into right and left primary bronchi – enter the lungs held open by “C” rings of hyaline cartilage = tracheal cartilage –16 to 20 incomplete rings •open side facing esophagus contains smooth muscle = tracheal ligament • layers: – innermost layer (mucosa) = pseudostratified columnar with cilia & goblet cells –outer layer (submucosa) = loose connective tissue & mucous glands •functions: conducts air into the lungs, filtration, moistens mucosa submucosa Trachea and Bronchial Tree • • • • • Primary bronchi supply each lung Secondary bronchi supply each lobe of the lungs (3 right + 2 left) Tertiary bronchi splits into successive sets of Intralobular bronchioles that supply each bronchopulmonary segment ( right = 10, left = 8) IL bronchioles split into Terminal bronchioles -> these split into Respiratory Bronchioles each RB splits into multiple Alveolar ducts which end in an Alveolar sac Gross Anatomy of Lungs • Base, apex (cupula), costal surface, cardiac notch • Oblique & horizontal fissure in right lung results in 3 lobes • Oblique fissure only in left lung produces 2 lobes • Blood vessels & airways enter lungs at hilus • Forms root of lungs • Covered with pleura (parietal becomes visceral) Alveoli • Respiratory bronchioles branch into multiple Alveolar ducts • Alveolar ducts end in a grape-like cluster = alveolar sac or lobule -each grape = alveolus Respiratory membrane = 1/2 micron thick Alveoli • site of gas exchange by simple diffusion • from heart (right ventricle)-> Pulmonary artery multiple branches ending as the Pulmonary arteriole Capillary bed over Alveolus Pulmonary venule multiple veins Pulmonary vein heart (left atrium) • deoxygenated blood flows over the alveolus & picks up O2 via diffusion because the alveolar wall is very thin Cells Types of the Alveoli • Type I alveolar cells – simple squamous cells where gas exchange occurs • Type II alveolar cells (septal cells) – free surface has microvilli – secrete alveolar fluid containing surfactant O2 CO2 • Alveolar dust cells – wandering macrophages remove debris • Respiratory membrane = 1/2 micron thick Bronchioles • surrounded by “ring” of bronchiolar smooth muscle that can control the diameter of the bronchiole smooth muscle 23-16 Pleural Membranes & Pleural Cavity • Visceral pleura covers lungs • Parietal pleura lines ribcage & covers upper surface of diaphragm • Pleural cavity is space between the two pleura – contains a small amount of fluid Mechanism of Breathing: Boyle’s Law • As the size of closed container decreases, pressure inside is increased • As the size of a closed container increases, pressure decreases Mechanism of Breathing Inspiration: -at rest: pressure inside lung = pressure outside lungs (atmospheric pressure) -inhale - diaphragm contracts and drops, external intercostal muscles swing the ribcage up and out -increase in thoracic cavity volume results -due to the cohesiveness of intrapleural fluid – lung volume increases also -pressure inside the lung drops = Boyle’s Law -air rushes in to equalize -SO: muscles of inspiration do not act directly on the lungs but act to change the volume of the thoracic and pleural cavities Mechanism of Breathing Expiration: occurs because of the elasticity of the lungs - PASSIVE -in addition: relaxation of diaphragm and intercostal muscles returns thoracic and pleural cavity volume to normal -pressure of air in the lungs increases over atmospheric pressure -air leaves lungs to equalize 23-20 Summary of Breathing • Alveolar pressure decreases & air rushes in • Alveolar pressure increases & air rushes out Labored Breathing • Forced expiration – abdominal mm force diaphragm up – internal intercostals depress ribs • Forced inspiration – sternocleidomastoid, scalenes & pectoralis minor lift chest upwards as you gasp for air Respiratory Volumes and Capacities • tidal volume (TV) = amnt of air that enters or exits the lungs 500 ml per inhalation • inspiratory reserve volume (IRV) = max. amnt of air taken in after a normal inhalation, 3000 ml • expiratory reserve volume (ERV) = amnt of air forcefully exhaled, 1100 ml •residual volume (RV) = amnt of air left in lungs after forced expiration 1200 ml 23-23 Body tissue O2 and CO2 transport • most O2 is carried in the blood bound to hemoglobin of the RBC • some is dissolved in blood plasma ( O2 not very soluble in water) • CO2 is carried by the blood in 3 ways: 1. 90% of the CO2 enters the RBC - combines with water of the cytosol to form carbonic acid • • immediately dissociates into bicarbonate and H+ ions (binds to Hb) catalyzed by the RBC enzyme called carbonic anhydrase 2. some CO2 dissolves in the water of the plasma as carbonic acid H+ and bicarbonate 3. CO2 can combine directly with hemoglobin to form carbaminohemoglobin • in the lungs – Hb releases its H+ ion – it combines with the HCO3- to reform carbonic acid • carbonic acid breaks up into H2O and CO2 • CO2 is also released by Hb • CO2 diffuses into the alveolar air and is breathed out CO2 produced CO2 transport from tissues Interstitial CO2 fluid Plasma within capillary CO2 H2O Red blood cell Capillary wall CO2 H2CO3 Hb Carbonic acid HCO3 Bicarbonate HCO3 H+ To lungs CO2 transport to lungs HCO3 HCO3 H2CO3 Hemoglobin (Hb) picks up CO2 and H+. H+ Hb Hemoglobin releases CO2 and H+. H2O CO2 CO2 CO2 CO2 Alveolar space in lung Respiration Rate: controlled by a respiratory center made up of a Medullary rhythmicity area in the medulla and two nuclei in the pons -MRA -group of neurons with an automatic, rhythmic discharge -groups are called the dorsal and ventral respiratory groups -controls rate and depth of breathing -dorsal group is called the inspiratory center which send signals via the motor neurons of the phrenic nerve and intercostal nerves that supply the inspiratory muscles (diaphragm and external intercostals) -ventral group contains expiratory neurons – inactive during normal quiet breathing but called into play with active breathing Respiratory Center • Respiration also controlled by neurons in pons • Pneumotaxic Area – constant inhibitory impulses to inspiratory area • inhibits inspiration before lungs become too expanded • Apneustic Area – stimulatory signals to inspiratory area to prolong inspiration Respiratory Center • Chemical regulation • Central chemoreceptors in medulla – respond to changes in H+ or pCO2 • Peripheral chemoreceptors – respond to changes in H+ , pO2 or pCO2 – aortic body---in wall of aorta • nerves join vagus – carotid bodies--in walls of common carotid arteries • nerves join glossopharyngeal nerve • Cortical Influences Tortora & Grabowski 9/e 2000 JWS – voluntarily alter breathing patterns – limitations are buildup of CO2 & H+ in blood – inspiratory center is stimulated by 23-27 increase in either Negative Feedback Regulation of Breathing • Negative feedback control of breathing • Increase in arterial pCO2 • Stimulates receptors • Inspiratory center • Muscles of respiration contract more frequently & forcefully • pCO2 Decreases