Powerpoint 22 Respiration
advertisement
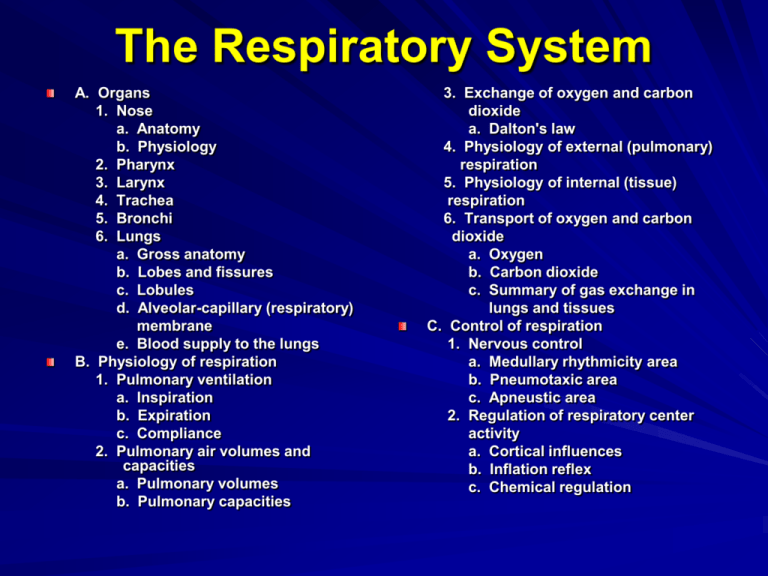
The Respiratory System A. Organs 1. Nose a. Anatomy b. Physiology 2. Pharynx 3. Larynx 4. Trachea 5. Bronchi 6. Lungs a. Gross anatomy b. Lobes and fissures c. Lobules d. Alveolar-capillary (respiratory) membrane e. Blood supply to the lungs B. Physiology of respiration 1. Pulmonary ventilation a. Inspiration b. Expiration c. Compliance 2. Pulmonary air volumes and capacities a. Pulmonary volumes b. Pulmonary capacities 3. Exchange of oxygen and carbon dioxide a. Dalton's law 4. Physiology of external (pulmonary) respiration 5. Physiology of internal (tissue) respiration 6. Transport of oxygen and carbon dioxide a. Oxygen b. Carbon dioxide c. Summary of gas exchange in lungs and tissues C. Control of respiration 1. Nervous control a. Medullary rhythmicity area b. Pneumotaxic area c. Apneustic area 2. Regulation of respiratory center activity a. Cortical influences b. Inflation reflex c. Chemical regulation Overview of Respiratory System The respiratory system has the following functions: 1. gas exchange 2. contains receptors for the sense of smell 3. filters, warms, and moistens inspired air 4. produces sounds 5. helps eliminate wastes other than carbon dioxide Respiration is the exchange of gases between the atmosphere, the blood, and the body cells. There are three basic processes involved: 1. pulmonary ventilation 2. external respiration 3. internal respiration Respiratory Organs 1. upper vs lower 2. conducting vs respiratory Nose Anatomy 1. external nose 2. internal nose 3. nasal cavity a. mucosa b. nasal septum c. vestibule d. nasal conchae (turbinate bones) Nose Physiology 1. filter, moisten, and warm air 2. olfaction 3. resonating chamber Pharynx 1. 2. 3. 4. muscular tube location constrictor muscles divisions a. nasopharynx b. oropharynx c. laryngopharynx Larynx 1. nine cartilages 2. thyroid cartilage 3. epiglottis 4. cricoid cartilage 5. laryngospasm 6. mucosa 7. vestibular folds 8. vocal folds 9. glottis 10. voice production Larynx and Voice Production Trachea 1. 2. 3. 4. 5. location mucosa submucosa cartilage adventitia Bronchial Tree 1. primary bronchi 2. secondary (lobar) bronchi ( 3 right, 2 left) 3. tertiary (segmental) bronchi (10 right, 8 left) 4. bronchioles 5. terminal bronchioles 6. respiratory bronchioles 7. alveolar ducts and sacs 8. alveoli Bronchial Tree Con’t 1. 2. 3. 4. 5. 6. 7. 8. primary bronchi secondary (lobar) bronchi tertiary (segmental) bronchi bronchioles terminal bronchioles respiratory bronchioles alveolar ducts and sacs alveoli Bronchial Tree (anatomical changes) 1. cartilage Trachea – C-shaped cartilage Bronchi – irregular plates of cartilage Bronchioles – cartilage gone 2. smooth muscle increases as cartilage decreases bronchodilation vs. bronchoconstriction 3. epithelium ciliated pseudostratified + goblet cells (trachea) ciliated simple columnar + goblet cells ciliated simple cuboidal + goblet cells ciliated simple cuboidal simple cuboidal simple squamous (alveoli) alveolus Smooth muscle Simple cuboidal Lumen of bronchiole Lungs 1. location 2. pleurae a. parietal b. visceral 3. pleural cavity (potential space) 4. pleural fluid Pleura Lungs, con’t 5. apex vs base 6. hilus 7. rt. lung = 3 lobes, 2 fissures (horizontal and oblique) 8. lt. lung = 2 lobes, 1 fissure (oblique) Lungs, con’t 9. bronchopulmonary segments 10. lobules 11. alveolus (3 cell types) a. squamous epithelial cell b. macrophage (dust cell) c. septal cell -- surfactant Alveolar-capillary membrane (respiratory membrane) 1. 2. 3. 4. surfactant alveolar epithelial cell fused basement membrane capillary endothelial cell Blood supply to the lungs 1. pulmonary artery 2. bronchial artery 3. pulmonary veins Physiology of Respiration What is the purpose of respiration? What three processes are necessary to accomplish this task: 1. pulmonary ventilation 2. external respiration 3. internal respiration Pulmonary Ventilation (breathing) 1. 2. 3. 4. inspiration vs expiration atmospheric pressure intrapulmonic pressure pressure gradient Thoracic Cavity Dimensions Inspiration (Active) 1. 2. 3. 4. Boyle's law inspiratory muscles phrenic nerve (C3-5) process thoracic volume pleural volume intrapleural pr. lung volume intrapulmonic pr. air flows into lungs Decrease volume increase pressure Increase volume decrease pressure Inspiration (Active) 1. 2. 3. 4. Boyle's law inspiratory muscles phrenic nerve (C3-5) process thoracic volume pleural volume intrapleural pr. lung volume intrapulmonic pr. air flows into lungs Expiration (passive) 1. elastic recoil 2. surface tension 3. process thoracic volume pleural volume intrapleural pr. lung volume intrapulmonic pr. air flows out Forced Expiration Compliance -- the ease with which the lungs and thoracic wall can be expanded. It is related to two factors: 1. elasticity 2. surface tension Compliance is decreased with any condition that: 1. destroys lung tissue (emphysema) 2. fills the lungs with fluid (pneumonia) 3. produces a deficiency of surfactant (premature birth, near-drowning) 4. interferes with lung expansion (pneumothorax) Pulmonary Volumes and Capacities 1. clinical respiration 2. tidal vol. (500 ml) 3. anatomic dead space (150 ml) 5. inspiratory reserve volume (3,000 ml) 6. expiratory reserve volume (1,200 ml) 7. residual volume(1,300 ml) 8. vital capacity (4,700 ml) Rates maximum voluntary ventilation = TV x breaths/minute alveolar ventilation rate = alveolar ventilation x breaths/minute Exchange of Oxygen and Carbon Dioxide 1. O2 flows down its concentration gradient by diffusion: alveoli ---> blood ---> interstitial fluid ---> body cells 2. CO2 flows down its concentration gradient by diffusion: cells ---> interstitial fluid ---> blood ---> alveoli 3. diffusion is dependent upon Dalton's law Dalton's law = each gas in a mixture of gases exerts its own pressure as if all of the other gases were not present. 1. The pressure of a specific gas is known as its partial pressure (p). 2. The total pressure of a mixture is the sum of all the partial pressures. 3. Atmospheric air pressure = 760 mm Hg nitrogen = 597 mm Hg + oxygen = 159 mm Hg + carbon dioxide = 0.3 mm Hg + water vapor = 3.7 mm Hg PARTIAL PRESSURES OF OXYGEN EXTERNAL RESPIRATION alveolar air = 104 mmHg deoxygenated (pulmonary arterial) blood = 40 mmHg oxygenated (systemic arterial) blood = 104 mmHg INTERNAL RESPIRATION interstitial fluid = 40 mmHg cytoplasm = <40 mmHg PARTIAL PRESSURES OF CARBON DIOXIDE alveolar air = 40 mmHg deoxygenated (pulmonary arterial) blood = 46 mmHg oxygenated (systemic arterial) blood = 40 mmHg interstitial fluid = 46 mmHg EXTERNAL RESPIRATION INTERNAL RESPIRATION cytoplasm = >46 mmHg External (Pulmonary Respiration) 1. alveoli <---> blood a. deoxygenated ---> oxygenated blood b. loss of CO2 2. diffusion 100% of time 3. rate dependent upon: a. partial pr. differences b. surface area c. diffusion distance d. breathing rate and depth Internal (Tissue Respiration) 1. blood <---> tissue fluid <---> cells a. oxygenated ---> deoxygenated (only 25% O2 given up) b. gains CO2 2. diffusion 100% of time Oxygen Transport 100% 100% oxygen released to tissues at rest 80% 60% 40% 20% oxygen saturation oxygen saturation 1. 98.5% as oxyhemoglobin 2. fully saturated vs partially saturated 3. percent saturation of HB 4. O2 - Hb dissociation curve 5. pO2 most important factor oxygen released to tissues during exercise 80% 60% 40% 20% 20 20 60 100 PO2 (mmHg) 98% 75% LUNGS TISSUES 60 PO2 (mmHg) 100 23% 73% 98% 25% LUNGS TISSUES Oxygen Transport Con’t 6. Hb saturation and pH (Bohr effect) 7. Hb saturation and pCO2 8. Hb saturation and temperature curve shifts to right when: pH decreases, PCO2 increases, temp. increases curve shifts to left when: pH increases, PCO2 decreases, temp. increases Carbon Dioxide Transport 1. 5% dissolved in plasma, 7% exhanged 2. 5% as carbamino-Hb, 23% exchanged 3. 90% as bicarbonate ion, (HCO3-) 70% exchanged a. carbonic anhydrase b. Bohr effect c. chloride shift CO2 + H2O H2CO3 Carbonic anyhydrase H+ + HCO3- IN THE TISSUES SUMMARY diffuses from tissues into blood (RBCs) CO2 + H2O H ion binds Hb in RBC and causes oxygen release (Bohr effect) H2CO3 diffuses into plasma in exchange for chloride ions (chloride shift) H+ + HCO3_ Systemic Gas Exchange (in the Tissues) IN THE LUNGS SUMMARY diffuses into alveoli and breathed away CO2 + H2O H ion released from Hb into RBC cytoplasm H2CO3 H+ + HCO3- diffuses into RBC from plasma in exchange for chloride ions Alveolar Gas Exchange (in the lungs) Respiratory Centers In the medulla Dorsal Respiratory Group Ventral Respiratory Group – Inspiratory neurons – Expiratory neurons In the pons Pneumotaxic Area Apneustic Area Control of Respiration RESPIRATION AT REST active 2 seconds inactive 3 seconds inspiratory neurons diaphragm and external intercostals contract diaphragm and external intercostals relax + elastic recoil and surface tension effects normal resting inspiration normal resting expiration FORCED RESPIRATION diaphragm, external intercostals, scalenes, sternocleidomastoid contract DRG and inspiratory neurons active forced inspiration expiratory neurons of VRG inhibited DRG and inspiratory neurons inhibited inspiratory muscles relax active expiration internal intercostals and abdominal muscles contract expiratory neurons of VRG active Control of Respiration Continued Pons controls transition between inhalation and exhalation A. Pneumotaxic center (overides apneustic) - sends inhibitory impulses to inspiratory area which shortens duration of inhalation before lungs get too full B. Apneustic area - sends stimulatory impusles to the inspiratory area. Prolongs inhalation. Other influences on Respiration 1. cortical influences (chemoreceptors (Co2, H+) 2. Hering-Breuer inflation reflex 3. Proprioceptors 4. Pain receptors cerebral cortex limbic system hypothalamus sleep, exercise, vocalizations, exercise, breath holding, emotional responses pons respiratory group ventral respiratory group dorsal respiratory group altered patterns of breathing Hyperventilation and Hypoventilation What would be the net effect of hyperventilation? CO2 + H2O H2CO3 H+ + HCO3- reaction shifts to the left H+ used to reform carbonic acid used to reform CO2 pH increases increased CO2 lost from the body What would be the net effect of hypoventilation? CO2 + H2O H2CO3 H+ + HCO3- reaction shifts to the right as CO2 accumulates in the body H+ accumulate in the body pH decreases Negative Feedback Control CONTROLLED CONDITION A stimulus or stress disrupts homeostasis by causing a decrease in arterial oxygen and/or increase in hydrogen ions and/or an increase in carbon dioxide RETURN TO HOMEOSTASIS Hyperventilation results in increase in arterial oxygen and/or pH, and/or decrease in arterial carbon dioxide RECEPTOR Chemosensitive neurons in medulla and chemoreceptors in aortic and carotid bodies respond to changes and direct nerve impulses to the control center CONTROL CENTER Inspiratory neurons of medulla interpret sensory input and generate nerve impulses that pass ultimately to effectors EFFECTORS Muscles of inspiration contract more often and more forcefully (hyperventilation) Hypoxia and Positive Feedback CONTROLLED CONDITION A stimulus or stress disrupts homeostasis by causing a decrease in arterial oxygen below 50 mmHg RETURN TO HOMEOSTASIS Hypoventilation results in decreased arterial oxygen, causing greater hypoxia. This leads to positive feedback RECEPTOR Chemosensitive neurons in medulla suffer hypoxia, resulting in the output of fewer nerve impulses EFFECTORS Muscles of inspiration contract less frequently and with less force (hypoventilation) CONTROL CENTER Inspiratory neurons of medulla suffer hypoxia, resulting in fewer nerve impulses to the inspiratory muscles