The Respiratory System
advertisement

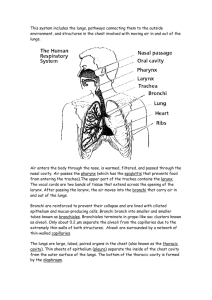
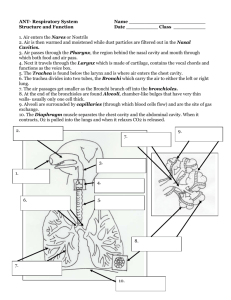
Includes the tubes that remove the particles from incoming air Transport air to and from the lungs Respiration: gas exchange between body cells and atmosphere air sacs Upper respiratory tract: nose, nasal cavity, paranasal sinuses, and pharynx Lower respiratory tract: larynx, trachea, bronchial tree, and lungs Nose: Nostrils: openings for air Nasal Cavity Nasal conchae: divides cavity into passageways bone and cartilage for support Helps increase the surface area of mucous membranes Mucous Membrane filters, warms, and moistens incoming air Ciliary action carries particle trapped in mucus to the pharynx, where they are swallowed Paranasal Sinuses Spaces in the bones of the skull that open into the nasal cavity Lined with mucous membranes Pharynx: behind the oral cavity and between the nasal cavity and larynx Passageway for air and food Larynx: conducts air and helps prevent foreign objects from entering the trachea Composed of muscles and cartilages Lined with mucous membranes Contains vocal cords Vibrate from side to side to produce sound with air passes Glottis and epiglottis help prevent foods and liquids from entering the trachea Trachea: extends into the thoracic cavity in front of the esophagus Divides into the right and left bronchi Bronchial Tree Consists of branched air passages Lead form the trachea to air sacs Alveoli: at the distal end of the narrowest tubes Alveolar ducts Lungs Separated by the mediastinum Enclosed by diaphragm and thoracic cage Visceral Pleura: attaches to the surface of the lungs Parietal Pleura lines the thoracic cavity Each lobe is composed of alveoli, blood vessels, and supporting tissue In 20 minutes your blood pressure will drop back down to normal. In 8 hours the carbon monoxide (a toxic gas) levels in your blood stream will drop by half, and oxygen levels will return to normal. In 48 hours your chance of having a heart attack will have decreased. All nicotine will have left your body. Your sense of taste and smell will return to a normal level. In 72 hours your bronchial tubes will relax, and your energy levels will increase. In 2 weeks your circulation will increase, and it will continue to improve for the next 10 weeks. In three to nine months coughs, wheezing and breathing problems will dissipate as your lung capacity improves by 10%. In 1 year your risk of having a heart attack will have dropped by half. In 5 years your risk of having a stroke returns to that of a non-smoker. In 10 years your risk of lung cancer will have returned to that of a nonsmoker. In 15 years your risk of heart attack will have returned to that of a nonsmoker. credit - Healthbolt Changes in size of the thoracic cavity accompany inspiration and expiration Atmospheric pressure forces air into the lungs Occurs when the pressure inside the alveoli decreases Diaphragm moves downward Thoracic cage moves upward and out Surface tension aids in lung expansion Elastic recoil of tissues and surface tension within alveoli provide the forces of expiration Thoracic and abdominal wall muscles aid expiration Respiratory cycle: one inspiration followed by one expiration Tidal Volume: amount of air that moves in/out during a single respiratory cycle Inspiration Reserve Volume: additional air that can be inhaled Expiratory Reserve Volume: additional air that can be exhaled Residual Volume: air remaining in the lungs after a maximal expiration Vital Capacity: maximum amount of air a person can exhale after taking the deepest breath possible Inspiratory Capacity: maximum volume of air a person can inhale following exhalation of the tidal volume Functional residual capacity: volume of air that remains in the lungs after a person exhale the tidal volume Total Lung Capacity: vital capacity + residual volume Normal breathing is rhythmic and involuntary Respiratory center: brain stem, pons, and medulla oblongata Medullary rhythmicity area: two neuron groups Dorsal respiratory group: basic breathing rhythm Ventral respiratory group: increases inspiratory and expiratory movements during forceful breathing Pneumotaxic area: regulates breathing rate Chemicals, stretching of the lung tissue, and emotional states Chemosensitive area: Blood concentrations of CO2 and H+ influence chemoreceptors Stimulation of these receptors increases breathing rate Peripheral chemoreceptors: located in the walls of certain large arteries Sense low oxygen concentration Increases breathing rate Overstretching lung tissue triggers an inflation reflex Shortens the duration of inspiratory movements Inflation reflex prevents over-inflation of the lungs during forceful breathing Hyperventilation: decreases blood CO2 Very dangerous when done before swimming Gas exchange occurs in the alveoli Alveoli: tiny air sacs clustered at the distal ends of alveolar ducts Respiratory membrane: consists of alveolar and capillary walls Blood and alveolar air exchange gases across membrane Diffusion across the respiratory membrane Partial pressure of a gas is proportional to the concentration of that gas in a mixture or the concentration dissolved in a liquid Gases diffuse from regions of higher partial pressure to lower partial pressure Oxygen diffuses from alveolar air into blood CO2 diffuses from blood into alveolar air Blood transports gases between the lungs and cells Oxygen Transport: blood transports O2 with hemoglobin Oxyhemoglobin is unstable and releases its O2 in regions where PO2 is low More O2 is released when: Blood concentration of CO2 increases Blood becomes more acidic Blood temperature increases May be carried in solution or bound to hemoglobin, or as a bicarbonate ion Most is transport in the form of bicarbonate ions Carbonic anhydrase: enzyme that speeds the reaction between CO2 and H2O to form carbonic acid Dissociates to release H+ and bicarbonate ions Anatomy of Breathing Flash Animation http://teachhealthk12.uthscsa.edu/studentresources/Anatomyof Breathing3.swf