The Respiratory System Notes
advertisement

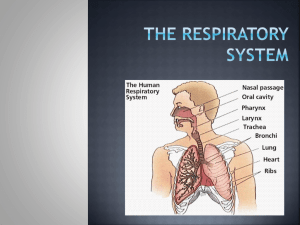
The Respiratory System LUNG CAKE Functions of the Respiratory System Obtain O2 from environment Expel CO2 into the environment Filter foreign particle out of incoming air Regulates H2O content and temperature of incoming air Creates vocal sounds Contributes to sense of smell Helps regulate blood pH Steps for Respiration 1) Breathing or ventilation Moving air in and out of lungs 2) External respiration Exchange of gases between lungs and blood vessels 3) Transport of gases to cells 4) Internal respiration Exchange of gases between blood vessels and cells 5) Cellular respiration Using O2 in metabolic processes to create energy Divisions of Respiratory Tract Upper respiratory tract Nose Nasal cavity Paranasal sinuses Pharynx Lower respiratory tract Larynx Trachea Bronchial tree Lungs Nose Bone and cartilage Support structure Nostrils Openings for entry of air Nose hairs Guard entrance and protect against particles Nasal Cavity Hollow space behind nose Nasal septum Bone and cartilage structure dividing cavity into 2 sides Nasal conchae Projections from nasal cavity wall; increase surface area Lining of nasal cavity Pseudostratified epithelial cells with mucous-secreting goblet cells Particles are trapped and moved out and air is warmed and moistened The NOSE bones and cartilage support nose, two openings (nostrils), hair filters large particles Nasal Cavity – hollow space behind the nose Nasal septum – divides the nose (bone) Nasal conchae – bones that divide the nasal cavity, support the mucus membrane and increase surface area (superior, middle, inferior) * deviated septum – when the septum bends to one side Nasal Conchae Function of the conchae - increase surface area Mucus Membrane warms and moistens air, also traps particles (dust) *particles go to stomach Paranasal Sinuses Air-filled sacs within skull bones Reduce the weight of the skull Affect sound of the voice Paranasal Sinuses - – spaces within the bones maxillary frontal ethmoid sphenoid • • • • reduce the weight of skull and are resonant chambers for voice. Pharynx Shared with digestive system Divisions: Nasopharynx Oropharynx Larygopharynx Otherwise known as hypopharynx Openings: Oral cavity Nasal cavity Esophagus Trachea The three pharyngeal regions Pharynx – behind the oral cavity, between the nasal cavity and larynx (space, not a structure) Larynx Enlargement at beginning of trachea Framework of muscle and cartilage bound by elastic tissue Largest cartilages: Thyroid (Adam’s apple) Cricoid Epiglottic Vocal Cords Housed in larynx False vocal cords Fold of tissue that helps to close passageway when swallowing True vocal cords Vibrate when air is forced through causing sound Tension of chords helps regulate pitch Force of air helps regulate volume of sound Larynx – enlargement at the top of the trachea and below pharynx, conducts air in and out of trachea, houses vocal cords - composed of a framework of muscles and cartilages (thyroid (Adam’s apple), cricoids, epiglottic cartilages) Glottis Triangular opening between vocal cords When swallowing: False vocal cords close glottis Larynx raises and presses epiglottis against opening Glottis - false vocal folds (do not produce sound) – help close airway during swallowing - true vocal folds (produce sound) – changing shape of the pharynx, and oral cavity changes sounds into words - contracting and relaxing muscles changes pitch (increased tension = higher pitch) www.voiceinfo.org Steven Tyler's Vocal Cords Glottis – triangular slit that opens during breathing/talking, and closes during swallowing Epiglottis – flaplike structure that stands upright, allows air to enter larynx, during swallowing it presses downward and prevents food from entering air passages LARYNGITIS When the mucus membrane becomes swollen and prevents the vocal cords from vibrating freely. Trachea (windpipe), flexible cylinder with cartilage to give it stiffness and keep it from collapsing Trachea leads to the BRONCHIAL TREE Trachea Also called windpipe Descends anterior to esophagus Lining of trachea: Pseudostratified epithelial cells with mucoussecreting goblet cells Enclosed with C-shaped rings of hyaline cartilage to prevent tube from collapsing Bronchial Tree Branching tubes connecting trachea to site of gas exchange in lungs Right and left primary bronchi Secondary bronchi Tertiary bronchi Bronchioles Terminal bronchioles Respiratory bronchioles Alveolar ducts Alveolar sacs Alveoli Amount of cartilage decreases through tract Amount of smooth muscle in the walls increases through tract Primary bronchii --> bronchioles --> alveolar ducts --> sacs --> alveoli *gas exchange Alveoli Terminal sacs at the end of the tract Surrounded by network of blood capillaries Site of gas exchange Respiratory membrane: Simple squamous epithelium in alveoli and blood capillary Basement membrane fuses the two (alveoli and capillary) together Alveoli & Lungs ALVEOLI $20,000 PYRAMID! A word/phrase will be posted – person A (who is facing the board) must attempt to explain the word (without saying it!) while Person B (who is NOT facing board) will guess what the word is. NO DRAWING! If your partner gets them all right – with NO CHEATING – raise your hands! GET READY!!!! Alveoli Larynx Trachae Quick Quiz 1. 2. 3. 4. What do you call the bones found within the nasal cavity? What specific bone divides the nasal cavity into two sides? The space at the back of the mouth is the________. The spaces within the bones of the skull are called the ______________________ 5. What structure is known as the windpipe? ______ 6. What is the triangular slit that opens during breathing and talking? 7. In what structures does gas exchange occur? 8. During swallowing, this flap closes to prevent food from entering the airway: ______________________ Lungs Located in thoracic cavity: Mediastinum between Thoracic cage surrounds Diaphragm below Suspended by bronchi and blood vessels Cover by visceral pleura which folds back to become parietal pleura Potential space between is pleural cavity Small layer of serous fluid between Right lung: 3 lobes Left lung: 2 lobes LUNGS - spongy tissue that sit within the pleural cavity Right Lung = 3 lobes Left Lung = 2 lobes Serous fluid lubricates lungs during breathing EXHALATION As the diaphragm and other muscles relax, ELASTIC RECOIL from surface tension forces air out. Muscles can force extra air out or in Inspiration At rest, pressure of air and thoracic cavity are the same; NO net movement of air Pressure must be decreased in thoracic cavity for air to move in Diaphragm is contracted (lowered) and external (inspiratory) intercostal muscles contract as well Contractions increase cavity volume which decreases pressure Inspiration (cont) Muscle movements pull on the pleural membranes to expand the lung Surface tension Difficulty in expanding alveoli because the walls tend to stick together Surfactant helps combat surface tension Deeper breaths can be taken by contracting muscle more forcefully or by involving other muscles Expiration Normally passive process Contracting muscles relax Elastic recoil and surface tension cause tissue to return to previous state before inspiration Pressure increases in cavity and forces air out of lungs Expiration (cont) More air can be expelled if: Internal (expiratory) intercostal muscle contract Pushes rib cage in (raising thoracic pressure even more) Abdominal muscles contract raising abdominal pressure pushing diaphragm higher raising thoracic pressure even more Respiration animation Respiratory Air Volumes Spirometry - measures the amount (volume) of air moving in and out of the lungs Respiratory Cycle - 1 inspiration and 1 expiration ATMOSPHERIC PRESSURE = 760 Hg Pressure is necessary for breathing, which is why it is difficult to breathe in high altitudes and also why a punctured lung can be dangerous. A hole in the pleural cavity can cause the lung to collapse or deflate Pneumothorax = collapsed lung: See Video Also check out this procedure where fluid is drained from the lungs - not for those with a weak stomach! Labeling Practice 1) By YOURSELF – using no notes, text – label the respiratory system diagram • 1 minute time – GO! 2) Switch with someone at your desk 3) Grade the diagram – you may use notes, text • 1 minute – GO! 4) Take a look at diagram key – make any changes! Image adapted from http://www.arthursclipart.org/ Resting Tidal Volume amount of air that enters the lungs during one cycle *take a normal breath Reserve volumes - air that can be forced out or in *inhale normally, pause, and try to inhale more that is your reserve inspiratory volume *exhale, then exhale a little more VITAL CAPACITY = Insp reserve + Exp reserve + Tidal Volume INSPIRATORY CAPACITY = Tidal Volume + Insp Reserve Volume FUNCTIONAL RESIDUAL CAPACITY is the volume of air that remains in the lungs at rest TOTAL LUNG CAPACITY varies by sex, age, body size, athletics Air Volumes Four Respiratory Volumes 1) Tidal Volume 2) Inspiratory reserve volume Amount of air that can be forcefully inhaled over tidal volume (about 3,000ml) 3) Expiratory reserve volume Amount of air moved during one respiratory cycle (resting tidal volume about 500ml) Amount of air that can be forcefully exhaled over tidal volume (about 1,100ml) 4) Residual volume Amount of air left in lungs after the most forceful expiration (about 1,200ml) Air Capacities Four respiratory capacities: 1) Vital Capacity 2) Inspiratory capacity Amount of air that can be inspired after a resting expiration (about 3,500ml) 3) Functional residual capacity Maximum amount of air that can be exhaled after deepest breath (about 4,600ml) Volume of air in lungs after resting expiration (about 2,300ml) 4) Total lung capacity Total amount of air that lung can hold (about 5,800ml) Air Volumes and Capacities (cont) Some volumes and capacities can change with age, sex, body size, and health Anatomical dead space: Air that fills passageways to alveoli; No gas exchange occurs About 150ml Lab- Measuring Lung Capacity Breathing is involuntary, but muscles are under voluntary control Respiratory Center – groups of neurons in the brain that control inspiration and expiration (based in the medulla and the pons) Factors Affecting Breathing *Chemosensitive areas – detect concentrations of chemicals like carbon dioxide and hydrogen 1. Rise in CO2 2. Low blood oxygen (peripheral chemoreceptors, carotid and aortic bodies, sense changes) 3. Inflation reflex – regulates the depth of breathing, prevents overinflation of the lungs 4. Emotional upset, fear and pain Hyperventilation - increase breathing, lower CO2 concentration Breathing into a bag can restore CO2 concentrations Control of Breathing Respiratory center of brainstem controls both inspiration and expiration Medullary rhythmicity area Dorsal respiratory group- emit bursts that cause muscles of inspiration to contract; impulse starts slow and builds; no impulse during expiration Ventral respiratory group - impulse increase inspiratory movements and forceful expiratory movements needed during deeper breathing Pneumotaxic area of pons Controls dorsal respiratory group by inhibiting impulses; as inhibition increases breathing rate increases Factors Affecting Breathing Chemosensitive area within respiratory center Senses changes to CO2 and H+ levels; Increase breathing rate and tidal volume if high Peripheral chemoreceptors in carotid and aortic bodies Sense changes in O2 levels; Increase breathing rate if levels are extremely low Factors Affecting Breathing (cont) Inflation reflex Stimulates pneumotaxic area to inhibit inspiration if tissues in visceral pleura, bronchioles, or alveoli are being overstretched Fear and pain Increase breathing rate Breathing can be voluntary Body will override if breath is held to long Hyperventilation Lowers levels of CO2 in blood; allows for breath to be held longer before levels raise again; can make O2 levels low enough to cause fainting Diffusion at the Respiratory Membrane Partial pressure of gases determine direction of movement Air in alveoli PCO2 = 40 mm Hg PO2 = 104 mm Hg Blood entering capillary PCO2 = 45 mm Hg PO2 = 40 mm Hg Blood leaving capillary - same as alveoli Opposite exchange occurs between the capillaries and tissue Oxygen Transport Over 98% of O2 attaches to heme group of hemoglobin in red blood cells to form oxyhemoglobin Remaining dissolves in blood Hemoglobin releases O2 when: PO2 is low PCO2 is high pH is acidic Temperature is higher Carbon Dioxide Transport About 7% can be transported as CO2 dissolved in the blood 23% is carried by amine group of hemoglobin to form carbaminohemoglobin Releases when PCO2 is low Remaining is carried as bicarbonate ion Bicarbonate Ion Reaction uses enzyme, carbonic anhydrase, in RBC’s Reaction: CO2 + H2O H2CO3 H+ + HCO3- Formation of bicarbonate ion can create excess H+ and create acidic pH; H+ is combined with hemoglobin to minimize this effect Gas Exchange Animation Respiratory Disorders Emphysema Emphysema TV ad Progressive, degenerative disease Destroys alveolar walls Results in air sacs merge to form larger chambers (decreases surface area reduces volume of gases that can be exchanged) Person has trouble breathing Causes: Exposure to respiratory irritants (tobacco smoke, polluted air) Inherited enzyme deficiency Respiratory Disorders Lung Cancer Like all other cancers, uncontrolled division of abnormal cells (rob other cells of their nutrients and gases) Cancer cells divide often to form tumors Can block airways and reduce gas exchange Causes: Exposure to respiratory irritants (tobacco smoke, polluted air) Treated with chemotherapy, surgery Survival rate is low Chronic obstructive pulmonary disease, or COPD, is a longlasting obstruction of the airways that occurs with chronic bronchitis, emphysema, or both. This obstruction of airflow is progressive in that it happens over time. SMOKING IS THE MOST COMMON CAUSE OF COPD & EMPHYSEMA Bronchitis is inflammation of the main air passages to the lungs. Bronchitis may be short-lived (acute) or chronic, meaning that it lasts a long time and Respiratory Membrane – alveoli and blood stream exchange gasses Gas exchange occurs across a membrane a layer of simple squamous cells Oxygen DIFFUSES into the bloodstream Other substances (like alcohol can diffuse too) Hypoxia is a disease in which there is an overall lack of oxygen content within the body's tissue and vital human organs (specifically the brain). Hypoxia has several potential causes, including: cardiac arrest, severe head trauma, carbon monoxide poisoning, suffocation, strangulation, and choking, as well as any instance in which oxygen supply is deprived from the body. Asphyxia is a condition of severely deficient supply of oxygen to the body that arises from being unable to breathe normally. An example of asphyxia is choking. Asphyxia causes generalized hypoxia, which primarily affects the tissues and organs. ILLNESSES RELATED TO THE RESPIRATORY SYSTEM 1. Cystic Fibrosis (genetic) 2. Asthma 3. Bronchitis 4. Apnea 5. Emphysema 6. Lung Cancer 7. Altitude Sickness 8. Chronic Obstructive Pulmonary Disease (COPD) 9. Sinusitis 10. Bacterial or Viral Infections (cold, flu, pneumonia) What is sleep apnea? Pause or slowing of breathing during sleep Video on Sleep Apnea Lung Cancer Lung cancer starts when abnormal cells grow out of control in the lungs. Lung cancer and smoking often, but not always, go hand in hand. There usually are no signs or early symptoms of lung cancer. As lung cancer stages advance, lung cancer symptoms may include coughing, wheezing, shortness of breath, and bloody mucus. Treatment for lung cancer can include surgery, chemotherapy, and /or ALTITUDE SICKNESS Acute mountain sickness is brought on by the combination of reduced air pressure and lower oxygen concentration that occur at high altitudes. Symptoms can range from mild to life-threatening, and can affect the nervous system, lungs, muscles, and heart. Pulmonary edema is an abnormal build up of fluid in the air sacs of the lungs, which leads to shortness of breath NON RESPIRATORY MOVEMENTS Coughing, sneezing, laughing, crying Hiccup - spasm of the diaphragm Yawn - possibly causes by low oxygen levels Respiratory Fun sounds! Cough: Take a deep breath, closes glottis, forces air upward from lungs against closed glottis glottis opens suddenly, blast of air forced upward Sneeze: Like a cough Clears upper respiratory passages rather than lower ones Initiated by mild irritation in nasal cavity Respiratory Fun sounds! Hiccup: Caused by sudden inspiration due to a spasmodic contraction of a diaphragm Air strikes vocal folds causing hiccup sound Yawning: Aid respiration by providing an occasional deep breath