Supplementary Information (docx 113K)
advertisement
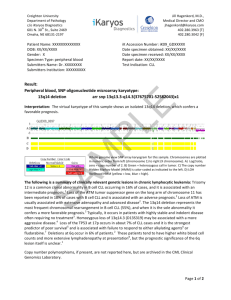
Supplementary Methods Patients Newly diagnosed CLL patients from several Italian Institutions were prospectively enrolled within 12 months of diagnosis into the O-CLL1-GISL protocol (clinicaltrial.gov identifier: NCT00917540). Recruitment began in January 2007 and the criteria for CLL diagnosis employed followed the 1996 NCI/WG guidelines requiring >5,000 lymphocytes/µL in the peripheral blood (1). CLL cell phenotype, CD38 and ZAP-70 expression, and IGHV mutational status were performed in a central laboratory in Genova, while all FISH and genetic analyses were performed in Milan. This study was approved by the ethics committees from each participating center. All patients provided written informed consent to participate in the study. To date the study has enrolled 480 Binet stage A patients. Assessment of biological markers Cytogenetic abnormalities involving deletions at chromosomes 11q23, 13q14, 17p13, and trisomy 12 were evaluated by FISH on a purified CD19+ population (2). CD38-positive leukemic cells were measured by triple staining with CD19-FITC, CD38-PE (both BD Biosciences), and CD5-PC5 (Beckman Coulter). The cells were analyzed using a FACS Calibur flow-cytometer (BD Biosciences). CD38-positive cases were indicated as those having greater than 30% positive cells (3). ZAP-70 was determined by flow-cytometry with a ZAP-70-FITC (clone 2F3.2, Millipore) or an isotype control mAb (mouse IgG2a-FITC, BD Biosciences) as previously described (4,5). We previously demonstrated that 40% of ZAP-70-positive cells represents the best cut-off value for predicting TFS (6), thus, this threshold was used to identify ZAP-70-positive cases in the O-CLL1GISL cohort. IGHV mutational status was assessed using cDNA (5). Sequences were aligned to the IMGT directory and analyzed using IMGT/VQUEST software. Indications for therapy All patients underwent follow-up visits every 6 months. All physicians used the NCI/WG guidelines as reference criterion for starting therapy (1,7) and all patients had a minimum follow-up of 6 months and were evaluated for TFS. Statistical analysis For categorical variables, statistical comparisons were performed using two-way tables for the Fisher’s exact test and multi-way tables for the Pearson’s Chi-square test. TFS was calculated from diagnosis to the first CLL treatment (event) or to last follow-up (censoring). TFS analyses were performed using the Kaplan-Meier method. Statistical significance of associations between individual variables and TFS was calculated using the log-rank test. Independent correlates of the outcome variable were identified by univariate and multiple Cox regression analyses. A value of P<0.05 was considered statistically significant. Continuous variables of prognostic importance on TFS in univariate proportional hazards Cox regression were dichotomized using published thresholds and laboratory norms. ROC curves identified additional thresholds. Robustness (i.e. the internal validity) of the multivariate Cox model was assessed by a bootstrapping resampling technique. In the bootstrapping method, the same multivariate Cox model was fitted 1,000 times using bootstrap sample. Harrell C-statistics were calculated to further evaluate discriminatory value of the progression-risk score (c=1 indicates perfect discrimination; c=0.5 indicates complete absence of prognostic accuracy). The prognostic accuracy of the risk score was further investigated by the Hosmer-May test (a test for analyzing calibration in Cox models) (8), explained variation on outcome (an index combining calibration and discrimination) (9), and Akaike information criterion (AIC) (10). The lower the AIC, the higher the prognostic accuracy of a predictive model. The chances of a given prognostic model to be the best model (among the two candidate models) were assessed by calculating Akaike weights. To calculate these weights, firstly we calculate for each model the relative likelihood, which is just the exp (-0.5 *∆AIC score for that model). The Akaike weight for the model under investigation is this figure divided by the sum of these values across all candidate models. The Harrell C-statistic was performed using STATA version 9; all the other analyses were performed using SPSS Statistics 21. Comparison of progression-risk score with the MD Anderson model Wierda et al proposed a prognostic model for predicting TFS in CLL (12). To compare our progression-risk score with this model, we calculated the total point score in our cohort using the formula proposed by Wierda: I(No. of lymph node sites involved=3) × 7.370 + I(FISH=del11q) × 9.312 + I(FISH=del17p) × 11.285 + (diameter of largest cervical lymph node in cm) × 4.172 + (LDH/100) × I([IGHV gene=mutated] × 5.000 + (LDH÷100) × I(IGHV gene=unmutated)×1.065] + 35.467. The indicator function (I) is equal to 1 if the statement in the parentheses is true and is equal to 0 otherwise. Supplementary References 1. Cheson BD, Bennett JM, Grever M, Kay N, Keating MJ, O'Brien S, et al. National Cancer Institute-sponsored Working Group guidelines for chronic lymphocytic leukemia: Revised guidelines for diagnosis and treatment. Blood 1996;87:4990-4997. 2. Morabito F, De Filippi R, Laurenti L, Zirlik K, Recchia K, Gentile M, et al. The cumulative amount of serum-free light chain is a strong prognosticator in chronic lymphocytic leukemia. Blood 2011;118:6353-6361. 3. Damle RN, Wasil T, Fais F, Ghiotto F, Valetto A, Allen SL, et al. Ig V gene mutation status and CD38 expression as novel prognostic indicators in chronic lymphocytic leukemia. Blood 1999;94:1840–1847. 4. Morabito F, Cutrona G, Gentile M, Matis S, Todoerti K, Colombo M, et al. Definition of progression risk based on combinations of cellular and molecular markers in patients with Binet stage A chronic lymphocytic leukaemia. Br J Haematol 2009;146:44-53. 5. Cutrona G, Colombo M, Matis S, Fabbi M, Spriano M, Callea V, et al. Clonal heterogeneity in chronic lymphocytic leukemia cells: superior response to surface IgM cross-linking in CD38, ZAP-70-positive cells. Haematologica 2008;93:413-422. 6. Morabito F, Cutrona G, Gentile M, Fabris S, Matis S, Vigna E, et al. Is ZAP70 still a key prognostic factor in early stage chronic lymphocytic leukaemia? Results of the analysis from a prospective multicentre observational study. Br J Haematol 2015;168:455-9. 7. Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood 2008;111:5446-5456. 8. Hosmer DW Jr, Lemeshow S, May S. Applied Survival Analysis: Regression Modeling of Time to Event Data, 2nd Edition. Wiley Edition, New York, 2008:191. 9. Tripepi G, Heinze G, Jager KJ, Stel VS, Dekker FW, Zoccali C. Risk prediction models. Nephrol Dial Transplant 2013;28:1975-1980. 10. Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control 1974; 19: 716–723. 11. Wierda WG, O'Brien S, Wang X, Faderl S, Ferrajoli A, Do KA, et al. Multivariable model for time to first treatment in patients with chronic lymphocytic leukemia. J Clin Oncol 2011;29:4088-95.