Dermatology - Clinical Departments
advertisement

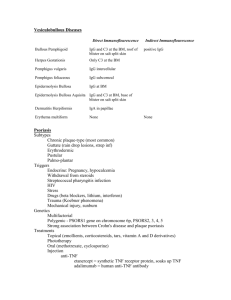
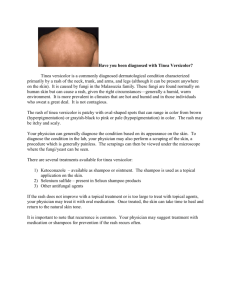
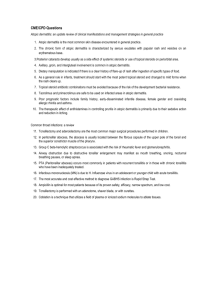
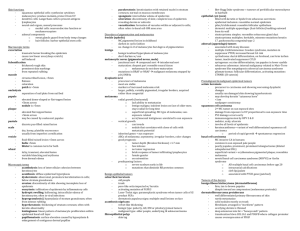
Dermatology Dave Walsh Topics Reviewed last year Common Rashes Eczematous Dermatoses Contact Dermatitis Atopic dermatitis Papulosquamous Dermatosis Psoriasis Pityriasis Rosea Seborrheic Dermatitis Acneiform Eruptions Acne Rosacea Common skin and Nail Infections Superficial Fungal Infections Tinea Candidiasis Viral Skin Infections Herpes Simplex Virus Herpes Zoster Wart Molluscum Topics Reviewed last year (continued) Stings and Bites Scabies Lice Bedbugs Common Neoplasm Basal Cell Carcinoma Actinic Keratosis and Squamous cell carcinoma In situ Squamous Cell carcinoma Keratoacanthoma Malignant Melanoma Foot and Leg Ulcers Venous stasis ulcers Arterial Ulcers Neuropathic ulcers Topics for this talk Treatment of Dermatologic Conditions in Pregnancy Common Rashes Eczematous Dermatoses Hand Dermatitis Xerotic Eczema Nummular Dermatitis Stasis Dermatitis Papulosquamous Dermatoses Lichen Planus Drug Reactions Pigmented Purpuric Dermatoses Miliaria Acontholytic Dermatosis (Grover Disease) Acneiform Eruptions Hidraenitis Suppurativa Common Skin and Nail Infections Bacterial Skin Infections Folliculitis Abscess/furuncle/carbuncle Impetigo Cellulitis/Erysipelas Erythrasma Keratolysis Cuts and Scrapes Topics for this talk (continued) Pruritis Urticaria Autoimmune bullous disease Cutaneous Manifestations of Internal Disease Derm Urgencies and Emergencies Hair Disorders Nail Disorders Disorders of mucous membranes Not covered: Derm diseases of skin of color Aging skin Topical steroids General Rules Ultrapotent steroids should be avoided on the face, groin, and axilla, atrophic skin Clobetasol Exception: ultrapotent steroids used to treat lichen sclerosis of the vulva Creams, ointments, gels, foams, lotions Creams – can be used widely Ointments – greasy feel, bad for hairy areas Lotion, foams, solutions – good for scalp and when large areas of skin need to be covered 30 Gm is needed to cover the skin of a 70-Kg man once Avoid combo steroid-antifungal products unless diagnosis is established A 22-year-old woman is evaluated for acne, which she has had since her teens. She is 2 months pregnant, and the acne seems to be worsening. She has been using over-the-counter benzoyl peroxide products, but the acne is not improving. Medical history is unremarkable, and her only medication is prenatal vitamins. On physical examination, scattered inflammatory papules, a few pustules, and open and closed comedones on the medial cheeks and chin are present Azelaic acid Clindamycin Tazarotene Tretinoin 0% oi n et in ot e za r Ta Tr in yc da m Cl in ca 0% ne 0% c id 0% Az el ai A. B. C. D. Answer Review Azelaic acid – Pregnancy category B Clindamycin – Pregnancy category B Tazarotene – topical acetylenic retinoid – Category X Tretinoin – differentiated retinoid (ATRA) – Category C; usually avoided in pregnancy In general, retinoids have an antineoplastic effect Treatment of Derm Conditions in Pregnancy Risk/benefit ratio Steroids (topical and systemic): category C; although generally considered safe Antihistamines – usually safe in pregancy Teteracycline – Category D – should be avoided Isotretinoin – X – mandatory pregnancy prevention plan Thalidomide – X – mandatory pregnancy prevention plan Spironolactone - avoid Table 4. Selected Pregnancy Category X Drugs to Avoid During Pregnancy and Lactation Acitretin Danazol Estrogens Finasteride 5-Fluorouracil Flutamide Isotretinoin (Accutane) Methotrexate Stanozolol Tazarotene (topical) Thalidomide A 40-year-old woman is evaluated for a rash on her hands that has been present for 6 weeks. This rash comes and goes throughout the year and has been present for many years, but never as severe as it is now. She also experiences itchy skin on her body. She had eczema as a child and currently has seasonal allergies. She is otherwise well and is currently taking no medication. On physical examination, vital signs are normal. She has dry skin on her trunk and extremities. Her hands are extremely dry with scaling, erythema, and fissuring on the dorsal hand surfaces. Her feet are not involved. A. Atopic hand dermatitis B. Keratoderma blenorrhagica C. Scabies D. Tinea manuum 0% m s an uu ie m ne a Ti ha g le no rr ab m de r ra to Ke 0% Sc ab s iti de rm at d ha n At op ic 0% ica 0% Answer Review: Common skin rashes Atopic hand dermatitis – increased prevalence in patients with atopic eczema; sometimes outgrow childhood eczema and then develop atopic hand dermatitis later in life Keratoderma blenorrhagica – erythematous scaly plaques palms and soles associated in with spondyloarthropathy (Reiter syndrome) Scabies – vesicular, itchy rash, burrows, interdigital web, wrist, penis, axillae, nipples, umbilicus, scrotum Tinea manuum –dermatophyte infection of the hand; usually only unilateral upper extremity and bilateral lower extremities Common Skin Rashes: (Eczematous Rashes) Hand Dermatitis – often in people that work that involves water (food services, hairdressers, health care workers) Patch testing can help if atypical/difficult to Rx disease Rx: avoidance of exposure, wear gloves Rx: mid to high potency steroids until rash clears Xerotic eczema – “winter itch”; dry skin, erythematous patches topped by dry tiles. Rx: moisterizers +/- low or mid potency steroids Common Rashes: Xerotic eczema Common rashes continued Nummular dermatitis: Form of eczema coin shaped patches and plaques. Affects patients with a history of atopic ezcema. Check KOH to rule out tinea. Rx: steroids, UVB. Slow to respond to Rx Stasis Dermatitis: Venous problem Older patients Erythema, edema, and brown discoloration, :”woody” DDx: cellulitis (cellulitis more commonly unilateral) Rx: Goal reduce venous HTN: elevation, weight loss Common skin rashes: Papulosquamous Dermatoses Lichen Planus: Idiopathic Skin, hair follicles, nails, mucous membrane 4Ps: pruritic, pink-purple, papules, plaques Lichenoid drug eruption – similar appearance, but associated with ACEi, TZDs, Lasix, b-blockers, anti-malarials Longstanding LP is a risk factor for SCC Rx: topical steroids first line, cola tar, calcineurin inhibitors, and UV therapy are second line. Drug Reactions: Fixed, DRESS, AGEP, EM, SJS, TEN Drug reactions: Can be localized to skin or systemic First step: stop the offending drug Similar appearing to vasculitis and viral exanthems Fixed drug eruptions (antibiotics, NSAIDs, acetaminophen) DRESS: fever, LAD, skin findings, hepatopathy; anticonvulsants; remove offending agent +/- steroids AGEP (acute generalized exanthematous pustulosis): widespread erythema studded by small pustules fever, leukocytosis MCC: Antibiotics, antimalarial, diltiazem, terbinafine Self limiting Rx: removal of agent +/- steroids EM, SJS, TEN – discuss in a bit A 23-year-old woman is evaluated for a very itchy rash for the last 2 days. She also reports “puffiness” in her face and fever. Because she has epilepsy, she was started on a new anticonvulsant 6 weeks ago. She takes no other medication. On physical examination, temperature is 38.7 °C (101.6 °F), blood pressure is 130/78 mm Hg, pulse rate is 106/min, and respiration rate is 16/min. She has facial edema and erythema. She has erythematous pink papules coalescing into plaques that diffusely involve her trunk and extremities. Her mucous membranes are hyperemic but not eroded or painful. Lymphadenopathy is noted in the cervical and axillary regions and inguinal regions. Laboratory studies show a serum alanine aminotransferase level of 330 units/L and a serum aspartate aminotransferase level of 355 units/L. Results of a complete blood count are normal except for 16% eosinophils. 0% 0% 0% o re tic u lar fo rm a L iv ed m ul ti eo s i. .. yt he m n ct io re a Er w it h ex an t.. . d ize al Dr ug en er is e 0% eg C. D. Acute generalized exanthematous pustolosis Drug reaction with eosinophilia and systemic symptoms Erythema multiforme Livedo reticularis cu t A. B. Common rashes: Pigmented Purpuric Dermatoses Miliaria PPD: Group of eruptions that share similarities Red-brown patches and plaques with superimposed petechiae New lesions form over old ones MC of lower extremities; bx shows small vessel disease Bx to rule out T-cell lymphoma, MF Rx: mid to high potency steroids over 6 weeks Miliaria – heat rash; sweat gland rupturing A 66-year-old man is evaluated for a persistent rash for 6 years' duration. The rash waxes and wanes in severity, and it becomes pruritic only after he becomes hot and sweating, such as when he mows the lawn or exercises. It has always been limited to his back and lower chest. He has never treated it. The patient is otherwise well, has no other medical problems, and takes no medication. On physical examination, vital signs are normal. There are small 2- to 3-mm red papules, some with slight scale, on his back and across the lower part of his chest. There are no lesions on his arms, legs, face, soles, or palms. The remainder of the examination is unremarkable Bacterial folliculitis Grover disease Miliairia Pityriasis Rosea Tinea Versicolor Ve rs ico l se a Ti ne a sis ria 0% or 0% Ro ai i li Pi ty se a di ve r Gr o M s iti lic ul lf ol ia ct er 0% ria 0% se 0% Ba A. B. C. D. E. Answer Review: Grover Disease Bacterial folliculitis – acute; not 6 years duration Grover – red papules on chest, flanks, and back that become pruritic with heat; 50 years and older bx shows acantholysis (loss of intercellular connections) Rx: reassurance, cooling, low to mid potency topical steroids Tends to recur regardless of rx Miliaria – should not persist for 6 years Pityriasis rosea – Herald patch, followed by diffuse eruption on torso, usually lasts no more than months Tinea versicolor – scaly hyyper/hypopigmented macules on the trunk and upper arms. Caused by Malassezia furfur, non-itchy, clinically manifests when in hot and humid conditions. A 44-year-old man is evaluated for tender, extremely painful nodules in the axillae and groin area. These lesions drain chronically. The patient is self-conscious about the occasional malodorous discharge. Topical and oral antibiotics have only been minimally helpful. He is a heavy smoker and has a family member with a similar condition that improved with age. On physical examination, vital signs are normal. He has inflammatory nodules with some double comedones in axilla and groin folds, some with drainage and sinus tracts. Skin findings are a ee ts yn dr Sw cg ra n ul o m tiv Py og en i 0% om e 0% a 0% ss up pu ra en it i Ac ne 0% ra d Acne Hidradenitis suppurativa Pyogenic granuloma Sweet syndrome Hi d A. B. C. D. Answer Review: Acneiform Eruption: Hidradenitis suppurativa Acne – no sinus tracts, atypical for axilla Hidradenitis (acne inversa) – follicular occlusion Tender, subcutaneous nodules; may rupture or lead to sinus tract Chronic, sterile abscess Axilla Associated with smoking and obesity Rx: no FDA Rx: tetracycline, surgical removal down to subcutaneous tissues Pyogenic granuloma – bright red/friable papules resulting from capillary proliferation Sweet syndrome – neutrophilic dermatitis; often associated with hematologic malignancies and females after an upper URI. (fevers, arthralgia), myalgia, and cutaneous lesions An 18-year-old man is evaluated for a 3-month history of asymptomatic lesions on the soles of his feet. His discomfort is worsened after wearing running shoes for long periods of time. He also notices odor and attributes it to excessively sweaty feet from his physical activities. He was previously diagnosed with palmar-plantar hyperhidrosis. On physical examination, vital signs are normal. Skin findings are shown di s 0% pe ne a Ti ol y ra t ke d te no rh a en bl 0% sis 0% gic a a 0% th ym Ecthyma Keratoderma blennorhagica Pitted keratolysis Tinea pedis Ec A. B. C. D. Answer Review: Pitted keratolysis Ecythma: saucer shaped, superficial ulcers with overlying crust caused by strep. Associated with IVDU and AIDS Ecythma gangrenosum – similar but caused by pseudomonas Keratoderma blennorrhagica Hyperkeratotic skin lesions on the soles and palms – associated with reactive arthritis Pitted keratolysis: crateriform pitted lesions on pressure areas of the feet associated with hyperhydrosis Typical asymptomatic but odorous. Caused by Kytococcus congolensis Rx: topical macrolide Tinea pedis – interdigital scaling and maceration. Does not present with pitting. Common Skin and Nail Infections Erythrasma Keratolysis Folliculitis: infection of the hair follicle Can be caused by bacteria, fungi, HSV (S. aereus) Dx: clinical; culture if concerned for resistant organism (MRSA) Rx: Topical abx +/- oral anti-staph Abscess/furuncles/carbuncles: Abscess – soft tissue infection Furuncle – abscess that involves a hair follicle Carbuncles – collection of furnucles/folliculitis S. aereus – MCC Dx: clinical Rx: warm compresses, I&D, abx if associated cellulitis, systemic sx, imuunosuppresion, prosthetic joints, abnormal heart valves Should ctx to help tailor abx if needed Common skin and nail infections (continued) Impetigo: S. aureus, strep pyogenes Usually healthy patients Not ill appearing Dx: clinical Rx: topical mupirocin or oral anti-staph Very contagious so hygiene is important Cellulitis: Infection of the deeper layers of skin (lower dermis, subcutaneous fat) staph and strep Nidus of infection include skin breaks, tinea, trauma Dx: usually clinical; bx: only to rule out other etiologies of erythema Rx: B-lactam (cephalexin and/or dicloxacillin) – cover b-hemolytic strep and staph aureus. If no improvement, cover MRSA (clinda, bactrim, tetracycline). Consider broad spectrum up front if immunocompromised. Erysipelas Infection of the superficial lymphatics and upper dermis Usually group A strep Acute onset erythematous plaques that are indurated Dx: clinical Rx: PCN Common skin and nail Infections (continued) Erythrasma Superficial infection caused by Corynebacterium minutissimum Pink brown pathces with fine scales Groin, axilla, intertrigious region Rx: topical macrolide antibiotics (clinda/erythro) Cuts, Scrapes, Burns Tetanus immunization indicated for 2nd degree burns or worse if not updated or unknown immunization. Wounds heal faster when they are kept moist and occluded Don’t give topical abx unless concern for secondary infection Neomycin, bacitracin – frequently cause allergic contact dermatitis Common Neoplasms A 78-year-old man reports a several-year history of developing an increasing number of irregularly pigmented “moles” on the back. The lesions are mostly asymptomatic, although some itch at times, and some may be getting larger. He is concerned they could be melanoma and wonders if they can all be removed. Family history is significant for a sister with melanoma at 55 years of age. Atypical nevi Melanomas Seborrheic keratoses Solar lentigines 0% rl en tig se s So la eb or rh e ic M el ke ra to an om i ev ln 0% in es 0% as 0% At yp ic a A. B. C. D. Answer Review: Seborrheic keratosis Atypical nevi – usually flat, can appear otherwise like seborrheic keratosis Melanomas – another discussion Seborrheic keratosis – benign, waxy, verrucous papules that can be flesh colored to tan. Increase with age. No malignant potential. Lesser-Trelat: rapid growth of multiple seborrheic keratosis assoicated with underlying malignancies Solar lentigines – completely flat; “liver spots”; brown, welldemarcated macules and patches Common Neoplasms Melanocytic nevi (moles) Benign pigmented lesions Birth to first three decades of life Congenital – at birth Compound – raised papules with possible irregular pigmentation Dermal – soft, flesh colored to light brown papules. Dysplastic nevi Melanocytic lesions Biology between benign nevi and melanomas Marker for increased risk for melanoma (although the nevi themselves are not considered precancerous) Need regular physical exams and very careful monitoring Common neoplasms Halo Nevi: Benign Results in a white macule Sebaceous hyperplasia: enlarge oil glands small umbilicated pink or yellowish papules on the face; harmless. Can be mistaken for BCC (telangiectasias should distinguish the two) Neurofibromas Soft, flesh colored asymptomatic papules Isolated NF very common and not associated with genetic conditions Multiple can be a sign of NF (axillary freckles, café au lait, Lisch nodules) Common neoplasms (continued) Skin tags: benign soft, fleshy papules that arise in areas of friction. Rx: remove (cryotherapy or scissor excision) Cherry hemangiomas Benign vascular lesion Bright red smooth papules, usually on trunk Benign, no Rx required A 25-year-old woman is evaluated for a firm “bump” on the leg. It has been present for approximately 3 years and has not changed in size or shape. The lesion is frequently traumatized by shaving. Skin findings are shown sis ic k rh e 0% er at o lc ce l bo r Se en Pi gm a. .. a 0% sa l ba te d al m er Ep id 0% el an om sio n m in clu at of ib ro 0% cy st a 0% De rm Dermatofibroma Epidermal inclusion cyst Melanoma Pigmented basal cell carcinoma E. Seborrheic keratosis M A. B. C. D. Answer Review: Dermatofibroma Dermatofibroma – firm pink brown papules, usually found on legs, When squeezed, they exhibit a “dimple sign”. Benign Epidermal inclusion cyst – benign, non-tender, smooth, firm well demarcated subcutaneous nodules. Central punctum, “sebaceous cysts”, white, cheesy, malodorous material when incised Melanoma – reviewed last year Pigmented basal cell carcinoma – reviewed last year Seborrheic keratosis – reviewed earlier Common Neoplasms (continued) Hypertrophic scars and keloids Occur at the site of injury or surgery Genetic predisposition, MC in darker skin tomes HS – don’t extend beyond site of injury Keloids – extend beyond site of injury; can occur spontaneously Rx: intralesional steroids Pyogenic granuloma Friable red, vascular papules, arise spontaneously and grow fast Collection of capillaries Common in pregnant wome Rx: shave technique or electrodessication Lipomas Benign, collections of fat commonly occur on the trunk and extremities. Asymptomatic, smooth Pruritis Evaluation – determine if related to underlying skin disorder “The rash that itches, or the itch that rashes” MCC – dry skin; Rx: bath every 2-3 days, use moisturizers Skin disorders Dry skin Dermatitis (atopic and allergic) Med reaction, scabies, psoriasis, lichen planus, dermatographism Non-skin disorder related (think systemic conditions) Malignancy (heme), cholestatic liver disease, renal disease, IDA, thyroid dysfunction, meds, HIV Work up: CBC, iron studies, TFTs, BMP, LFTs, CXR, age appropriate maligancy work up Neuropathic itch: Localized itch without skin lesion (damage to sensory nerves) General Rx measures: Rx underlying conditions General skin care, and reuglar emollient use Hot water – worsens histamine mediated itch A 43-year-old woman is evaluated in the emergency department for widespread pruritic wheals. The individual lesions seem to migrate, with each wheal lasting 30 to 60 minutes. The patient says this has been going on for 2 days. There is no accompanying wheezing and no lip or eyelid swelling. The patient is breathing comfortably, has no difficulty swallowing or clearing secretions, and no skin pain. She took diphenhydramine twice yesterday without relief. She has no known drug allergies and just finished a 3-day course of levofloxacin for her third urinary tract infection in the past 6 months. On physical examination, temperature is normal, blood pressure is 110/78 mm Hg, pulse rate is 90/min, respiration rate is 18/min. BMI is 22. There are scattered edematous indurated erythematous plaques consistent with wheals over the scalp, face, neck, chest, upper back, flanks, and arms. The patient has marked dermatographism. There is no wheezing or stridor, no mucosal lesions, and no bullae. 0% 0% 0% in et cy ... ha c . ni .. ea do m in tw ith gh Tr hi Tr ea tw ith ith tw ea po te n ra ne , ce Ad m it t ir iz i to ho sp it a l 0% Tr A. Admit to hospital B. Treat with cetirizine, ranitidine, and diphenhydramine C. Treat with high potency topical steroids D. Treat with indomethacin Answer Review: Urticaria Inflammatory reaction that results from mast cell degranulation Triggers: Infections (viral, bacterial, parasitic) and meds (PCN, beta lactams, vanc, ASA, NSAIDs, opiates, contrast dye), food, stings allergies, chemical exposures (latex), and physical agents (heat, cold, pressure, exercise) Clinically: red, edematous, wheals; acute v. chronic; look for warning/atypical features All acute needs to be evaluated for anaphylaxis Chronic: difficult to assess; 50% idiopathic Atypical features (last > 24 hours, burning sensation, resolve with bruising, fail to respond to anti-histamines) – should be evaluated for underlying vasculitis Food allergies – refer for RAST testing Rx: Acute – H1 and H2 blockade, followed by po steroids on people that don’t resolve; management changes if signs of impending airway obstruction Chronic – colchicine, dapsone, plaquenil, mycophenolate mofetil, MTX If patient has angioedema, they need an epi-PEN A 79-year-old woman is evaluated for pruritic blisters on the chest, abdomen, and lower extremities of 3 to 4 weeks' duration. The blisters arise in crops, drain clear yellow fluid, and crust over before healing. She reports no recent illness and, other than significant itching, feels well. She cannot identify any precipitating causes of the blisters; she reports taking no new medications, using no new topical products, and having no new exposures to plants. She has not been around anyone who is ill or who has had similar skin lesions. Medical history is remarkable only for hypothyroidism secondary to Hashimoto thyroiditis; her only medication is levothyroxine. On physical examination, the patient is afebrile. Typical skin findings are shown :shown . Sk in bx 0% ck ct pr e im pa m ra t un ... io n 0% Tz an PC R an d di re fro m bl ist e rf lu re ul tu lc ia 0% id 0% ct er D. Bacterial culture PCR from blister fluid Skin bx and direct immunoflourescence microscopy Tzanck preparation Ba A. B. C. Answer Review: Autoimmune Bullous Disease Rare, heterogeneous group of unrelated skin disorders Bullous pemphigoid, dermatitis herpetiformis, IgA bullous dermotosis, pemphigous vulgaris Blisters and erosions Cause significant M&M, so recognition and dx are important Dx should be considered when unexplained blisters or erosions are seen Skin bx +/- blood testing (circulating auto-antibodies) Rx: Most diseases have systemic steroids or other immunosuppressants (azathioprine, MTX, cyclophosphamide, Cellcept) as part of Rx. Often require multiple drugs Cutaneous Manifestations of Internal Disease Rheum Covered in Rheum lecture Nephrology Pruritis: discussed earlier Calciphylaxis: necrotic tissue caused by vascular calcifications Rx: Sodium thiosulfate, wound care Nephrogenic systemic fibrosis Distal extremity thickening, fibrosis, limited mobility Dx: clinical, bx can confirm Suspected to be related to gadolinium based MRI Post – Tx: Think about non-melanoma skin cancers (especially SCC) Pulmonary Sarcoidosis: Violaceous papules and infiltrative plaques Granulomas at the site of trauma (surgical scars or tattoos) Lupus pernio Erythema Nodosum in Lofgren syndrome (can also be seen as the result of abx, ocp, HRT) Gastroenterology IBD: Erythema Nodosum and pyoderma gagrenosum ESLD Covered in liver Heme/Onc Sweet Syndrome Covered previously Endocrine Covered in endocrine ID HIV Covered previously A 22-year-old man is evaluated for lip erosions and a new rash on the palms. A representative example of the skin findings is shown 0% 0% lla ic e Va r Gr o up A o st re zo st e p r 0% B1 9 0% Pa rv HSV Parvo B19 Group A strep Varicella zoster HS V A. B. C. D. A 37-year-old woman is evaluated in the emergency department for a 24-hour history of peeling skin. She was recently treated for a urinary tract infection with trimethoprimsulfamethoxazole. Several days into treatment, she developed fever followed by fine, red, itchy papules on her torso and extremities. She continued the antibiotics, the rash worsened, and her skin became painful during the next few days. This morning, she awoke with sores in her mouth, and when she touched her skin it peeled off. She takes no other medications and has no documented allergies. On physical examination, she appears acutely ill and is in pain. Temperature is 39.4 °C (102.9 °F), blood pressure is 100/60 mm Hg, pulse rate is 106/min, and respiration rate is 20/min. The skin shears when lateral pressure is applied to areas of erythema. Erythema and crusting are present around the eyes and on the lips, and open erosions are present in the mouth. The vulva has superficial erosions. Skin findings are shown :shown . The patient is admitted to the intensive care unit, and aggressive intravenous fluid replacement is begun. 0% bx kin Va n as n Ob ta in gi tic os te r lc or to pi ca n gi Be 0% .. . ds ro i st e co co rti iv n gi 0% c 0% Be Begin iv corticosteroids Begin topical corticosteroids Begin Vanc Obtain a skin bx Be A. B. C. D. Derm Urgencies and Emergencies: Erythema multiforme, SJS, TEN EM SJS TEN SJS/TEN – Morphology Typical three-zoned target Atypical targets and confluent erythema with sloughing Distribution Favors extremities Trunk, extremities Up to 10% BSA involvementa Trunk, extremities At least 30% BSA involvementa Mucosal disease (oral, eye, genitourinary) One or two sites Two or more sites Two or more sites Constitutional symptoms + ++/+++ +++ Extensive, confluent erythema with sloughing antiseizure medications, NSAIDs, abx, PPI, sertraline, tramadol, allopurinol Dx: clinical; bx Caused by infection (%) (herpes simplex or Mycoplasma pneumoniae) 30-80 22 6 confirms Rx: Caused by drugs implicated in (%) Up to 50 74 94 Mortality (%) 0 5-13 25-39 1. Supportive (fluid, electrolytes, wound care) 2. dc offending agent A 58-year-old man is evaluated for a 3-year history of an itchy, scaly rash. It began as patches and plaques but over the past several months has progressed to a generalized, red skin rash. The pruritus is intense and interferes with his life. His only other medical problem is hypertension for which he has taken lisinopril for the past 5 years. On physical examination, vital signs are normal. He has erythema with scales affecting more than 90% of the body surface area. Skin findings are shown :shown . He also has alopecia, thickening of the nails, palms, and soles, and nail dystrophy. Generalized lymphadenopathy is also present. St ap h sc a in ld ed sk lar re Pu st u vit y sit i se n hy pe r 0% sy n. .. sis 0% ps or ia ... m ph o m l ly el -c Dr ug ou sT an e Cutaneous T-cell lymphoma Drug hypersensitivity reaction Pustular psoriasis Staph scalded skin syndrome Cu t A. B. C. D. 0% a 0% Answer Review: Erythroderma Erythroderma: erythema (inflammation) of at least 80% skin surface Erosions from severe pruritis, peripheral edema, scaling, LAD Difficult to find underlying cause Acute caused by uncontrolled dermatosis, meds, idiopathic Alopecia, nail dystrophy, thickening of the palms and soles of the feet indicate long term erythroderma T-cell lymphoma, GVHD, psoriasis Dx: largerly clinical; bx has high rate of being non-specific Rx: stop the medication if involved, referral to dermatologist, supportive care A 21-year-old man is evaluated for a 1-month history of hair loss in a small, oval patch on the scalp. He indicates that a similar process occurred several years ago in a different location on the frontal scalp, but the hair re-grew spontaneously. He has no hair loss elsewhere. He is in excellent health and takes no medications. His family history is significant for Hashimoto thyroiditis in his mother. On physical examination, the scalp appears normal, without inflammation or scale. Scalp findings are shown :shown . s 0% Ti ne a Ca p iti um ef ge n lo Te ne t og e An dr 0% flu vi op ec ic c ia al ar 0% Lu pu s 0% ia ea ta 0% op e Alopecia areata Androgenetic alopecia Lupus Telogen effluvium Tinea Capitis Al A. B. C. D. E. Hair Disorders Alopecia (hair loss) Scarring v. non-scarring (bx can distinguish) Non-scarring: PCOS, thyroid dysfunction, IDA, meds (beta blockers, anti-siezure, coumadin, oral retinoids) alopecia areata telogen effluvium (diffuse hair loss triggered by stress) Androgenetic (male/female pattern baldness) Scarring Alopeica: Traction CCCA (central centrifugal cicatricial alopecia) “hot comb alopecia” Lichen planopilaris (associated with lichen planus elsewhere) discoid SLE A 30-year-old man presents with concern about nail changes. He underwent induction chemotherapy for acute myeloid leukemia approximately 1 month ago and has done well in the interim. He is currently afebrile, has no systemic complaints, and his vital signs are normal. His kidney and liver chemistry studies are normal. Nail findings are shown :shown . sis 0% Ps or ia ld ys tro an us L ic he n pl lin 0% ph y 0% es 0% ai Beau lines Lichen planus Median nail dystrophy Psoriasis Be au A. B. C. D. Answer Review: Nail Disorders Psoriatic nail changes: pitting, onycholysis, “oil drop sign”, multiple nails, no correlation with disease severity Lichen Planus – pitting, pterygium formation, and onycholyis Melanonychia (picture) and subungal melanoma Single nail affected is suggestive of an underlying melanocytic lesion (melanoma) Subungal melanoma: rare in Caucasians, but MC type of melanoma in Asian and black patients Beau lines – transverse linear depressions that occur during severe illness/stress Median nail dystrophy – logitudinal depression ususally involving 1-2 nails usually the result of trauma. Most commonly occurs in the thumb Onychogryphosis – thickening/yellowing of nail plate see in elderly patients “Ram horn” deformity Rx: Trimming the nails +/- ablation of the nail matrix A 35-year-old man presents with a 6-month history of small polygonal violaceous papules on the wrists bilaterally and a white, lacy, discoloration on the buccal mucosa of the cheeks bilaterally. The white lacy areas do not come off when scraped with a tongue depressor. The affected areas in the mouth occasionally ulcerate and become tender. The patient is in excellent health, takes no medications, and has no history of chronic disease or immunosuppression. Oral mucosal findings are shown 0% 0% lak ia an us uk op pl n le air y al h Or Ca n di d ia rs lce us u 0% sis 0% L ic he Aphthous ulcers Candidiasis Lichen planus Oral hairy leukoplakia Ap ht ho A. B. C. D. Answer Reviewed: Disorders of Mucous Membranes Aphthous ulcers: Small tender ulcers that occur on tongue and buccal mucosa Candidiasis: Discussed previously Lichen planus: Idiopathic autoimmune disease of skin and mucous membranes mucous membrane findings: white, reticulated network on the buccal mucosa; desquamative gingivitis; chronic erosions of the oral or vulvar mucosa Oral hairy leukoplakia: Wrinkled, white adherant plaques that generally occur on lateral aspects of the tongue; no ulceration; HIV; Etiology – EBV Oral Melanotic macule: Brown, macules on lower lip, singular, benign Need to remove if atypical to r/o melanoma Erythroplakia: Erythematous, velvety plaques on tongue, need to bx Actinic cheilitis: Erythema, scaling, and fissuring of the lower lip Rx: with cryotherapy, imiquimod, laser therapy (high rate of carcinoma) Black Hairy Tongue Hypertrophy and filiform papillae on dorsum of the tongue Caused by abx, coffee, tea, poor hygiene, and tobacco SCC: Reviewed previously; MCC of intraoral malignancy A 26-year-old man is evaluated for a firm, smooth nodule. This appeared several weeks after trauma to the area and enlarged steadily until reaching its current size. The nodule is occasionally tender, but is otherwise asymptomatic. Skin findings are shown In tra on e c in ol la pi ca m ra i lt pi ca al p Or To To le sio na l tri a m c in ol o. . re dn is o ne A. Intralesional triamcinolone injections B. Oral prednisone C. Topical abx D. Topical traimcinolone bx 25% 25% 25% 25%