Be Suspicious of Scabies

Dermatology
“Doc, I Have This Rash…”
Joseph S. Baler M.D.
September 7, 2013
Guttate Psoriasis
• Small pink papules with scale.
• Scalp, face, trunk, and ext.
Guttate Psoriasis
• 2-3 wks post group A strep.
• Personal or family h/o psoriasis.
• May be initial psoriatic event.
• Post sunburn.
• Viral URI.
Guttate Psoriasis
• Look for Strep.
• Pen VK 500mg BID.
• Topical mid potency steroids such as TAC
0.1% cream.
• NBUVB , Sunlight.
• Do not use
Prednisone!
Photodermatitis
Phototoxicity Photoallergy
• Sunburn reaction, erythema, edema.
• Pruritic, eczematous lesions.
• Direct tissue injury
• Type IV delayed hypersensitivity.
• Occurs after first exposure.
• Onset minutes to hours.
• Does not occur after first exposure.
• Onset 24-48 hours.
• Large dose of agent needed for eruption.
• Small dose of agent .
Phototoxicity Photoallergic
Phototoxic agents
• Systemic:
Tetracyclines,
Phenothiazines,
Thiazides, Furosemide,
Sulfonylureas.
• Topical:
Furocoumarins: lime, lemon, celery, tar.
Photosensitivity/Doxycycline
Photoallergic agents
• Systemic:
Quinolones,NSAIDs, sulfonamides.
• Topical:
Fragrances.
Photocontact/Allergic Contact
Dermatitis
?
• At beach.
• Having a refreshing drink with a twist of lime.
Phytophotodermatitis
• Limes have psoralens containing compounds that are phototoxic.
• Oil of Bergamot
Phytophotodermatitis
• Initial onset erythema or blisters after contact and sun exposure. May be absent.
• 48-72 hrs later hyperpigmentation at sites of contact.
• May persist up to 4-6 weeks
Phytophotodermatitis
• Biting into lemon
• Squeezing limes
?
Allergic Contact Dermatitis-Mangos
• Mango skins have urushiol which is same as poison ivy
• Oil from skin of mango drips onto skin creating contact dermatitis
Poison Ivy
• Leaves and vine can cause rashes
• Any season
• Sensitivity varies from person to person
• Three leaflets
Poison Ivy
• Look for linear blisters or erythema
• Very pruritic
• Blister fluid is not contagious
Poison Ivy
• New areas may develop over time due to small areas of chemical contact taking longer to react.
• Resin from plant called urushiol can oxidize and turn black on the skin which is called a “black lacquer spot”
Treatment
• Ultra potent topical steroids if a localized area such as clobetasol propionate 0.05%
• Systemic steroids often needed
• Medrol dose pack too little, and too short
• Prednisone 40-60mg with a slow taper over
12-18 days, maybe longer if reactivation
• Ivy Block etc. may help prevent the oils from the plant getting to the skin by acting as a barrier which you apply as a lotion prior to potential contact
• Wash all clothes, tools, shoes, and gloves after contact since resin may last for years even when air dried.
Swimmer’s Itch
(clam digger’s itch)
Sea Bather’s Eruption
Swimmer’ Itch Sea Bather’s Erupt.
• Water: fresh or salt
• Water: salt
• Body part: uncovered
• Locale: North US and
Canada
• Cause: cercarial forms of nonhuman schistosomes(snails)
• Body part: covered
• Locale: Florida and
Cuba
• Cause: larval forms of marine coelenterates
(sea anemone, jellyfish)
Treatment/Prevention
• Swimmer’s itch: symptomatic Rx for itch.
Vigorous towel drying may prevent penetration of the cercariae
• Sea Bather’s eruption: symptomatic Rx for itch.
Remove swimwear before shower since fresh water may cause discharge of nematocysts. Heat dry swimwear
Swimmer’s Itch
(clam digger’s itch)
Sea Bather’s Eruption
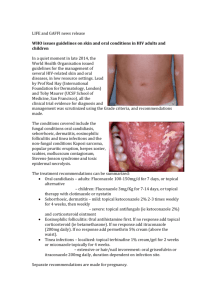
Tinea Versicolor
Tinea Versicolor
• Malassezia furfur
• Normal cutaneous flora
• 2-8% US population
• Warm, humid enviroment
• Very common in tropical regions of world
• Immunosupression,
Cushings disease
• Hyper and hypopigmented macules with fine scale
• Hypopigmentation caused by tyrosinase inhibition
• Hyperpigmentation caused by enlarged melanosomes
• KOH: short hyphae and spores “spaghetti and meatballs”
Tinea Versicolor - Treatment
• Topical anti-fungals
• Selenium sulfide 2.5% lotion
• Oral ketoconazole 400mg single dose, repeat in 1 week
• Fluconazole 200-400mg weekly 2-4 weeks
• Itraconazole 200mg QD x 7 days
Pityriasis Rosea
Pityriasis Rosea
• Pruritic, oval, salmoncolored macules with collarette scale
• Herald patch on neck or trunk, then 1-2 wks later smaller lesions
• Lasts approx. 12 weeks
Pityriasis Rosea
• Follows skin creases
• Can have atypical cases which are more papular, vesicular, or widespread
Pityriasis Rosea
• Probable viral etiology, but no definitive data
• Clusters during spring common
• Not contagious
PR- Treatment
• Symptomatic for itch: antihistamines, topical steroids
• UVB, sunlight helpful
Perioral Dermatitis
• Acneiform lesions.
• Erythema and scale.
• Common in women.
• Etiology unclear, but topical steroid use often the cause.
Perioral Dermatitis
• Perioral and perinasal most common.
• Occasional periocular.
Treatment Perioral Dermatitis
• Avoid high potency topical steroids.
• If topical steroids have been used for longer than 1 month prior to diagnosis, may need to use a mild (1%) hydrocortisone cream to prevent rebound flare.
Treatment Perioral Dermatitis
• Oral antibiotics: Doxycycline, and minocycline good choices
• Topicals: Clindamycin lotion, metronidazole gel, lotion
• Elidel and Protopic have shown some promise
Perioral Dermatitis
• Remember : topical steroids are most often the cause, not the cure.
What is it ?
• Annular
• Raised scaly boarder
• Central clearing
• Pruritic
Tinea Corporis
• Tinea
Differential Diagnosis
• Nummular eczema
Nummular eczema
• Annular
• No central clearing
• Pruritic
What to do?
• KOH
• Look for other signs of eczema: dry skin, atopy, h/o eczema
• If in doubt treat with topical antifungal first
• If you use topical steroid first, it will flare a fungal infection
• Be careful with betamethasone/clotrimazole combination
• Never more than 2 weeks
• The betamethasone component too potent for most fungal infections, and high risk of steroid atrophy
• Worsening tinea
• Striae
Treatment
• Topicals: Econazole, Ketoconazole etc….
• Keep dry
• Be patient
Tinea Capitis
Most common under age 15.
It is rare in adults.
Sebaceous gland maturity is protective against Tinea in scalp
• Scale, loss of hair, other siblings with same
• If healthy adult with similar clinical picture, think psoriasis or seborrhea
Tinea Capitis
US: Trichophyton tonsurans most common
Europe:
Microsporum canis and audouinii most common
Woods lamp not always helpful since
Trichophyton do not fluoresce.
(microsporum do)
KOH and culture to diagnose
Treatment of Tinea Capitis
• Systemic rx needed
• Griseofulvin ultra microsized
250mg bid 8-16wks until clear
• Griseofulvin Suspension 20-25 mg/kg/day for younger children
• Lamisil
10-20kg, 62.5mg/d
20-40kg, 125mg/d
>40kg, 250mg/d
KERATOSIS PILARIS
Keratosis Pilaris
• Hyperkeratotic erythematous follicular papules
• Cheeks, arms, thighs, occ. trunk
• Genetic: Autosomal
Dominant
Keratosis Pilaris
• Cheeks improve at puberty. Other sites persist
• Improves in summer, worse in winter
• Treatment
– Ammonium lactate 12%, salicylic acid 6% , urea
40-50%.
– Topical retinoids occasionally
Pityriasis Alba
• Don’t confuse Pityriasis alba with Tinea Versicolor
• Pityriasis alba more often associated with atopic dermatitis
• Hypopigmented, erythematous dry patches. Face and arms.
Pityriasis Alba Treatment
• Emollients and keratolytics:
Ammonium lactate
12%, Salicylic acid
6%.
• Low potency topical corticosteroids: 1%
HC, Desonide 0.05%.
Lichen Planus
• Purple, pruritic papules
• Wrists, legs, trunk, genitals, and scalp
• May hyperpigment as it resolves
• White streaks over surface – Wickham’s striae
• Adults > children
• Oral involvement with whitish lacy patches
• May ulcerate
• Risk oral SCC
• Nail LP may cause chronic changes
• Scalp LP called
Lichen Planopilaris.
• May cause scarring alopecia
• Immune mediated.
• May be associated with
Hep C
Treatment LP
• Topical corticosteroids
• Oral steroids if severe
• UVB, PUVA
• Oral Retinoids
• Protopic ointment 0.1% for oral disease
• Hydroxychloroquine, Mycophenolate Mofetil, and recently Pioglitazone for Scalp LPP
SCABIES
(Sarcoptes Scabiei var Hominis)
SCABIES
• Very pruritic
• Burrows and erythematous papules
• Nipples, areola
• Glans penis, scrotum
• Finger webs, axilla
• Female mite causes symptoms. Male dies after fertilization
• 5-15 mites per patient
• Ova or feces may be found
• Crusted (Norwegian) scabies has hundreds to millions of mites
• Live up to 48hrs off host
• Nursing homes, group homes etc.
• Scraping may be negative
If your patient has:
• Chronic itch
• Worse at night
• Others with itch in household
• No other obvious cause
• Be Suspicious of
Scabies
Scabies Treatment
• 5% Permethrin cream (Elimite) neck to toes (occasionally face and scalp ) overnight. Repeat in 1 week
• Treat others in house
• No need for lindane
• Change bedding after each treatment
• Ivermectin 150-200 mcg/kg single dose. May repeat in 1 week
Dermatology
“Doc, I Have This Rash…”
Joseph S. Baler M.D.
September 7, 2013