Ch 25 Skin Money [5-11
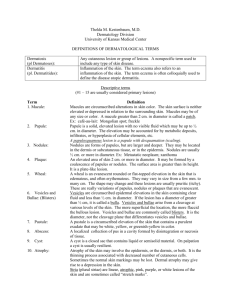
advertisement

Skin functions squamous epithelial cells: synthesize cytokines melanocytes: produce melanin, protect from UV dendritic cells: Langerhans cells to present antigens lymphocytes neural end organs, axonal processes o merkel cells: neuroendocrine function or mechanoreceptors adnexal components o sweat glands: guard from body temp changes o hair follicles: harbor epithelial stem cells Macroscopic terms excoriation traumatic lesion breaking the epidermis cause raw linear area (deep scratch) self induced lichenification thickened rough skin prominent skin markings from repeated rubbing macule circumscribed lesion, <5mm flatness coloration patch is >5mm oncholysis separation of nail plate from nail bed papule elevated dome-shaped or flat-topped lesion <5mm across nodule is >5mm plaque elevated flat-topped lesion >5mm across may be caused by coalescent papules pustule discrete pus-filled raised lesion scale dry, horny, platelike excrescence usually from imperfect cornification vesicle fluid-filled raised lesion <5mm across bulla >5mm blister is common term for both wheal itchy, transient, elevated lesion variable blanching and erythema from dermal edema Microscopic terms acantholysis: loss of intercellular cohesion between keratinocytes acanthosis: diffuse epidermal hyperplasia dyskeratosis: abnoromal, premature keratinization in cells; below stratum granulosum erosion: discontinuity of skin showing incomplete loss of epidermis exocytosis: infiltration of epidermis by inflammatory cells hydropic swelling: ballooning; intracellular edema of keratinocytes; often in viral infections hypergranulosis:D hyperplasia of stratum granulosum; often from intense rubbing hyperkeratosis: thickening of stratum corneum; often with keratin abnormality lentinginous: linear pattern of melanocyte proliferation within epidermal basal cell layer papillomatosis: surface elevation caused by hyperplasia & enlargement of contiguous dermal papillae - parakeratosis: keratinization with retained nuclei in stratum corneum; normal on mucous membranes spongiosis: intercellular edema of epidermis ulceration: discontinuity of skin; complete loss of epidermis revealing dermis or subcutis vacuolization: formation of vacuoles within or adjacent to cells; often refers to basal cell-BM zone area Disorders of pigmentation and melanocytes freckle (ephelis) MC pigmented lesion in childhood darken in cyclic fashion no change in # of melanocytes but degree of pigmentation lentigo benign localized hyperplasia of melanocytes don’t darken w/ sun melanocytic nevus (pigmented nevus, mole) junctional nevi compound nevi intradermal nevi maturation: deepest part resemble neural tissue o melanomas do not show maturation mutations in BRAF or NRAF malignant melanoma stopped by p16/INK4a dysplastic nevi precursors of melanoma most are stable markers of increased melanoma risk larger, pebbly, variably pigmented, irregular borders, acquired rather than congenital melanoma radial growth (horizontal) o lack ability to metastasize o lentigo maligna: indolent lesion on face of older men; stays radial for long time o superficial spreading: MC type of melanoma; sunexposure related o acral/mucosal lentiginous: unrelated to sun exposure vertical growth o can invade o nodule that correlates with clone of cells with metastatic potential inherited genes + sun exposure ABCs of melanoma: asymmetry, irregular borders, color changes good prognosis: o tumor depth (Breslow thickness) <1.7 mm o few mitoses o no tumor regression o brisk response of tumor infiltrating lymphocytes o female gender o on extremities predisposing factors: o severe sunburn early in life o mutations that diminish RB proteins common Benign epithelial tumors seborrheic keratosis old people trunk pore-like ostia impacted w/ keratin activating mutation of FGFR3 Leser-Trelat sign: paraneoplastic syndrome when tumor cells of GI product FGFa dermatosis papulosa nigra: multiple small lesions on face acanthosis nigricans velvet-like thickening benign type: puberty, AD, DM or pituitary/pineal tumors malignant type: older people, underlying GI adenocarcinoma fibroepithelial polyp skin tag - Birt-Hogg Dube syndrome = tumrors of perifollicular mesenchyme in hairbulb epithelial cyst (wen) filled with keratin or lipids from sebaceous secretions epidermal inclusion: resembles normal epidermis pilar/trichilemmal: resemble follicular epithelium dermoid: multiple appendages (hair follicles) budding outward from its wall steatocystoma simplex: resembles sebaceous gland duct steatocystoma multiplex: heritable, missense mutations keratin 17, pachyonychia congenital type 2 adnexal (appendage) tumors associated with many diseases multiple trichilemmomas: Cowden syndrome, mutation in suppressor PTEN, increased breast CA risk cyclindroma: ductal differentiation, on forehead, can form turban tumor, inactivated suppressor CYLD syringomas: eccrine differentiation, tan papules in lower eyelids sebaceous adenomas: internal malignancy related in Muir-Torre syndrome like nonpolyposis colorectal carcinoma syndrome pilomatricomas: follicular differentiation, activating mutations CTNNB1 (B-catenin) Premalignant & malignant epidermal tumors actinic keratosis precursor to carcinoma and showing worsening dysplastic changes usually sun damaged skin showing hyperkeratosis may develop keratin “cutaneous horn” <1cm sandpaper consistency squamous cell carcinoma 2nd MC tumor on sun exposed sites damage from exposure to UV proportional to sun exposure time P53 damage occurs early immunosuppression by HPV 5 & 8 nodular, scaly, ulcerate involve all levels of epidermis keratoacanthoma = variant of well differentiated squamous cell carcinoma o period of rapid growth spontaneous regression basal cell carcinoma MC invasive CA in humans common in sun exposed pale people pearly papules, prominent, prominent telangiectasias (dilated subepidermal BVs) superficial variant = erythematous pigmented plaque; resembles melanoma nevoid basal cell carcinoma syndrome (NBVVS) or Gorlin syndrome o AD multiple basal cell carcinomas before age 20 o intracranial calcifications o cleft lip/palate o associated with PTCH gene (patched) Tumors of the dermis benign fibous histiocytoma (dermatofibroma) firm, tan to brown papules dimple inward on compression (melanomas protrude) dermatofibrosarcoma protuberans well differentiated primary fibrosarcoma of skin rarely metastasize solid nodules mostly on trunk fibroblasts arranged in “storiform” pattern overlying dermis is thinned deep extension into fat = “honeycomb” pattern translocation btwn COL1A1 and PDGFB where collagen promoter causes overexpression of PDGF Tumors of cellular migrants to skin mycosis fungoides (cutaneous T cell lymphoma) chronic proliferative process may evolve into generalized lymphoma red patches, scaling plaques, fungating nodules development of large multiple red nodules correlates to systemic spread Sezary syndrome: seeding of blood by malignant T cells w/ erythemia & scaling of entire body (erythroderma) Sezary-Lutzner cells = histologic hallmark of CTCL; T helper cells CD4+ forming bandlike aggregates in superficial dermis o small clusters = Pautrier microabscesses mastocytosis mast cell degranulation release histamine & heparin urticarial pigmentosa o children, occurs for 50% o multiple round red nonscaling papules Darier sign: localized dermal edema & erythemia when lesion rubbed Dermatographism: edema resembling hive in normal skin due to stroking w/ pointed instrument point mutation in c-KIT receptor tyrosine kinase Disorders of epidermal maturation icthyosis green root “fishy” excessive keratinization looks like scales defective desquamation buildup of compacted stratum corneum X-linked = deficiency of steroid sulfatase impaired epidermal maturation Acute inflammatory dermatoses urticaria (hives) wheal and flare = pruritic edematous plaques o occur in areas exposed to pressure (trunk, extremities, ears) o superficial dermal edema IgE mediated type I hypersensitivity o dependent: antigens (pollen, food) o independent: degranulation of mast cells (opiates, antibiotics, aspirin) acute exzematous dermatitis (“to boil over”) allergic contact dermatitis: poison ivy o Langerhans cells present to CD4+ and memory cells recruit inflammatory cells on next exposure within 24 hrs UV light injurious to Langerhans cells and prevent sensitization atopic dermatitis drug-related eczematous dermatitis photoeczematous dermatitis primary irritant dermatitis erythema multiforme hypersensitivity rxn to infections, drugs, collagen vascular dz o macules, papules, vesicles, bullae o target lesions Steven-Johnson syndrome = febrile, children, erosion of skin & mucous membranes toxic epidermal necrolysis = diffuse necrosis & sloughing of cutaneous & mucosal epithelial surfaces (analogous to burns) epithelial cells killed by skin homing (CLA+) CD8+ CTLs Chronic inflammatory dermatoses psoriasis well-demarcated pink to salmon-colored plaques w/ silver-white scale arthritis, myopathy, enteropathy, spondylitic joint disease, AIDS - - elbows, knees, scalp, lumbosacral areas, intergluteal cleft, glans penis nail changes: yellow-brown, pitting/dimpling/separation pustular psoriasis = pustules form on plaques o can become generalized and life threatening w/ fever, leukocytosis, arthralgia, electrolyte problems stratum granulosum thinned or absent & extensive overlying parakerototic scale seen o auspitz sign = minute bleeding points when scale lifted from plaque HLA-C & TNF major factors Koebner phenomenon = psoriatic lesions induced by local trauma where inflammatory response promotes lesions seborrheic dermatitis areas w/ sebaceous glands (scalp, forehead, face, presternal area) o not a disease of these glands though often presents as dandruff Leiner disease: generalized and associated w/ diarrhea and FTT Cradle cap: infants HIV: worse prognosis worse in Parkinson disease ( sebum as result of dopamine) Yeast Malassezia furfur may cause lichen planus 6 P’s: pruritic, purple, polygonal, planar papules, plaques Resolves in 1-2 years Wickham striae: papules w/ white dots/lines by areas of hypergranulosis Civatte bodies (colloid): anucleate necrotic basal cells Lichen planopilaris: lichen planus affecting epithelium of hair follicles Blistering (bullous) diseases inflammatory Pemphigus o IgG Autoantibodies that result in dissolution of intracellular attachments within the epidermis and mucosal epithelium o Can be life threatening o Pemphigus vulgaris: most common type, effects mucosa and skin May present as oral ulcers months before on skin Suprabasal acantholytic blister o Acantholysis: lysis of intercellular adhesions that connect squamous epithelial cells, cause cells to become rounded Bullous pemphigoid o Subepidermal, nonacantholytic blisters difficult to rupture o Linear deposition of Ig & complement in the BM zone o BPAG1 and BPAG2 that are constituents of hemidesmosomes in which antibodies attack Dermatitis herpetiformis o Urticaria and grouped vesicles, o Celiac disease association: IgA antibodies to gliaden cross react with reticulin Discontinuos granular deposits of IgA on tips of dermal papillae Involve symmetric extensor surfaces noninflammatory Epidermolysis Bullosa: inherited defects in structural proteins Porphyria: inborn errors in porphyrin metabolism, pigments in hemoglobin o Subepidermal vesicle w/ associated marked thickening of walls of superficial dermal vessels Disorders of epidermal appendages acne vulgaris Noninflammatory o open comedones: small follicular papules central black keratin plug (oxidation of melanin) o closed comedones: follicular papules w/o central plug, only seen microscopically Inflammatory: erythematous papules, nodules, pustules Propionibacterium acnes: lipase synthesizing bacteria in upper portion hair follicle o Convert lipids in sebum to proinflammatory fatty acids Androgens may cause Treated with antibiotics and synthetic vitamin A (anti-sebaceous action) rosacea Inappropriate activation of the innate immune system o High levels of antimicrobial peptide cathelicidin (mediator of innate) 4 stages o Flushing (pre-rosacea) o Persistent erythema and telangiectasia o Pustules/papules o rhinophyma Panniculitis Inflammatory rxn in subQ adipose tissue preferentially affecting CT separating lobules of fat or lobules themselves usually in lower legs Erythema nodusum Acute presentation associated with infection by B-hemolytic strep Tender erythematous plaques readily palpated rather than seen Over weeks become flattened and bruise-like Widening of connective tissue septa due to edema, fibrin exudation, neutrophilic infiltration w/o vasculitis Erythema induratum (uncommon) Primary vasculitis deep vessels supplying lobules subsequent necrosis and inflammation of fat Erythematous tender nodule goes on to ulcerate Without underlying cause Shows caseous necrosis of fat lobule & granulomatous inflammation Infection Verrucae (warts): HPV Based on appearance and location Verruca vulgaris: most common type o Frequently on dorsum of hand Molluscum contagiosum: pox virus, self limited umbilicated lesions Spread by direct contact Predilectation for trunk Staining with giemsa reagent shows diagnostic molluscum bodies Impetigo: superficial bacterial infection of skin Contagiosa: group A B-hemolytic strep Bullosa: s. aureus Face and hands honey-colored crust Accumulation of neutrophils beneath stratum corneum o Subcorneal pustule Blister formation: toxin that cleaves desmoglein 1 No dermis involvement: so no scarring Superficial fungal infections: tinea capitis (scalp), barbae (beard), corporis (body surface), cruris (inguinal obese), pedis (athletes foot), onychomycosis (nails), dermatophytes Versicolor: yeast malassezia furfur