Introduction to Toxicology
advertisement
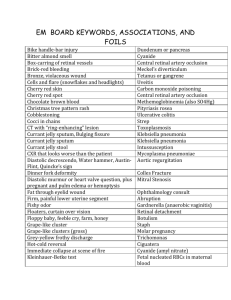
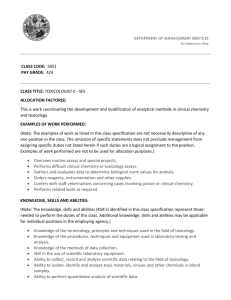
Introduction to Toxicology Medical Toxicology.... Is a board-accredited specialty requiring at least two years of training after residency in either emergency medicine, pediatrics, internal medicine or preventative medicine. Deals with the “diagnosis, management and prevention of poisoning and other adverse health effects due to medications, occupational and environmental toxins, and biological agents” This lecture will condense this information into two parts: • The approach to the poisoned patient Case scenarios • Part I: Approach to the poisoned patient. “Attempts to identify the poison should not delay care.” Initial management of the poisoned patient begins with the ABC’s. ACLS algorithms apply in toxicology with only a few exceptions. Once these are stable, begin considering how to minimize bioavailability. Then you may begin your history and physical. History: find out all of this information: The question words: Which drug(s) were taken? When was it taken? How much was taken? How was it taken? Why was it taken? Was anything else taken? (Consider coingestants: other things which may be in this person’s medicine cabinet.) History continued.... Patients who overdose or use illicit drugs may be unreliable. Gather info from paramedics, family, friends, the PCP, old medical records, pill bottles the patient has on them, their occupational environment or by having people return to the scene where the incident took place. History continued.... Obtain a clinical history from family/friends or paramedics: - patient’s behavior prior to arrival - changing vital signs - seizures Physical Examination: Vital Signs: You MUST obtain a full set of vital signs, including blood glucose. Vital signs are the key to your initial management of the patient.... Vital signs: Pulse Bradycardia (P.A.C.E.D.) Propanolol, poppies Anticholinesterases Clonidine, CCB’s Ethanol Digoxin Tachycardia (F.A.S.T.) Freebase Anticholinergics/ Antihistamines Amphetamines Sympathomimetics Solvents Theophylline Vital signs: Temperature Hypothermia (C.O.O.L.S.) Carbon monoxide Opiates Oral hypoglycemics Liquor Sedatives/Hypnotics Hyperthermia (N.A.S.A.) N.M.S., Nicotine Antihistamines Salicylates Sympathomimetics Anticholinergics Antihistamines Vital signs: Blood pressure Hypotension (C.R.A.S.H.) Clonidine, CCB’s Reserpine Antihypertensives Antidepressants Aminophylline Sedative/Hypnotics Heroin (opiates) Hypertension (C.T.S.C.A.N.) Cocaine Thyroid supplements Sympathomimetics Caffeine Anticholinergics Amphetamines Nicotine Vital signs: Respiration rate Hypoventilation (S.L.O.W.) Sedative/Hypnotics Liquor Opiates Weed (marijuana) Hyperventilation (P.A.N.T.) PCP Pneumonitis Noncardiogenic pulmonary edema Toxic met. acidosis Physical: Neurologic exam Mental status (AEIOU TIPS) Alcohol Endocrine/Epilepsy Intoxication Oxygen Uremia Trauma/Tumor Infection Psychological Shock/Strokes Seizures (OTIS CAMPBELL) Organophosphates Tricyclics INH/Insulin Sympathomimetics Camphor/Cocaine Amphetamines Methylxanthines PCP Benzo withdrawal Ethanol Lead, Lithium Lidocaine, Lindane Physical exam: Pupils Miosis (C.O.P.S.) Cholinergics Clonidine Opiates Organophosphates Pontine bleed Phenothiazines Sedatives/Hypnotics Mydriasis (A.A.A.S) Antihistamines Antidepressants Anticholiergics (Atropine) Sympathomimetics (Cocaine) Physical: Dermatological exam Diaphoresis Red Skin Blue Skin (S.O.A.P.) CO Cyanosis Sympathomimetics Boric Acid MetHb Organophosphates Anticholinergics ASA PCP Blistering Barbituates, CO, Sedative hypnotics, snake/spider bites Odors... Bitter almonds: Mothballs: Garlic: Peanuts: Carrots: Rotten eggs: Wintergreen: Gasoline: Fruity: Pears: Cyanide Camphor Organophosphates, Arsenic Rodenticide Water hemlock Sulfur dioxide, HS Methyl salicylates Hydrocarbons DKA, Isopropanol Chloral hydrate Epidemiology of Toxicology... The majority of poisonings were unintentional.... But, the majority of deaths secondary to poisoning were intentional. Most poisonings are by ingestion and most poisonings occur at home. Epidemiology continued... The most commonly reported poison? Analgesics! The least commonly reported? Alcohol! Which is associated with the most deaths? Analgesics! Which is associated with the least deaths? Hydrocarbons! The number one poisonous killer? Carbon monoxide! Lab tests/Diagnostics... EKG. Why? To look for conduction delays and ischemia. (sympathomimetics, B-blockers, TCA’s, digoxin, CCB’s, CO) CMP. Why? To calculate anion gap and osmolality. (CAT MUD PILES and ME DIE mnemonics) Tylenol and Aspirin levels. Why? Because of the frequency of abuse and co-ingestion. Lab tests/diagnostics continued... Serum volatiles (this tells you quantitative amounts of alcohols). Why? When? With AMS of unknown etiology, for legal purposes, for unexplained osmolar gaps. Drug screens. Why? When? With urine: Screening purposes only. (This rarely changes your management) With blood: For quantitative information regarding specific ingestants. Imaging... Chest XR: (Pulmonary Edema) (M.O.P.S.) Meprobamate Methadone Opiates Phenobarbital Propoxyphene Salicylates KUB: (C.O.I.N.S.) Chloral hydrate Cocaine packets Opiate packets Iron (Heavy metals) Neuroleptics Sustained release/ enteric coated tabs. Management... “Coma cocktail” (Dextrose, Narcan, Thiamine) - Check blood sugars (the sixth vital sign) - Narcan has side effects too! - Thiamine for the malnourished Flumazenil is reserved for people who we overdose with benzos! Management (GI decontamination) Syrup of ipecac: Is not used Gastric lavage: - Used with “moderate to severe overdoses” within an hour of ingestion. -There is a highly variable outcome with this intervention. -Lavage is contraindicated with ingestion of corrosives. GI decontamination continued... Activated charcoal: - Purported to be superior to lavage - Used in toxic ingestions within an hour of the ingestion. - Dosed as 1g/kg or 10:1 ratio of charcoal to poison - Given as single dose or multiple dose Multiple dose Not adsorbed (A.B.C.D.) Antimalarials Aminophylline ASA (?) Barbiturates B-Blockers (?) Carbamazepine Dapsone Dilantin (?) (C.H.A.R.C.O.A.L.) Caustics/Corrosives Heavy metals Alcohols Rapid onset cyanide Chlorine/Iodine Other insolubles (tabs) Aliphatics Laxatives GI decontamination... Cathartics: - Given with charcoal to enhance elimination - Unproven efficacy when used alone. Whole bowel irrigation: - May be effective for things not adsorbed by charcoal - Used for body stuffers/packers Decontamination via enhanced elimination... Hemodialysis: (I.S.T.U.M.B.L.E.) Isopropanol Salicylates Theophylline Uremia Methanol Barbiturates Lithium Ethylene glycol Urine Alkalinization: ASA, Phenobarbital (Alkalinizing the urine with NaHCO3 to trap ions of weakly acidic agents to promote excretion). Titrate NaHCO3 to maintain urinary pH of 7.5-8.0. Management (Antidotes)... Toxin Acetaminophen Anticholinergics Arsenic/Lead B-Blockers Benzos CO Cyanide Digoxin Ethylene glycol/Methanol Iron INH Lead/Mercury Methemoglobinia Opioids Organophosphates TCA’s Antidote N-acetylcysteine Physostigmine BAL chelation Glucagon Flumazenil O2, HBO Nitrites Digibind Fomepizole/Ethanol Deferoxamine B6/Pyridoxine Succimer/DMSA Methylene blue Naloxone Atropine Sodium bicarbonate Pitfalls... Ingestion of multiple agents is common Dangerous drug combinations Drugs masking the effects of other drugs All altered mental status is not tox. Consider trauma (head bleeds) and metabolic causes (DKA, Thyroid, etc) Pearls... Always begin with airway, breathing, circulation. The poisoned patient is not exempt from this mantra. ACLS protocols generally apply to poisoned patients. Treat the patient, not the poison. Observe vital signs and provide supportive care constantly. Part II: Case studies Case 1: Mr. Smith, a 28 year old male presents in police custody complaining of chest pain. He has no other past medical history. No history of cardiac disease. Patient further states that his chest pain began tonight about one to two hours after he was arrested by police. No history of trauma. Social history=Smokes 1 pack/day. Occasional EtOH. Family History= No cardiac deaths. Mr. Smith Physical exam... General: Patient very agitated, clutching his chest. Vitals: P 140, BP 220/130 RR-28 Temp- 103.2F Eyes: Pupils 7mm, equal, EOMI Lungs: Clear Bilaterally Heart: Regular rate and rhythm, 2+/6 systolic murmur Abd: Soft, Non-Tender, BS+ Neuro: No focal deficits. Skin: Diaphoretic Differential diagnosis??? Sympathomimetics (cocaine? amphetamines?) Anticholinergics? Thyroid disease? Solvents? Antihistamines? Undiagnosed hypertension? Acute MI? Malingering? (Why did his symptoms begin an hour after the arrest? Why not immediately? What do you want to order? EKG? (grossly abnormal vital signs) CMP? TSH? UTox? Serum volatiles? Imaging? Cardiac enzymes? EKG: How should this person’s cocaine related chest pain be managed? 1. 2. 3. 4. Benzodiazepines- First line therapy (in high doses) Nitroglycerin- for control of ischemic pain and HTN Labetalol- alpha/beta blocker (the use of propranolol will leave the alpha portion unopposed theoretically exacerbating cocaine's toxicity). Alternatively, phentolamine could be used. Nitroprusside- for refractory HTN This person ingested bags of cocaine. What is the best method of GI decontamination? Ipecac Whole Bowel Irrigation Cathartics Activated Charcoal Dialysis Urine alkalinization Gastric lavage Should other services be involved? If so, whom? Tox! Surgery (Why?) Cardiology (Why?) The outcome.... The patient's chest pain and hypertension eventually resolve with large doses of nitroglycerin and benzodiazepines. The patient is administered activated charcoal and polyethylene glycol solution by the ED physician. Because of the ST segment elevations, the cardiologist elects to give thrombolytics. Since thrombolytics were "on board" the general surgeon refuses to take the patient to the OR for exploratory laparotomy and removal of the cocaine packets. The patient is transferred to the ICU, where he eventually recovers and is discharged with a 10% ejection fraction. Case 2 The patient is a 18 year old male presenting to the ED by paramedics after found at home unresponsive, face down in bed. According to friends, the patient had consumed two beers and a glass of wine earlier that day following a period of depression. The patient was orally intubated in the field by paramedics after no response to D50 and naloxone administration. Physical exam: General: Patient responsive only to deep painful stimuli Vitals: BP 150/70, HR=92, RR=24, T=95.4F Lungs: CTA, BS Equal, (Intubated) CV: RRR, no murmur Abd: Soft, Non-Tender, No Trauma, No Masses Rectal: Normal Tone, HemeNeuro: DTR's Hyporeflexive, Withdraws to Painful Stimuli Differential diagnosis?? Alcohol intoxication? Carbon monoxide? Sedatives/Hypnotics? (benzos? barbiturates? muscle relaxants?) Tylenol? Trauma? Large doses of narcotics? What do you want to order? CBC? CMP? Serum osmolality? Serum volatiles? Urine toxicology screen for drugs of abuse? EKG? Results: CBC: WBC 29K HCT=45 Lytes: Na=145 Cl=105 K=5.2 HCO3=5 BUN/Cr: 28/1.8 Glucose 180 Osm: 370 (Measured) ETOH: 46 Calcium 7.0 Toxicology Screen: Pending Toxic Alcohols: Pending What is his anion gap? What is his osmolar gap? AG: 20. Osmolar gap: 370 – (2(Na) + Glu/18 +BUN/2.8 +ETOH/4.6) = 50! (50 is greater than 10, so..... ) Results continued... EKG shows NSR. No interval changes. No ST, T or Q wave changes. Normal axis. Normal R wave progression CXR: Shows normal sized heart and mediastinum. No effusions or infiltrates. No acute disease. ETT in proper position. How do you want to manage this patient? Supportive care only Gastric lavage Hemodialysis Is there a potential antidote for this? YES! Fomepizole! We don’t have any fomepizole. But we do have ethanol! Outcome... With a strong clinical suspicion for toxic alcohol ingestion, an ethanol drip is ordered, but due to pharmacy delay, the patient is orally loaded with 85 proof whiskey obtained from another patient in the ER waiting room. Urine is positive for calcium oxalate crystals. Dialysis is initiated by the renal service, after which an ethylene glycol level of 310 mg/dl returns 12 hours later. The patient recovers with mild renal insufficiency, and is subsequently followed-up by the psychiatric service for his depression. References... 1. Erickson TB et al. Toxicology Update: A Rational Approach to Managing the Poisoned Patient. Emerg Med Pract. 2001; 3(8): 1-28 2. Tuckler, Victor. Introduction to Toxicology handout 3. Rivers, Carol S. Preparing for the Written Board Exam in Emergency Medicine. 5th Ed. Volume II. PP 735-738 4. “Case studies in Toxicology” available at: http://www.uic.edu/com/er/toxikon/cases/allcase.htm 5. http://www.med.umich.edu/lrc/baliga/case02/images/infMI2. jpg