laburine.PRE
advertisement

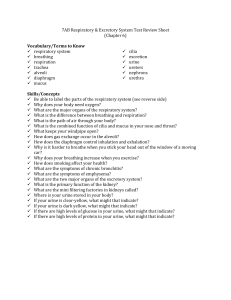
Lab Medicine Conference : Urinalysis Jim Holliman, M.D., F.A.C.E.P. Professor of Surgery and Emergency Medicine Director, Center for International Emergency Medicine M. S. Hershey Medical Center Penn State University Hershey, Pennsylvania, U.S.A. Indications for Urinalysis ƒ Suspect / confirm UTI ƒ R/O primary renal disease ƒ R/O systemic disease with major renal manifestation ƒ Assess complications of hypertension ƒ Assess presence or amount of endogenous or exogenous excreted substances Complete Urinalysis : Components ƒ Color / appearance ƒ Specific gravity ƒ pH ƒ Chemistries –protein –glucose –ketones –bilirubin / urobilinogen –hemoglobin / blood –nitrite –leucocyte esterase ƒ Microscopic exam –cells / casts –bacteria –other organisms –crystals Secondary, Optional Tests on Urine ƒ ƒ ƒ ƒ ƒ ƒ ƒ Culture Quantitative culture Sensitivity Gram stain Acid-fast stain Protein electrophoresis Antigen detection (immunofluorescence) ƒ Quantitative assays What is Urine, Anyway ? ƒ 95 % water, 5 % solids ƒ 3 main components : –water –urea –NaCl ƒ Color from pigments urochrome & urobilin ƒ Intensity of color parallels degree of contamination Urinalysis : Important Aspects of Collection ƒ "Clean - voided" specimen necessary if micro exam to be done –Cleansing of urethral meatus –Preinsert tampon if discharge present –Hold labia minora apart –Midstream specimen ƒ "Mini-cath" is option to reliably avoid menstrual or vaginal discharge contamination ƒ Adhesive perineal bag vs. direct bladder puncture with 22 g. needle are collection options for peds patients (or try "Perez reflex") “Minicath” urine collection tube Problems with Delayed Analysis of Unrefrigerated Urine ƒ Bacteria split urea to ammonia, & urine becomes alkaline ƒ Casts decompose ƒ Red cells lyse ƒ Bacterial counts increase ƒ Glucose decreases Diagnostic Clues from Urine Odor ƒ Volatile acids responsible for normal urine odor ƒ Specific odors & dx's : –Acetone : DKA –Ammonia : infection with urea breakdown –Maple Syrup Urine Disease –Asparagus or garlic ingestion Causes of Increased Turbidity of Urine ƒ ƒ ƒ ƒ ƒ ƒ ƒ Urate crystals in acid urine Phosphates in alkaline urine RBC's WBC's Bacteria Vaginal secretions Fat globules Differential diagnosis of red-orange urine color Differential diagnosis of red or pink urine color Differential diagnosis of purple urine color Differential diagnosis of red-brown urine color Differential diagnosis of brown-black urine color Differential diagnosis of yellow-brown urine color Differential diagnosis of yellow urine color Differential diagnosis of yellow-orange urine color Differential diagnosis of colorless urine Differential diagnosis of milky-colored urine Parasitic chyluria due to Wucheria bancrofti or other filaria ; can cause thoracic duct fistulas to the kidney or bladder Differential diagnosis of blue-green urine color Differential diagnosis of brown-green urine color Differential diagnosis of yellow-green urine color Interpretation of Specific Gravity in U/A's ƒ S.G. is the ratio of urine density compared to a water standard ƒ S.G. indirectly measures renal concentrating ability ƒ Is measured by dipstick or refractometer ƒ S.G. values : –Distilled water : 1.000 –Dilute urine : 1.001 to 1.010 –Concentrated urine : 1.025 to 1.030 ƒ Correlation with osmolarity : –S.G. 1.010 = osmolarity 285 (same as serum) –S.G. 1.025 = osmolarity > 600 Causes of Falsely High S.G. Readings ƒ Excretion of radiopaque contrast media ƒ Excessive proteinuria (as in nephrosis or diabetes) ƒ Excessive glycosuria ƒ Refrigerated urine Diagnostic Clues from Urine pH ƒ Range 4.6 to 8 ; normal about 6 ƒ Animal protein diet : acid urine ƒ Vegetable / fruit diet : alkaline urine ƒ Stones that develop in alkaline urine : –Calcium phosphate –Calcium carbonate –Mg PO4 ƒ Stones that develop in acid urine : –Uric acid –Cysteine –Calcium oxalate Protein Analysis in U/A's ƒ Normal urine contains small amounts of albumin & globulin ƒ Proteinuria exists if > 20 mg/dl –Incidence 6 to 9 % in asymptomatic patients ƒ Dipstick tests use tetrabromophenol blue indicator system (yellow to green as conc. increases) –React mainly with albumin –False positive with quaternary ammonia compounds & phenazopyridine dyes Clinitest Use for Detection of Glycosuria ƒ Based on reduction of metal ions by glucose ƒ False positive reactions due to : –Hypochlorite or chlorine –Other sugars (galactose, lactose, fructose, maltose, as during pregnancy) ƒ Enzyme - based tests (glucose oxidase) are more specific for glucose ƒ Can have false negative results with ascorbic acid, tetracycline, or high uric acid Correlation of Urine Glucose Readings Reading mg/deciliter Glucose Negative 0 Trace 100 1+ 250 2+ 1000 3+ 2000 4+ >2000 Analysis for Ketones in U/A's ƒ Choices are : –Acetest (tablet) –Test tube (Rothera) –Dipstick ƒ All use reaction between acetoacetic acid & nitroprusside to make a violet dye complex ƒ Acetone reaction is < 5 % of color change ƒ Beta-hydroxybutyrate not detected Causes of False Positive Urine Ketones ƒ ƒ ƒ ƒ ƒ ƒ Levodopa Phenolphthalein (in laxatives) Insulin Pyridium (phenazopyridine) Phenformin Phenylketonuria Analysis of Bilirubin in U/A's ƒ Conjugated bilirubin in normal urine up to 0.002 mg/dl ƒ Dipstick uses diazonium salt reagent (buff to pink to brown) ƒ Positive test for urinary bilirubin with a negative urine urobilinogen indicates biliary obstruction ƒ Phenazopyridine causes false positive ƒ False negatives : –Chlorpromazine, selenium –Exposure to light (inactivates to biliverdin) Analysis of Urobilinogen in U/A's ƒ Is colorless ƒ Produced as byproduct of bacterial degradation of conjugated bilirubin ; enterohepatic circulation accounts for normal urinary excretion ƒ Is increased with hemolysis or liver disease, & decreased with biliary obstruction ƒ Phenazopyridine causes false positive ƒ High nitrates cause false negative (as in red wines) Analysis of Hemoglobin in U/A's ƒ Not detectable by naked eye unless > 1:1000 blood in urine ƒ Uses peroxidase characteristic of hemoglobin or myoglobin to change color of chromogen ƒ Dipsticks detect both free Hgb & myoglobin, and intact RBC's ƒ False positives from bromides, copper, iodides, oxidizing agents ƒ False negative from ascorbic acid Analysis of Nitrites in U/A's ƒ Nitrites absent from normal urine ƒ Most UTI bacteria reduce urinary nitrates to nitrites using enzyme nitrate reductase ƒ Dipstick uses aromatic amine & diazonium compound to produce pink color in presence of nitrite ƒ False positive rare ( can be due to phenazopyridine) ƒ False negatives : –Bacterial inhibition with antibiotics –High urine flow (dilutional) ; Frequent or continuous (foley) voiding –Ascorbic acid Analysis of Leucocyte Esterase in U/A's ƒ Any purple color on dipstick indicates > 5 WBC's/hpf ƒ Detects intact & lysed WBC's & WBC casts ƒ False negatives : –Cephalexin, gentamicin, nitrofurantoin ƒ Up to 97 % sensitivity & 90 % specificity for culture - proven UTI's Use of "Reflex Urinalysis" at Hershey Medical Center ƒ "Reflex U/A" = dipstick (Chem 9) –Micro exam done at no extra charge if dip is positive for protein, Hgb, or leucocyte esterase ƒ Is indicated for routine U/A's as part of routine physical exam, and in other patients without possible urologic sx Costs for U/A's at Hershey Medical Center ƒ $17.00 for inpatients ƒ $12.00 for outpatients ƒ If microscopic U/A ordered separately : –Add $15.00 for inpatients –Add $13.00 for outpatients ƒ Urine culture is $32.00 ƒ Urine C&S is $79.00 Rationale for Use of Dipstick as Screening for Micro Exam of Urine ƒ 5 combined studies : 3205 patients –Sensitivity : 94 % –Specificity : 72 % ƒ HMC study : 50 patients –Sensitivity : 93 % –Specificity : 72 % ƒ Post - test probability of abnormal urine sediment if reflex U/A is negative is 1 to 6 % Analysis of WBC's in Urine ƒ Normal WBC excretion in urine : –Up to 400,000 cells per hour –Averages 650,000 per day –10 WBC per ml. correlates with 1 WBC per hpf ƒ Counts exceeding 10 WBC per ml. correlate with significant bactiuria in 40 to 84 % ƒ Can have false negative if patient is leucopenic White blood cells in urine Causes of Sterile Pyuria ƒ ƒ ƒ ƒ ƒ ƒ ƒ ƒ Balanitis or urethritis Bladder tumors Calculi Exercise Fever Glomerulonephritis Renal tuberculosis Viral infections Analysis of RBC's in Urine ƒ Normal RBC excretion in urine : –Up to 1,000,000 per day –Average 130,000 per day –So average is 1 RBC per 2 to 3 hpf or 500 to 1000 RBC per ml. ƒ Hematuria then represents greater amounts of blood than these ƒ For urine to be considered free of blood, both supernatant & sediment should be dipstick tested Red blood cells in urine Gross hematuria from congenital urethral stricture Analysis for Bacteria in U/A's ƒ Bacteria are absent in normal bladder urine ƒ Micturition commonly deposits bacteria in urine ƒ Classic infection definition : > 100,000 organisms per ml. of freshly centrifuged, freshly voided urine ƒ Correlations with infection : –Detection of any bacteria on uncentrifuged specimen – > 10 bacteria / hpf of centrifuged sample Bacterial urethritis (should be treated with topical and oral anti-Staph antibiotics) Bacterial Counts in Urine ƒ < 1000 colonies per ml. implies only contamination ƒ Counts > 1000 and < 100,000 per ml. may imply infection ƒ Counts > 100,000 / ml. almost always imply infection ƒ Causes of false low counts : –pH < 5, S.G. < 1.003, voiding < 45 minutes from sample collection, urethral obstruction, infections with fastidious organisms, contaminants with string oxidants (bleach) Diagnostic Significance of Cellular Casts ƒ Represents contents of renal tubules discharged into urine ƒ Cast width descriptions : –Narrow : 1 to 2 RBC's in width –Medium : 3 to 4 RBC's in width –Broad : > 5 RBC's in width ; these are formed in the collecting tubules & suggest severe renal disease ƒ Cast types & associated diseases : –Broad, epithelial, fatty, granular, or waxy : parenchymal renal disease –RBC : acute glomerulonephritis –WBC : pyelonephritis Diagnostic Aspects of Cellular Casts ƒ RBC casts –Usually represent significant glomerular disease –Can occur after very strenuous exercise –Alkaline urine hemolyzes RBC's & can dissolve casts if analysis delayed ƒ Hyaline casts –Clear, colorless ; due to protein precipitation –Occurence depends on urine flow, pH, degree of proteinuria ƒ Granular casts –Result from disintegration of cell material into particles –Form waxy casts when renal failure is advanced Hyaline casts from protein gel in the renal tubule ; normal sediment has one to two per high power field Granular casts Red blood cell casts White blood cell cast Red cell casts in acute glomerulonephritis Waxy granular and cellular casts in chronic glomerulonephritis Hyaline cast with epithelial cells in tubulo-interstitial disease Analysis for Crystals in U/A's ƒ Crystals commonly found in normal urine ƒ Pathologic crystals : –Cysteine (hexagonal ; not birefingent under polarized light, unlike uric acid) –Leucine (yellow spheres with striations) –Tyrosine (fine needles in rosettes) ƒ Phosphate & urate crystals of little Dx significance ƒ Calcium oxalate crystals sometimes indicate ethylene glycol poisoning (but can be normal) Crystals found chiefly in alkaline urine Sulfonamide crystals Crystals found chiefly in acid urine Ammonio-magnesium-phosphate (struvite) crystal due to chronic U.T.I. with Proteus (alkaline urine) Uric acid crystals under bright field microscopy Uric acid crystals under polarized light Tyrosine crystals under bright field microscopy Leucine crystals under bright field microscopy Cystine crystals under bright field microscopy Uric acid crystals in a 3 month old patient evaluated for orange diaper stains ; this situation calls for evaluation of renal function tests Miscellaneous Agents Detectable on U/A Micro Exam ƒ ƒ ƒ ƒ Spermatozoa Trichomonads Candida albicans Rarely Giardia or Entamoeba histolytica ƒ Other parasites –Schistosoma –Nematodes Trichomonas vaginalis in urine Candida albicans in urine Measurements of Electrolytes in Urine ƒ Ion specific electrodes currently used (same as for serum) ƒ Clinical situations where measurements useful : –Sodium ƒ Volume depletion, acute oliguria, hyponatremia (R/O SIADH) –Chloride ƒ Determine if metabolic alkalosis is chloride resistant or sensitive –Potassium ƒ Determine site of K+ loss in hypokalemia (if < 10 meq/liter, implies GI tract as source) Interpretation of Urinary Chloride Levels in Metabolic Alkalosis ƒ Urinary chloride 0 to 10 meq/liter ("chloride-responsive") : –Vomiting –NG suction –Diuretic effect –Post-hypercapnia ƒ Urinary chloride > 10 meq/liter (approx. dietary intake) : –Severe hypokalemia –Renal failure –Edematous states –Mineralocorticoid excess –Licorice ingestion Suggested Criteria for Obtaining Urine Cultures if UTI Suspected ƒ All children (age < 14) ƒ All males ƒ Women with history of : –Immunocompromise –Renal abnormalities –Diabetes mellitus –Recent instrumentation –Indwelling catheter –Prolonged Sx before seeking care –3 or more ( ? > 5 ) UTI's in last year –Recent pyelonephritis –Recent hospitalization Lab Medicine Conference : Urinalysis Summary ƒ Assess urine color & overall appearance ƒ Decide if only dipstick analysis needed ƒ Consider explanations for each abnormal component on dipstick & micro ƒ Decide if additional studies (C & S, electrolytes, osmolality, etc.) needed