Payment Schedule Working with the people of Camden to achieve
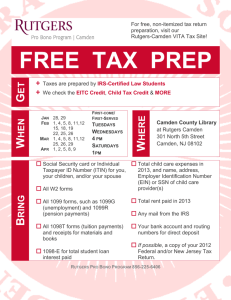
advertisement
Frail and Elderly Complex Care Case Management Locally Commissioned Service (LCS) Dr Lance Saker CCG Governing Body member and Clinical Lead Role of the LCS within the FE Programme • Supports improved identification of frail patients with complex needs. • Improves the co-ordination of care for those patients. • Supports delivery of an integrated model of care. • Supports a reduction in use of unscheduled health and social care • Is the underpinning of the whole FE programme. Role of General Practice in the FE Programme 1. Identification and Assessment • • • • Regularly review patients on lists. Enter suitably frail patients onto the frailty register. Record a full frailty assessment Record a comprehensive care plan. • Use the designated Camden EMIS templates. 2. Case management of patients on register • Decide on level of need – in practice or hub? • In practice – MDT case management in place. • Hub – refer on and ensure delivery of actions arising. Working with the people of Camden to achieve the best health for all Role of General Practice in the FE Programme 3. Practice Based MDT Meetings • Must include patient’s case manager, GP and community team rep. • Meet at least quarterly. • Patients can be stepped down from case management if risk of unscheduled need reduces. 4. Training and education All clinicians at the practice to undertake a learning module. One member for peer education at MDT Hub every 6 months. Practices to undertake adult safeguarding training. Working with the people of Camden to achieve the best health for all The CCCM LCS Process Map Revisions to original LES A Complex Care Management LES was in place 13/14. Was accompanied by a Risk Stratification ES. New LCS incentives practices to do a detailed assessment of need, to further increase referrals to the MDT Hub. Removed the requirement to undertake audits. Payment for case management is being replaced by proactive home visiting and in-practice consultation. Working with the people of Camden to achieve the best health for all Payment Schedule Component Payment Comment All fields marked “LCS” on the relevant template must be completed to incur payment Assessment undertaken and care plan completed on template with evidence of £75 per patient MDT input MDT team meetings to discuss cases To qualify, the practice must have £100 per practice, per month at least 10 patients on their FR (max. 12/year) 6 monthly attendance at Hub MDT peer review education sessions £150 per attendance practice Only one person per practice will per be paid to attend but as many as wish to may attend Working with the people of Camden to achieve the best health for all Impact of the LCS Variation by practice Variation in care plans Further impact Potential Frailty Gap Future Developments • Federated GP Practices • Proposed development of an FE Integrated Practice Unit • Taking forward the ‘Vanguard’ possibilities Working with the people of Camden to achieve the best health for all The Future circa 2017/18? Diagnostics Key in year changes • Integration with acute • Commission GP front end front end hub GP Front End (Hub) 8am-8pmcommission Specialist services Link to GP Core GP service GP Federation Admin Hub OOH/111 Elective GP (Spoke) 8am-8pm Camden Community Service (CCS) Unscheduled Care 8am-10pm • Minor injury Outreach to home MDT working Chronic Disease Management • Community LTC Hub • Diagnostics • Ambulatory Care • Link to GP OOH/111 • Specialist clinicians Chronic Disease Management Community Services • Advice and Guidance • Cross-cutting • services • Community and Social Care teams • Rehabilitation • Link to community beds • Rapid Response teams A&E • Outreach to local population • In-reach to hospital Nonelective Secondary care Continuous focus on prevention Underpinned by: Workforce development via partnership work across providers Shared / interoperable records system (CIDR)