Adelsheim
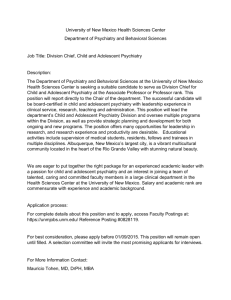
advertisement

THE SCHOOL MENTAL HEALTH IMPERATIVE Steven Adelsheim, M.D. University of New Mexico Department of Psychiatry NM Department of Health, OSH Jenni Jennings Dallas Independent School District THE SCHOOL MENTAL HEALTH IMPERATIVE Steven Adelsheim, M.D. University of New Mexico Department of Psychiatry NM Department of Health, OSH Mark D. Weist, Ph.D. University of Maryland Department of Psychiatry Prevalence of Childhood Mental Health Problems About 20% of children and adolescents (15 million), ages 9 to 17, have diagnosable mental health disorders Between 9-13% of children, ages 9-17 years, meet the definition of serious emotional disturbance (SED) that limits their ability to function in the family, school, and community An estimated 70% of those identified are not getting the mental health treatment they need Surgeon General’s Conference on Children’s Mental Health By 2020, childhood neuropsychiatric disorders will rise by over 50% internationally to become one of the 5 most common causes of morbidity, mortality, disability Global Burden of Disease study predicts that major depression will become the second leading cause of disability in the world by the year 2010 “There is no mental health equivalent to the federal government’s commitment to childhood immunization” Surgeon General’s Suicide Data 1997 Rate for ages * 10-14 - 1.6 /100,000 * 15-19 - 9.7 /100,000 * 20-24 - 14.5 /100,000 For young people 15-24, suicide is third leading cause of death In 1996, more youth and young adults died from suicide than cancer, heart disease, AIDS, stroke, pneumonia, & birth defects COMBINED 2001 New Mexico YRRS 13.7% of students had attempted suicide in the 12 months prior to the survey 15.5% 7.1% Up of females of males from 9.1% in 1999 An Attitudinal Shift Towards Children’s Mental Health Programs Public Health perspective similar to that for immunizations, sexually transmitted diseases Put children’s services on equal financial footing as adult programs if we really believe in prevention and early identification Equal focus for children’s services at federal, state, and local systems University training systems prioritize children services Prevalence of Mental Health Problems Post 9/11 64% of students had been exposed to one or more traumatic events BEFORE 9/11 10.5% of students were estimated to have PTSD (75,000) Previous exposure to traumatic event or exposure of a family member or were more important than personal physical exposure in predicting who developed PTSD 26.5% have at least one of the seven assessed mental health problems, excluding alcohol abuse (190,000 students) At least 66% of students with probable PTSD following the 9/11 attacks had not sought out ANY mental health services! Early Identification and Treatment of Psychiatric Disorders as Prevention ADHD – Pharmacotherapy reduces risk for later substance use disorder (Biederman, et al, 1999) Bipolar disorders – early identification of BAD in younger children reduces risk of ASUD 8X over adolescent identification (Wilens et al, 1999) Opposition Defiant/Conduct Disorders – early treatment of child, parent, family all decrease later ASUD risk (Riggs) NYC Mental Health System Recommendations All interventions should be school-based to increase access and decrease stigma Outreach and training in schools to identify youth with mental health problems Screening and assessment system within schools. that includes a seamless link to services Evidence–based models of intervention Increase school-based clinics throughout NYC schools Schools: The Most Universal Natural Setting Over 52 million youth attend 114,000 schools Over 6 million adults work in schools Combining students and staff, one-fifth of the U.S. population can be found in schools Why Put Mental Health Services in Schools? Improve access: It’s where the students are! Families more comfortable in community setting Minimize stigma issues Opportunities to observe and intervene directly in setting where most student’s time is spent Clinical efficiency and productivity Ability to collaborate and advocate directly for education needs of students Greater ability to reach those with “internalizing disorders” Major Approaches to Mental Health in Schools School-Based Health Centers (1,400) Community Mental Health Center Outreach (114,000 schools) Private Practitioner Outreach Communities in Schools Enabling Framework (Adelman and Taylor) Other Education-Based, Including Special Education Linked and Consultation School Mental Health Partnerships with Families Opportunities to collaborate with providers onsite about education needs of child Improved coordination of interventions around whole child and family Access is easier with fewer transportation issues More comfortable community setting Stigma issues may be minimized School-Community Collaboration in School Mental Health Programs Collaboration and coordination between school and providers is critical Roles of all on-site providers, including school health professionals must be clear Communication and confidentiality issues must be directed addressed and established Resource coordination efforts must be determined by organized team within school (SAT, resource team, etc.) School Mental Health Programs and Special Education Currently most school mental health professionals work only with special education students SBHCs may have a critical role to play in evaluation, recommendations, interventions, IEPs for special education School mental health providers may find students in need of further educational assessment and be on site to advocate for their needs On-site school mental health professionals are a resource for administrators struggling with difficult discipline issues School mental heath providers may give direct guidance to teachers in meeting student classroom needs School Mental Health Program Outcomes Improved grades, attendance, and behavior in students Decreased inappropriate referrals to special education Improved school climate Funding a Continuum of School Mental Health Programs and Services State and local grants and contracts Federal and foundation grants and contracts Innovative prevention funding Medicaid: fee-for-service, Medicaid managed care, Medicaid in the Schools Allocations from schools, special education services, and departments of education Continuum of Care for School Mental Health Programs Awareness and training Three levels of prevention, including universal, selective and indicated Screening and assessment Early identification and early intervention Three levels of treatment, including community-based, transitional, and high-end NM DOH Office of School Health Director Laurie A. Mueller HPM-1/Santa Fe School Health Officer Jane McGrath (UNM)/Abq School-Based Health Center Consultant Mary Blea Nurse-5/Abq SBHC Nurse Practitioner Medicaid Consultant Paula LeSueur (UNM)/Abq School Health Advocates Deb Werner - Dist I Janie Lee Hall - Dist I Trudy Perry - Dist II Laura Mandabach - Dist III Janice Jordan - Dist IV Administrative Assistant II Carol Montoya (UNM)/Abq Medical Care Administrator Vacant PH Educ./Santa Fe Healthier Schools Consultant Randy Sanches PH Educ./Santa Fe Planner Vacant Santa Fe Secretary Pamela Hedrick Santa Fe Dropout Prevention Coordinator Nissa Patterson (UNM)/Albq School Mental Health Advocates Vacant - UNM / Dist I Jaynee Fontecchio - UNM /Dist I NW Joseph Vigil - UNM / Dist II Albert Sanchez - UNM / Dist III Steven Courts - UNM / Dist IV School Mental Health Initiative, Director Steve Adelsheim (UNM)/Abq Program Manager Kris Carrillo (UNM)/Abq Behavioral Education Consultant Vacant PH Educ./Abq School-Based Mental Health Services Consultant Jacque Masog (UNM)/Abq Screening / Early Identification Consultant Ernest Coletta (UNM)/Albq Administrative Asst. III Clancey Tarbox (UNM)/Abq Office of School Health Locations District IV District III New Mexico School Behavioral Health Partnership Office of School Health Behavioral Health Division CYFD-Prev. & Interv. Dept of Ed.-Spec.Ed. Dept. of Ed.-School Health Fed. M H Block Grant HSD-Med. Asst. Div. $300,000 $400,000 $320,000 $170,000 $350,000 $140,000 Interdepartmental School Behavioral Health Partnership Funded Programs School Behavioral Health Training Institute Youth Mental Health Awareness Initiative“Childhood Revealed” Dropout Prevention Project School Behavioral Health Screening Program School-Based Mental Health Center Program Development SBHC Mental Health Exemplary Pilot Sites School Mental Health System Recommendations Through schools, train educators, students, and families about children's mental health issues and their impact on education Continue to fund evidence-based prevention programs, including indicated prevention activities Expand incentives to increase the numbers of child-trained MH providers and require a school-based component to their training School Mental Health System Recommendations-continued Implement screening and assessment for behavioral health issues: Head Start Child Find and IDEA EPSDT Entrance to schools with vision and hearing At critical junctures in school such as at transition grades and at point of disciplinary action School Mental Health System Recommendations-continued Create specific funding for school-based mental health services in school-based health centers and as a part of federally funded mental health and education programs Examples: SCHIPS Medicaid Medicaid in the Schools “No Child Left Behind”-Safe and Drug Free Schools, Title 1 and other entitlements School Mental Health System Recommendations-continued Support state level infrastructure for mental health service system delivery between mental health and education systems Fund school mental health demonstration sites and disseminate the most effective models Create Office of School Health/Mental Health at federal level (joint Health and Ed.), pool funds from multiple agencies and distribute to schoolcommunity collaboratives Integrate school-based mental health and primary care services Find Children and Adolescents with Behavioral Health Problems Early and Treat Them Prevent later special education referrals Reduce primary care and urgent care over utilization Decrease high risk behaviors including violence and substance abuse Improve educational outcomes Decrease the accidents, suicides, and homicides that are the public health mortalities for our children The National Child Psychiatrist Shortage In 1990, COGME reported a national need for 30,000 child psychiatrists by 2000 Currently there are 6,300 A minimum projected need for 12,624 to meet demand by 2020 with a predicted 30% increase in numbers to 8,312 New Mexico School Behavioral Health Training Institute Train-the–Trainers model of adult education Training 180 teachers and school health professionals from 14 districts this year Training in aspects of school behavioral health and classroom intervention On-site workshops with staff support Childhood Revealed New Mexico 2001 Art exhibit as centerpiece for youth mental health awareness expansion statewide Linkages to school districts for in-service training and classroom programs (0ver 5000 youth so far this year) Community education programs for expanded awareness Media, government, and business support all to help to decrease stigma New Mexico School Mental Health Prevention Programs Dropout Prevention Program Peer Navigator’s Program Crisis Prevention and Intervention Coordination Prevention Programs Resource New Mexico Dropout Prevention Initiative Case management model for high risk youth and their families Focus on wraparound supports for those identified of being at risk to dropout Statewide training and RFP development 2002 fiscal year Focus on implementation at 3 pilot sites statewide for fiscal years 2003-4 Target 9th grade students making transition to high school New Mexico K-6th Behavioral Health Assessment Training for teachers and school health professionals statewide in behavioral health issues Website development as training and resource model-www.nmsmhi.org Developing of screening and assessment tools for K-6th grade use statewide Focus on student support team system development for schools Funded by state legislature through SDE New Mexico Screening and Early Identification Models Early identification and intervention as prevention Public health screenings vs. selective screenings in SBHCs Piloting computer-based models for early identification and suicide prevention Expanded interest by schools to utilize screening tools on larger scale New Mexico School-Based Health Center Mental Health Program Development Expanded funding for mental health and substance abuse services 17 SBHC programs One cluster wide Medicaid Managed Care School Behavioral Health Pilot Program Standards and protocols for MH/SA services in schools Four “Exemplary” School Mental Health Sites looking at mental health and educational outcomes New Mexico Medicaid Managed Care SBHC Pilot Projects Pilot with Center for Health Care Strategies Reimbursement through Medicaid for mental health and substance abuse services 5 Medicaid Managed Care SBHC pilots Developing depression, ADHD and substance abuse protocols for MH/SA services in schools “Enhanced Mental Health Services” code for some sites New Mexico School Mental Health Initiative Statewide efforts to link families, communities, schools and behavioral health programs Phone: 505-841-5879 Fax: 505-841-5885 Email: stevea@doh.state.nm.us Website: http://www.nmsmhi.org University of Maryland Center for School Mental Health Assistance Provide technical assistance and consultation Provide national training and education Disseminate and develop knowledge Promote communication and networking phone: email: web: 410-706-0980 (888-706-0980 toll free) csmha@psych.umaryland.edu http://csmha.umaryland.edu UCLA Center for Mental Health in Schools Directed by Howard Adelman and Linda Taylor Phone: 310-825-3634 Enews: listserv@listserv.ucla.edu web: http://smhp.psych.ucla.edu