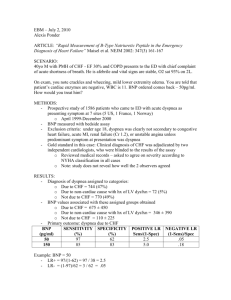
Heart failure
advertisement
Hypertension Complications of Hypertension • • • • • • Hypertensive Cardiovascular Disease Hypertensive cerebrovascular disease Hypertensive Renal Disease Aortic Dissection Atherosclerosis Vision Changes Collaborative Management of Hypertension • Pharmacologic – – – – Diuretics ACE Inhibitors/Angiotensin Receptor Blockers (ARBs) Calcium channel blockers Nitrates • Non-Pharmacologic – – – – – Stress reduction Weight control Decrease alcohol intake Beware of OTC drugs Stop Smoking DASH Diet Hypertensive Emergencies • High B/P • Urgencies • Emergencies Nursing Diagnoses • Knowledge Deficit • Impaired Health Maintenance Nursing Interventions: (NIC) • • • • • • • • • Anticipatory guidance Behavior Modification Calming Techniques Coping Enhancement Electrolyte Management and Monitoring Exercise Promotion Nutrition Counseling Teaching: Disease Process Teaching: Medications Nursing Outcomes (NOC • Health seeking behavior • Knowledge of diet, disease process, medications…. etc. • Adherence (compliance) behavior Heart Failure Review • The basic function of the renin-angiotensin-aldosterone system • Use of the following in HTN/HF: – ACE/ARB – CCB – Beta Blockers • Diagnostic criteria for Hypertension (JNCC 7) http://hin.nhlbi.nih.gov/nhbpep_slds/jnc/jncp2_1.htm • Incidence, prevalence, epidemiology of hypertension, heart failure • Clinical presentation of right and left sided heart failure. • Function of ANP/BNP • Vascular assessment findings r/t arterial and venous insufficiency. Learn: • Definition and defining characteristics of – Ineffective Health Maintenance r/t deficient knowledge regarding treatment and control of disease process – Decreased cardiac output r/t impaired cardiac function – Ineffective Tissue Perfusion • Definition and indicators for these NOCs: – Health Promoting Behavior – Tissue integrity: Skin and Mucous Membranes – Hemodynamic regulation • Review these NICs: – Circulatory Care: Arterial Insufficiency – Circulatory Care: Venous Insufficiency • Cardiac resynchronization therapy Objectives: • Plan, implement and evaluate care for patients with acute and chronic heart failure. • Plan, implement and evaluate care for patients with hypertension, and patients experiencing hypertensive emergencies. • Describe nursing strategies for promoting adherence with medication therapy for HTN, HF • Describe health promotion strategies for patients at risk for HTN. Fact: CHF Incidence=550,000 cases/year (AHA,2005) Prevalence= 5 million living with HF (AHA, 2005). CHF office/hospital visits = 12 -15 million office visits per year. -6.5 million hospital days/year (AHA, 2005). Hospital discharges= $5,471 per discharge -377,000 (1999) /yr 970,000 (2002) /yr, a 157% increase (AHA,2005). Cost/year/Hospital admissions = 27.8 billion in 2000 (CMS 2003, AHA 2005) Cost/year/managing CHF= $56 billion,70% due to hospitalization (Bhalla, 2004) Summary: (AHA,2005) Percent of Population 14 11.6 12 12.4 10 7.2 8 5.2 6 4 2 2 0.3 1.5 0.2 0 20-39 40-59 Men 60-79 Women Prevalence of heart failure by age and sex (NHANES: 1999-2004). Source: NCHS and NHLBI. 80+ Discharges in Thousands 700 600 Male 500 Female 400 300 200 100 0 79 80 85 90 95 00 Years Hospital discharges for heart failure by sex (United States: 1979-2004). Source: NHDS, NCHS and NHLBI. Note: Hospital discharges include people discharged alive, dead and status unknown.. 04 Per 1,000 Person Years 50 40 43.0 Men 30 30.7 22.3 20 10 Women 14.8 9.2 4.7 0 65-74 75-84 85-94 Age Incidence of Heart Failure* by age and sex. (FHS: 1980-2003). Source: NHLBI. * HF based on physicians review of medical records and strict diagnostic criteria. Review Blood Circulation What is heart failure? • The American College of Cardiology/American Heart Association (ACC/AHA) (2005) provides a scientific statement defining heart failure as “A complex clinical syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood. The cardinal manifestations of HF are dyspnea and fatigue, which may limit exercise tolerance, and fluid retention, which may lead to pulmonary congestion and peripheral edema (p. e160).” • Heart failure usually occurs when another problem makes the heart weak or stiff so it doesn’t pump or fill normally. Natural History of Heart Failure Diabetes Obesity Diabetes HTN Diabetic Cardiomyopathy LVH CHF Smoking Lipids Normal LV structure and function Diastolic dysfunction MI LV remodeling Systolic dysfunction Subclinical LV dysfunction Overt heart failure Vasan RS, Levy D. Arch Intern Med. 1996;156:1789–1796. HF…… ……..complex progression of domino effects involving cardiac and neurohormonal systems…….. Compensatory Mechanisms • Sympathetic Nervous System Stimulation • RAAS • Neurohormonal responses TNF / Interlukins 1 and 6 BNP Endothelin [1] Sympathetic Nervous System Stimulation • Normal adaptive mechanism: – As a response to decreased CO, the body attempts to compensate: – increased release of catecholamines • Undersirable effects of catecholamine release: – Afterload is increased, increasing cardiac work load – SV Inc----Starling’s Law---– Arterial vasoconstriction----leading to---Inc afterload—LV requiring more energy to eject----SV declines [2] Neurohormonal Responses [1] After MI release of proinflammatory cytokines (TNF) and interleukins (IL 1 & IL 6) , leading to ventricular remodeling. [2] BNP release promote diuresis, (vasodilates) counteract RAAS decrease preload decrease CO Decreased cerebral perfusion release of vasopressin/ ADH (fluid retention) from the PPG causes vasoconstriction worsening HF [3] RAAS – Blood flow to kidneys reduced, which activates the reninangiotension system (RAS) – Activation of RAAS, leads to production of renin, ACE 1, ACE 2, Aldosterone, leading to NA and water retention…….. – Preload and afterload increase – Leading to ventricular remodeling , consisting of left ventricular dilatation, myocyte hypertrophy and elongation. – Enhanced neurohormonal stimulation can lead to apoptosis, aggravation of ventricular contractility and death (ACC/AHA, 2005). [3] Release of endothelins (potent vasoconstrictor) increased peripheral resistance, increase B/P ( worsening of HF). [4] Myocardial Hypertrophy • Final compensatory mechanism • Heart wall thickens increased contractions increase CO leading to hypertrophied cardiac muscle increase O2 consumption myocardial reserve exhausted HF!!! • HF is a common outcome for many cardiovascular diseases that results in symptomatic or asymptomatic left ventricular dysfunction (LVD). • HF is a vicious cycle if left untreated. • Dysfunction begets additional dysfunction that culminates in the demise of the patient (Ramakrishnan, et al., 2005). Summary: Role of B-type natriuretic peptide (BNP) in HF • BNP is a group of natriuretic peptides that are involved in the regulation of diuresis. • Antagonizes and counteract the vasoconstricting effects of the renin angiotensin-aldosterone system (RAAS), thereby regulating blood pressure and fluid balance (Chiong & Miller, 2002). • Is a neurohormone released from the cardiac ventricles in response to increased volume and cardiac overload (Mark & Felker, 2004). Physiologic Actions of Endogenous BNP Cardiac Antifibrotic Antiremodeling Abraham WT et al. J Card Fail. 1998;4:37 Clemens LE et al. J Pharmacol Exp Ther. 1998;287:67 Marcus LS et al. Circulation. 1996;94:3184 Tamura N et al. Proc Natl Acad Sci U S A. 2000;97:4239 Zellner C et al. Am J Physiol. 1999;276(3 pt 2):H1049 Hemodynamic (balanced vasodilation) Veins Arteries Coronary arteries Neurohormonal aldosterone endothelin norepinephrine Renal sodium and water excretion BNP/RAAS : Blood Pressure and Fluid Balance RAAS (constriction) BNP (dilation) A-HEFT Study Combination Drugs: [a] Isosorbide dinitrate is an NO donor and [b] hydralazine an antioxidant that inhibits destruction of NO.[3,4] Aheft Trial Results ISDN +Hydralazine Placebo -0.1 -0.5 .01 All Cause Mortality 6.2 10.2 .02 First hospitalization for HF 16.4 24.4 .001 Change in QOL scores 6 months -5.6 -2.7 .02 Primary composite Score p Components of Primary Composite Score Kaplan-Meier survival analysis showed that the survival benefit with ISDN plus hydralazine appeared at around 180 days and increased progressively from then on. Conclusion: • A-HeFT data "support, but do not prove the existence of a protective role of NO even in the presence of neurohormonal blockade." They call for "a strategy to identify genotypic and phenotypic characteristics that would transcend racial or ethnic categories to identify a population with heart failure in which there is an increased likelihood of favorable response to such therapy." Emerging Biomarkers for HF [1] BNP [2] Mid-regional adrenomedullin [3] Gal3= Galactin 3 [4] MPO= Myeloperoxidase [5] ST2 = interleukin receptor family member [6] Markers of Renal Function (a) BUN/ Creat (b) EGFR (c) Cystatin C [7] Markers of Renal Injury (a) Albuminuria (b) NGAL =N eutrophil gelatinase associated lipocalin Summary: BNP • • • • • Regulates B/P and fluid balance. BNP elevated with ventricular stretch. BNP increases with volume overload. BNP = biomarker for CHF. weaker the heart = HIGHER BNP levels. Causes of heart failure • high blood pressure (75%) CAD diabetes problems with the heart valves ETOH abuse chemotherapy or radiation Unknown (Idiopathic dilated cardiomyopathy) Types of Heart Failure • Left-sided HF Systolic Dysfunction = EF<40% Diastolic dysfunction = EF high • Right sided HF Left sided HF [1] Exertional dyspnea (DUE) [2] Orthopnea (dyspnea at rest (lying flat) [3] Paroxysmal Nocturnal dyspnea (PND) (sudden awakening with a feeling of breathlessness 2 -5 hours after falling asleep) Left Sided HF Decreased CO [1] Fatigue [2]Weakness [3] Oliguria during the day [4] angina [5] Confusion/restlessness [6] Dizziness [7]Tachycardia [8] Pallor [9] Weak peripheral pulses [10] Cool extremities Pulmonary Congestion [1] hacking cough, worse at night [2] Dyspnea [3] Crackles/wheezes in lungs [4] Frothy, pink-tinged sputum [5] Tachypnea [6] S3/S4 Gallop [7] AFIB is common Right Sided HF Systemic Congestion [1] JVD [2] Enlarged liver and spleen [3] Anorexia and Nausea (Megase) [4]Dependent edema (legs and sacrum) [5] Swollen hands and fingers [6] Polyuria at night [7] Weight gain (most reliable indicator of fluid loss/gain) [8]Increased BP (from excess volume) or decreased BP (from failure) Signs and Symptoms of Heart Failure • The staging of HF was devised to establish the evolution and progression of the disease that can worsen over time. • These levels or stages can only advance forward and not backward. This classification focuses on patients with HF as well as those who are at risk of developing HF (ACC/ AHA, 2005). ACC/AHA Classification of Chronic Heart Failure A High risk for developing heart failure B Asymptomatic heart failure C Symptomatic heart failure D Refractory end-stage heart failure Hypertension, diabetes mellitus, CAD, family history of cardiomyopathy Previous MI, LV dysfunction, valvular heart disease Structural heart disease, dyspnea and fatigue, impaired exercise tolerance Marked symptoms at rest despite maximal medical therapy NYHA Functional Classification • NYHA I = No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea (shortness of breath) • NYHA II (Mild) Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea. • NYHA III (Moderate) Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea. • NYHA IV (Severe) Unable to carry out any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased. New Approach to the Classification of Heart Failure Stage NYHA functional class A High risk for developing heart failure (HF) None B Asymptomatic HF I Asymptomatic C Symptomatic HF II Symptomatic with moderate exertion III Symptomatic with minimal exertion D Refractory end-stage HF IV Symptomatic at rest New Approach to the Classification of Heart Failure Stage Patient Description A High risk for developing heart failure (HF) B Asymptomatic HF C Symptomatic HF D Refractory end-stage HF Hypertension CAD Diabetes mellitus Family history of cardiomyopathy Previous MI LV systolic dysfunction Asymptomatic valvular disease Known structural heart disease Shortness of breath and fatigue Reduced exercise tolerance Marked symptoms at rest despite maximal medical therapy Psychosocial Assessment • Anxiety • Depression • Empower Patient Labs • • • • • • Chest –x-ray BNP levels Echocardiogram Cardiac catheterization MUGA Scan TSH, T4 levels Interventions • Medical treatments • Surgical treatments • Non-pharmacologic interventions Medical Management • Vasodilators – ACE Inhibitors – Specific beta blockers (not all) – Nitrates • Aldosterone blockade – Inspra (eplerenone) • Inotropic Agents – Phosphodiesterase Inhibitors (Milrinone) – Cardiac Glycosides • Diuretics • Intravenous Natrecor (nesiritide) Pharmacologic Interventions HFSA Guidelines (2006) • Beta –blockers • ACE Inhibitors /ARB • Diuretics / Digoxin • Inotropic drugs Dobutamine Drugs that reduce afterload [1] ACEI [2] Natrecor Drugs that reduce preload [1] Diuretics [2] Venous vasodilators Drugs that enhance contractility [1] Digitalis Came from? Digoxin level S/S [2] BB Beta Blockers Action Side effect What to watch for before giving? Surgical interventions • • • • • LVAD BI-V Cardiac transplant Intra-aortic Balloon Pumping CRT Non-pharmacological Interventions • • • • • Diet = Low Na Daily weights Disease State Management Assess Sleep Disordered Breathing Cardiac Rehabilitation HF-ACTION enrolled 2331 patients at 82 study sites throughout the U.S., Canada and France. Patients were randomized into a group that received usual care or to a group that received usual care plus an exercise training program that began under supervision but then transitioned to home-based, self-monitored workouts. Conclusion: Based on the protocol-specified initial analysis, exercise training produced only a modest, nonsignificant reduction in the primary endpoint of all-cause hospitalization or all-cause death. QOL: Researchers also found that a higher percentage of those in the exercise group experienced more robust gains. At three months, 54 percent of those in the exercise group saw a five-point gain in overall KCCQ score, while only 28 percent of those in the usual care group met that goal. (p = .0001). Assessment • • • • • Lung Sounds Jugular Venous Distention + Hepatojugular Reflex Peripheral Edema EKG findings Heart Failure: Pearls to Remember [1] Do not miss correctable causes [2] Common condition with high mortality [3] Get echocardiogram. Get clinical picture low EF= systolic Hf, normal EF= Diastolic HF [4]Check BNP levels (helpful dyspnea or SOB) [5] ACEI, ARB = decrease mortality [6] BB=increase longevity, reduce morbidity and mortality • [7] Digoxin helpful in AFIB. • [8] Spironolactone= reduce mortality in class IV HF. Watch for hyperkalemia. • [9] AICD for patients with EF<35% (sudden death) • [10] BI-V for resistant Hf if QRS duration is >120ms • [11] transplant for resistant HF, if no serious co-morbidities. Holistic Nursing Interventions • Physiological = Physical signs and symptoms • Psychological = depression, anxiety • Emotional = sense of isolation, feeling a burden • Spiritual = faith, hope Nursing Diagnoses • • • • • Decreased Cardiac Output Fluid Volume Excess ** Impaired Gas Exchange ** Activity Intolerance Knowledge Deficit Nursing Interventions (NIC) • Calming Techniques • Cardiac Care – Rehabilitative • Electrolyte Management and Monitoring • Energy Management Nursing Outcomes (NOC) • Tissue perfusion • Cardiac pump effectiveness • Circulatory status Valvular Disease [1] Mitral stenosis (mostly women) [2] Mitral Regurgitation (Insufficiency) [3] Mitral Valve Prolapse (Marfan’s Syndrome) [4] Aortic Stenosis (Congenital valvular disease or malformation) [5] Aortic Regurgitation (Insufficiency) (75% men) Interventions [1] Non-surgical management: a. Drugs = BB, diuretic, O2 (HF meds) = Prophylactic antibiotics prior to any invasive surgery = amiodarone (afib, dec.CO 25% -30%)/ cardioversion b. Rest Interventions [2] Surgical a. Valve repair b. Balloon valvuloplasty (< 6 months, poor surgical candidate) c. Direct commissurotomy (heart surgery, clean, debrides calcium) d. Mitral annuloplasty (reconstruction) e. Valve Replacement Biologic = porcine, bovine Prosthetic = St. Jude’s (coumadin for life!) Websites: • www.hfsa.org • www.aha.org