Health behavior beliefs and physical health risk factors for
advertisement

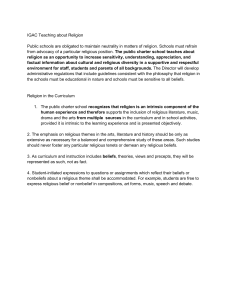
HEALTH BEHAVIOR BELIEFS AND PHYSICAL HEALTH RISK FACTORS FOR CARDIOVASCULAR DISEASE IN AN OUTPATIENT SAMPLE OF CONSUMERS WITH A SEVERE MENTAL ILLNESS: A CROSS-SECTIONAL SURVEY ARTICLE WRITTEN BY: SCOTT BRUNERO & SCOTT LAMONT PRESENTED BY: LASHONDA MARTIN INTRODUCTION Schizophrenia: A brain disorder that causes patients to be unable to distinguish reality from imagination. Affects about 3 million Americans Peak incidence of onset is 15-25 years of age in men & 25-35 in women. Symptoms: delusions, hallucinations, disorganized thinking, speech and behavior, flat affect, social withdrawal or discomfort Medications: Haldol, Seroquel, Risperdal, Clozaril INTRODUCTION (CONT’D) Known: Many factors contribute to an increased risk of developing health related diseases in those with a mental illness. Unknown: The beliefs of these patients toward their health Purpose: To understand the correlation between physical health risk factors and health behavior beliefs in schizophrenia patients. Understanding their perspective → better delivery of care. EVIDENCE FOR CARE Nursing care problem: There is little understanding the beliefs of schizophrenia patients towards their physical health. Health behavior beliefs are key in allowing patients to engage in treatment for physical health issues NURSING THEORY Health Belief Model Theory of Reasoned Action Cognitive Theory Based Model Faye Abdellah’s Patient-Centered Approaches to Nursing HEALTH BELIEF MODEL STUDY METHODS AND RESULTS Participants: 163 schizophrenia patients Methods: BP, waist circumference, BMI, smoking hx, exercise levels, demographics, family hx of diabetes and cardiovascular disease European Health and Behavior Survey (EHBS) Results: Mean waist circumference and BMI > normal population Consumers beliefs toward their health were positive. Physical health risks > than the general population norms. EVALUATION OF THE EVIDENCE ?? Critique: Cross-sectional Ethically approved by the South Eastern Sydney Illawarra Area Health Service Ethics Committee No conflicts of interest 2 authors Scholarly, peer-reviewed article Limitations: Participants on Clozapine, an antipsychotic with a known side effect of weight gain and lipid abnormality. No matched control group Prior exposure to health education programs or promotion? PATIENT CARE DESIGN Place patient, their beliefs, and their needs at the center of care Address both physical and mental health risk factors Shared/collaborative approach between mental health care givers and general physicians NURSING CARE PLAN Nursing Diagnosis Interventions Rationales Goals Readiness for enhanced power: expresses willingness to enhance participation in choice for daily living and health and enhance knowledge for participation in change 1. Encourage pt to continue to verbalize true feelings 2.Allow pt to make choices in ADL’s and their health 3. Give patient learning/educational opportunities such as programs 1. Promotes a trusting relationship between RN and pt 2. Instills confidence to help develop decision-making skills and allows them to have a voice in their care 3. Helps to build pt’s knowledge 1. Pt will develop trust in at least one staff member within one weeks 2. Pt will be able to comfortably make small decision on their own in ADL’s and care within two weeks. Ineffective health maintenance R/T lack of resources Provide pt with healthy/educational nutritional programs and exercise activities Improving pt health will decrease risk of developing a physical health problem. Pt will participate in 3 health promotion activities each week. NURSING PRACTICE Many factors including health beliefs influence health behavior Develop individualized treatment programs in addition to a physiological and/or pharmacological approach Understand the “whole” patient Individualized, accessible treatment programs Prevent physical health disease ADVOCATE ROLE Patient advocate Empathy: Build trust and rapport Effective, therapeutic communication Comfortable, healing environment Best patient outcomes SUMMARY Although patients with a mental illness have an increased risk for serious physical health problems, they have a positive attitude toward their physical healthcare. Health professionals must do more to improve the physical health of these patients by providing them with access to adequate treatment and services. REFERENCES Brunero, S., & Lamont, S. (2010) Health behavior beliefs and physical health risk factors for cardiovascular disease in an outpatient sample of consumers with a severe mental illness: A cross-sectional survey. International Journal of Nursing Studies, 47, 753-760. doi: 10.1016/j.ijnurstu.2009.11.004 Health behavior and health education: Theory, research, and practice. (2014). Retrieved from http://www.med.upenn.edu/hbhe4/part2ch3-main-constructs.shtml Videbeck, S.L. (2014) Psychiatric-mental health nursing (6th ed.). Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins.