types of diabetes - دائرة الامور الفنية
advertisement

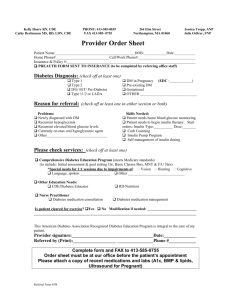
PROTOCOL FOR DENTAL PATIENT WITH DIABETES MELLITUS Introduction: Diabetes mellitus is a clinical syndrome characterized by hyperglycemia due to absolute or the relative deficiency of insulin. This can arise in many different ways but is most commonly due to autoimmune type 1 diabetes or adult onset type 2 diabetes. Lack of insulin effects the metabolism of carbohydrate, protein and fat, and can cause a significant disturbance of water and electrolyte homeostasis.[1] A third type of diabetes mellitus, gestational diabetes, represents carbohydrate intolerance with its onset or first recognition during pregnancy.[2] The most important risk associated with development of diabetes is heredity. Obesity and old age are also risk factors.[3] There a vascular aspect to diabetes mellitus, which comprises arteriosclerosis and microangiopathy especially of kidneys and eyes. Of all the best-known systemic diseases, diabetes has been the one most frequently blamed as a risk agent for periodontal disease and other oral pathogenic disorders. Therefore, every dentist should have a basic understanding of the incidence, etiology, systemic implications and possible oral associated findings of diabetes. [8] It is a common disease that affects approximately 200 million people in the world. Diabetes affects 17 people per thousand between the ages of 25 and 44 and 79 people per thousand over the age of 65. Thus, approximately 3 to 4 % of the dentist's adult patients will have diabetes. The importance of diabetes care in the dental practice is only as important as the dentist wants it to be. Practicing dental professionals must prepare themselves for the increase in the diabetic patient population and extensive medical care that they require to curtail the development of complications. Dentist's training in preventive healthcare philosophy makes them apply suited to play a significant role as part of the "Diabetes Team".[8] TYPES OF DIABETES Type I diabetes: It results from the body’s failure to produce insulin, the hormone that “unlocks” the cells of the body, allowing glucose to enter and fuel them. It is estimated that 5-10% of Americans who are diagnosed with diabetes have type1 diabetes.[6] Type 2 diabetes: this type results from insulin resistance (a condition in which the body fails to properly use insulin), combined with relative insulin deficiency. Most Americans who are diagnosed with diabetes have type2 diabetes. [6] Gestational diabetes: Gestational diabetes affects about 4% of all pregnant women – about 135,000 cases in the United States each year. [6] Pre-diabetes: Pre-diabetes is a condition that occurs when a person’s blood glucose levels are higher than normal but not high enough for a diagnosis of type2 diabetes. In incidences of pre-diabetes there are no symptoms. People may not be aware that they have type 1 or type 2 diabetes because they have no symptoms or because the symptoms are so mild that they go unnoticed for quite some time.[4] AETIOLOGY AND PATHOGENESIS OF DIABETES MELLITUS: TYPE 1 DIABETES: Type 1 Diabetes is a slowly progressive T cell-mediated autoimmune disease. Family studies have produce evidence that destruction of the insulin-secreting cells in the pancreatic islets takes place over many years. 1 Genetic factors account for about one third of the susceptibility to type 1 diabetes, the inheritance of which is polygenic. Stress may precipitate type1 diabetes by stimulating the secretion of counterregulatory hormones and possibly by modulating immune activity. Circumstantial evidence supports that proposition that dietary factors may influence the development of type 1 diabetes. [5] TYPE 2 DIABETES: Type 2 diabetes is a more complex condition than type 1 diabetes because there is a combination of resistance to the action of insulin in liver and muscle together with impaired pancreatic ᵦ cell function leading to 'relative insulin deficiency'. Type 2 diabetes is a more complex condition than type 1 diabetes because there is a combination of resistance to the action of insulin in liver and muscle together with impaired pancreatic ᵦ cell function leading to 'relative insulin deficiency. In patient with type 2 diabetes excessive production of glucose in the liver and underutilization of glucose in skeletal muscle resulting from resistance to the action of insulin. [5] Genetic factors are important in the etiology of type 2 diabetes, many genes are involved and the chance of developing diabetes is also influenced very powerfully by environmental factors. Epidemiologic studies provide evidence that type 2 diabetes is associated with overeating, especially when combined with obesity and under-activity. Age: Type 2 diabetes is principally a disease of the middle aged and elderly in the UK, it affects 10% of the population over 65, and over 70% of all cases of diabetes occur after the age of 50 years. [5] OTHER SPECIFIC TYPES Genetic defect of B cell function Genetic defect of insulin action Pancreatic disease (e.g. pancreatitis, pancreatectomy, neoplastic disease, cystic fibrosis, haemochromatosis, fibrocalculous, pancreatopathy) Excess endogenous production of hormonal antagonists to insulin (e.g. growth hormone-acromegaly; glucocorticoids-cushing's syndrome; glucagon-glucagonoma; catecholamines-phaeochromocytoma; thyroid hormones-thyrotoxicosis) Drug -induced (e.g. corticosteroids, thiazide diuretics, phenytoin) [5] Viral infection s (e.g. congenital rubella, mumps, coxsackie virus B) Uncommon forms of immune-mediated diabetes Associated with genetic syndromes (e.g. Down's syndrome; Klinefelter's syndrome; Turner's syndrome; DIDMOND (Wolfram's syndrome) diabetes insipidus, diabetes mellitus, optic atrophy, nerve deafness; Friedreich's ataxia; myotonic dystrophy) [5] GESTATIONAL DIABETES The term 'Gestational Diabetes' refers to hyperglycemia occurring for the first time during pregnancy. During normal pregnancy, insulin sensitivity is reduced through the action of placental hormones and this affect glucose tolerance. Repeated pregnancy may increase the likehood of developing irreversible diabetes, particularly in obese women; 80% of women with gestational diabetes ultimately develop permanent diabetes. [5] 2 MEDICAL EVALUATION OF THE PATIENT WITH DIABETES MELLITUS THE DIAGNOSIS OF DIABETES: When diabetes is suspected the diagnosis may be confirmed by a random blood glucose concentration greater than 199 mg/dl. When random blood glucose values are elevated but are not diagnostic of diabetes, glucose tolerance is usually assessed either by fasting blood estimation or by the oral glucose tolerance test (OGTT) table 1. The diagnostic criteria for diabetes mellitus (and normality) recommended by the world Health Organization (WHO) in 2000 is shown in table 1. [5] TABLE 1 - DIAGNOSIS OF DIABETES 1- Patient complains of symptoms suggesting diabetes 2- Laboratory evaluation: A) Test urine for glucose and ketones B) Measure random or fasting blood sugar, Diagnosis confirmed by*: Fasting plasma glucose = 126 mg/dl Random plasma glucose = 200 mg/dl C) oral glucose tolerance test (OGTT) Unrestricted carbohydrate diet for 3 days before test Fasted overnight (for at least 8 hrs.). Rest before test (30 minutes; no smoking; seated for duration of test Plasma glucose measured before, and 2 hrs after, 75 g glucose load. [5] *in asymptomatic patients two samples are required to confirm diabetes. N.B. HbA1c is not used for diagnosis. [5] DIAGNOSTIC CRITERIA FOR DIABETES: American Diabetes Association (ADA) expert committee in 1997 and 1998 has revised the diagnostic criteria for diabetes and has implemented changes in the 1979 classification as follows: a) Use of the term type 1 and type 2 diabetes instead of insulin-dependent (IDDM) and non insulin-dependent (NIDDM) to refer to the two major types of diabetes mellitus. b) Use two fasting plasma glucose (FPG) determination and c) Lowering cutoff level for FPG 126 mg/dL (7 mmol/L) to diagnose diabetes (this level of FPG is equivalent to the 200 mg/dL (11.1 mmol/L) value in the oral glucose tolerance test as in table 2. [8] Table 2 – American Diabetes Association (ADA) diagnostic criteria for diabetes and pre-diabetes (non-pregnant adults) Normal 1. Fasting plasma glucose <100 mg/dl. OR 2. Oral glucose tolerance test (OGTT) 2-hr plasma glucose <140 mg/dl. Pre-diabetes 1. A1C range of 5.7–6.4%. OR 2. Impaired fasting glucose (IFG) = fasting plasma glucose of 100–125 mg/dl. OR 3. Impaired glucose tolerance (IGT) = OGTT 2-hr plasma glucose of 140–199 mg/dl. 3 Diabetes 1. A1C > 6.5%. The test should be performed in a laboratory using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized to the Diabetes Control and Complications trial (DCCT) assay. OR 2. Fasting plasma glucose >126 mg/dl. Fasting is defined as no caloric intake for at least eight hours. OR 3. 2-h plasma glucose >200 mg/dl during an oral glucose tolerance test. The test should be performed using a glucose load containing the equivalent of 75-g anhydrous glucose dissolved in water. OR 4. Symptoms of diabetes and a casual plasma glucose >200 mg/dl. “Casual” is defined as any time of day, without regard to the time since the last meal. The classic symptoms of diabetes include polyuria, polydipsia, and unexplained weight loss. Clinical assessment: Symptomatic patients with polyphagia, polydipsia, polyuria, and weight loss may have the diagnosis of diabetes confirmed by the demonstration of a fasting blood glucose level above 120 mg/dl. Since transient elevations in blood glucose occur after meals, elevations of blood glucose after fasting are more diagnostic of an abnormal state (table 3). [3] TABLE 3 - SYMPTOMS OF HYPERGLYCEMIA Thrist, dry mouth Blurring of vision Polysuria Pruritis valuae. Balanitis (genital candidiasis) Nocturia Nausea; headache Tiredness, fatigue Hyperphagia; predilection for sweet foods Recent change in weight Mood change, irritability, difficulty in concentrating, apathy. [5] MEDICAL MANAGEMENT OF DIABETES MELLITUS Management: The method of treatment of diabetes is: 1) Dietary / lifestyle modification 2) Oral anti-diabetic agents and 3) Insulin by injection [5] 1. DIETARY / LIFESTYLE MODIFICATION A. Dietary management: The aims of dietary management are to: Achieve good glycaemic control Reduce hyperglycaemia and avoid hypoglycaemia Assist with weight management Reduce the risk of micro- and macrovascular complications Ensure adequate nutritional intake Avoid 'atherogenic' diet or those that aggravate complications, e.g. high protein intake in nephropathy. 4 B. Life style modification: The importance of lifestyle changes such as taking regular exercise, observing a healthy diet and reducing alcohol consumption should not be under-estimated in improving glycaemic control, but many people, particularly the middle aged and elderly, find them difficult to sustain. [5] Lifestyle changes include: Regular exercise Stop smoking Reducing alcohol consumption Observing a healthy diet People should, however, be educated about the potential risk of hypoglycaemia and how to avoid it. [9] Patient should be encouraged to stop smoking. It is essential that people with diabetes understand their condition and learns to handle all aspects of their management as comprehensively and quickly as possible. [5] Physical activity: Regular exercise can significantly improve glycemic control. All inmates with diabetes should be counseled on the benefits of increased physical activity, as well as the degree of exercise best suited to them. Sedentary diabetic inmates should be medically evaluated prior to undertaking aerobic physical activity that goes beyond the intensity of brisk walking. [7] Physical activity promotes weight reduction and improves insulin sensitivity, thus lowering blood glucose levels. Together with dietary treatment, a programme of regular physical activity and exercise should be considered for each person. Such a programme must be tailored to the individual’s health status and fitness. 2. Oral anti-diabetic agents and Insulin injection: Various drugs are effective in reducing hyperglycaemia in patient with type 2 diabetes. Although their mechanism of action is different, most depend upon a supply of endogenous insulin and they therefore have no hypoglycaemic effect in patients with type 1 diabetes (table 4). TABLE 4 EFFECTS OF HYPOGLYCAEMIC DRUGS USED IN THE TREATMENT OF TYPE 2 DIABETES Reduced basal glycaemia Reduced post prandial glycaemia Raise plasma insulin Increase body weight Improved lipid profile Risk of hypoglycaemia Tolerability Insulin Sulphonylureas Metformin Acarbose Thiazolinediones Yes Yes Yes Slight Yes Meglitimide and aminoacid derivitives ? Yes Yes Yes Yes Yes Yes Yes Yes No No No Yes Yes Yes No No yes Yes Yes No Slight Slight Variable No Yes Yes No No No Yes Good Good Moderate Moderate Good Good 5 3. INSULIN: Various insulin regimens are used in the treatment of diabetes. The choice of regimen depends on the desired degree of glycaemic control, the patient lifestyle and his or her ability to adjust the insulin dose (Table 5). TABLE 5 DURATION OF ACTION (IN HOURS) OF INSULIN PREPARATIONS Insulin Onset Peak Duration Rapid-acting (insulin analogues, lispro, aspart, glulisine) < 0.5 0.5-2.5 3-4.5 Short-acting (soluble (regular)) 0.5-1 1-4 4-8 Intermediate-acting (isophane(NPH), lente) 1-3 308 7-14 Long-acting (bovine ultralente) 2-4 6-12 12-30 Long-acting (insuli analogues-glargine, detemir) 1-2 None 18-24 COMPLICATIONS OF DIABETES: Microvascular / neuropathic Retinopathy, cataract Impaired vision Neuropathy Renal failure Peripheral neuropathy Sensory loss Motor weakness Autonomic neuropathy Postural hypotension Gastrointestinal problems (gastroparesis; altered bowel habit) Foot disease Ulceration Artherpathy Macrovascular Coronary circulation Myocardial ischemia/infarction Cerebral circulation Transient ischemic attack Stroke Peripheral circulation Claudication Ischemia DENTAL EVALUATION OF THE PATIENT WITH DIABETES MELLITUS MEDICAL CONSIDERATIONS: A carefully questions can give some indications that a patient could be at risk of being diabetic or be an undiagnosed diabetic especially type 2 such as: do you urinate frequently especially at night? Are you frequently thirsty? The patient should be further questioned about personal and family history of diabetes (table 6). [12] It is recommended that patient suspected by the dentist to be diabetic, should be referred to a physician for proper evaluation and diagnosis (table 6). 6 Any dental patient whose condition remains undiagnosed but who has the cardinal symptoms of diabetes (i.e., polydipsia, polyuria, polyphagia, recent weight loss, and weakness) should be referred to a physician for diagnosis and treatment. [12] Patients with findings that may suggest diabetes (headache, dry mouth, marked irritability, repeated skin infection, history of poor wound healing, blurred vision, paresthesias, progressive periodontal disease, multiple periodontal abscesses, persistent candidiasis, loss of sensation) should be referred to a clinical laboratory or a physician for screening tests. [12] The following findings are also indicative of possible diabetes; if a woman has given birth to an unusually heavy baby (>5 kg) or has had several spontaneous abortion and obese patients over 40 years of age also should be properly questioned. [8] TABLE 6 DETECTION OF THE PATIENT WITH DIABETES KNOWN DIABETIC PERSON 1. Detection by history: a. Are you diabetic? b. What medications are you taking? c. Are you being treated by a physician? 2. Establishment of severity of disease and degree of “control” a. When you were first diagnosed as diabetic? b. What was the level of the last measurement of your blood glucose? c. What is the usual level of blood glucose for you? d. How are you being treated for your diabetes? e. How often do you have insulin reactions? f. How much insulin do you take with each injection, and how often do you receive injections? g. Do you test your urine for glucose? h. When did you last visit your physician? i. Do you have any symptoms of diabetes at the present time? UNDIAGNOSED DIABETIC PERSON 1. History of signs or symptoms of diabetes or its complications 2. High risk for developing diabetes a. Parents who are diabetic b. Gave birth to one or more large babies c. History of spontaneous abortions or stillbirths d. Obese. e. Over 40 years of age 3. Referral or screening test for diabetes DENTAL CONSIDERATIONS: Based upon the information gathered, generally we have two groups of patient: 1. Patients not known to have diabetes mellitus: These are patients with sign and symptoms suggesting the possible diagnosis of diabetes. Patients with positive family history of diabetes, and Patients documented to have evaluated of blood glucose level. All of them should be referred for medical evaluation and blood glucose level determination prior to the initiation of comprehensive dental treatment. [8] 2. Patient known to have diabetes mellitus: For this group, time of onset of diabetes, type of required therapy (control of diet, oral hypoglycemic agents, insulin therapy), adequacy of control (fasting blood sugar, 7 hemoglobin A1c level, history of hypoglycemia, history of ketoacidosis), complication of diabetes (vascular, neurological, renal, infections) must be taken in consideration. [8] RISK CATEGORIES FOR THE PATIENT WITH DIABETES MELLITUS REGARDING DENTAL TREATMENT: Patients at Low risk: Patients with good metabolic control on a stable medical regimen are at low risk. These patients are asymptomatic and have no neurologic, vascular, or infectious complications. Fasting blood sugar < 200 mg/dl Hemoglobin A1c level < 7% Patients at Medium risk: These patients have occasional symptoms but are in reasonable metabolic balance. There is no recent history of hypoglycemia or ketoacidosis, and few of the complications of diabetes are present. Fasting blood sugar < 250 mg/dl Hemoglobin A1c level < 7% to 9% Patients at High risk: These patients have multiple complications of the disease and are under poor metabolic control. There is a history of frequent hypoglycemia or ketoacidosis, and there is often a constant need to adjust insulin dosages. Fasting blood sugar > 250 mg/dl Hemoglobin A1c level > 9% These risk categories should suggest some specific guidelines for management. [8] DENTAL MANAGEMENT OF THE PATIENT WITH DIABETES MELLITUS GENERAL GUIDELINES The dentist should know if the patient has a history of hypoglycemic attacks and the accompanying signs and symptoms. The chances of having a hypoglycemic attack are increased if there have been previous attack. [8] It should be stressed that the dentist should take all the necessary precautions in order to avoid the occurrence of hypoglycemic attack while the patient is undergoing dental treatment. The primary goal should be to avoid untoward metabolic imbalances during the period of dental therapy. Patients should be carefully instructed about their diet and their medications during the course of therapy so as to minimize problems related to either hyperglycemia or hypoglycemia.[3] 1. DIET: A major goal in the dental management of patients with diabetes who are being treated with insulin is to prevent insulin shock during the dental appointment. Patients should be told to take their usual insulin dosage and to eat normal meals before their dental appointment, which is usually best scheduled in the morning. When such a patient comes for the appointment, the dentist should confirm that the patient has taken insulin and has eaten breakfast. In addition, patients should be instructed to tell the dentist whether at any time during the appointment, they feel symptoms of an insulin reaction. [12] It is advisable to have in the dental office orange juice or any other form of sugar. Preparedness should include availability of different forms of orally administered rapidly absorbed carbohydrates such as fruit juice, sodas, cake icing, plain sugar, ice cream, candies, etc. patients with hypoglycemia will recover from the attack within 10 to 20 minutes after orally administering 15 g of carbohydrate, this is 8 equivalent to 4 to 6 ounces of fruit juice or soda, the same result will be achieved with 4 teaspoons of plain sugar. [8] 2. MEDICATION The dentist must know the type and dose of insulin as well as any other medications that the patient is taking. [8] The patient must be advised not to change the insulin dose and time of application as well as not to change his/her diet. [8] Patients should be instructed to take their normal dosage of oral hypoglycemic agents for all patient dental procedures. [3] In order to avoid an episode of hypoglycemia while undergoing dental treatment it is advisable to schedule the patient based on the time of highest insulin activity which varies from 30 minutes to 8 hours after injection depending on the type of insulin. Therefore, the appointment does not need to be necessarily in the morning. [8] 3. MINIMIZATION OF STRESS The dentist should attempt to minimize stress to the diabetic patient. Whenever feasible, lengthy procedures should be spread over several shorter appointments. Appropriate sedation should be considered. [3] Emotional and physical stress increases the amount of secreted cortisol and epinephrine, which induce hypoglycemia. Therefore, if the patient is very apprehensive pre-treatment sedation should be contemplated. [8] 4. MINIMIZING THE RISK OF INFECTION: Host immune defenses are altered in the patient through several mechanisms. High glucose concentrations in blood and body fluids promote the overgrowth of certain fungal pathogens, particularly the Candida species. Infections, whether from the mouth or other sites, will sometimes cause an increase in blood glucose levels. Treatment of infection in a patient with diabetes requires aggressive antibiotic therapy. [8] Instruct the patient to leave dentures out at night and to soak denture in a 1% sodium hypochlorite solution for 15 minutes with thorough rinsing under running water for at least 2 minutes, before bedtime. [8] Antibiotic should be prescribed for patients who have a difficult to control diabetes or is under high insulin dosage in order to prevent secondary infections or complication of the pre-existing infection and to facilitate wound healing. The basic aim of treatment is to simultaneously cure the oral infection and respond to the need to regain control of the diabetic condition. Patients who are receiving insulin usually require additional insulin, which should be prescribed by their physician; non–insulin-controlled patients may need more aggressive medical management of their diabetes, which may include insulin, during this period. The dentist must treat the infection very aggressively by incision and drainage, extraction, pulpotomy, warm rinses, and antibiotics. [12] 5. MEDICAL CONSULTATION: The physician should be consulted on specific management issues in order to ascertain the severity of the patient's disease and the degree of control over it. The physician should also be involved in decisions about insulin coverage during dental treatment. [3] 9 6. TREATMENT PLANNING MODIFICATIONS: The patient with diabetes who is receiving good medical management and is under good glycemic control without serious complications such as renal disease, hypertension, or coronary atherosclerotic heart disease can undergo any indicated dental treatment. If diabetes is under good control, even cardiac transplantation can be safely performed. However, in patients with diabetes who have serious medical complications, the plan of dental treatment may need to be altered. Studies have indicated that many dental patients with diabetes are not under good glycemic control. Elevated fasting blood glucose levels render the dental patient more susceptible to complications. [12] SPECIFIC GUIDELINES: Patients at Low risk: Properly controlled type 1 and type 2 diabetes patients usually can undergo all treatment without special precautions. Patients with diabetes who have no evidence of complications and whose disease is under good medical control, as determined by consultation with the patient's physician, require little or no special attention when receiving dental treatment, unless they develop a significant dental or oral infection that is possibly accompanied by swelling or fever. [12] Patients at Medium risk: General guidelines regarding diet control, minimization of stress, and risk of infection are increasingly important for patients at medium risk. Patient advised to take usual insulin dosage and normal meals on day of dental appointment; information confirmed when patient comes for appointment. Advise patient to inform dentist or staff if symptoms of insulin reaction occur during dental visit. These patients can undergo restorative dentistry utilizing normal protocol. [3] Aggressive soft tissue management, periodontal scaling, root planning and periodontal surgery are indicated depending on the level of periodontal disease involvement. The patient's level of disease control should be reassessed on a regular basis and related to any oral health problems they may have.[8] If is lengthy, especially surgical procedure is to be undertaken; the patient's physician should be consulted. [8] Consultation with the patient's physician is a must when the patient has systemic complications of diabetes such as heart or renal disease.[8] Some patients with type 1 diabetes who are being treated with large doses of insulin have periods of extreme hyperglycemia and hypoglycemia (brittle diabetes), even when given the best of medical management. For these patients, antibiotic prophylaxis can be considered and close consultation with the physician is required before any dental treatment is started. [12] Patients who have not seen their physician for a long time, who have had frequent episodes of insulin shock, or who report signs and symptoms of diabetes may have disease that is unstable. These patients should be referred to their physician for evaluation, or the physician should be consulted to establish the patient's current status. [12] The patient's physician should be consulted about dietary recommendations for the postoperative period. One suggestion is to have the patient use a blender to prepare his or her usual diet so that it can be ingested with minimum discomfort; alternatively, special food supplements in a liquid form may be used. The physician also may alter the patient's insulin regimen according to his or her ability to eat properly, and according to the extent of the surgery to be performed. [12] 10 Patients at High risk: These patients can undergo oral examination after appropriate measures are taken to minimize stress. All other procedures should be deferred until the medical status is stabilized. [3] DENTAL MANAGEMENT OF THE PATIENT WITH DIABETES AND ACUTE ORAL INFECTION Host immune defenses are altered in the diabetic patient through several mechanisms. High glucose concentrations in blood and body fluids promote the overgrowth of certain fungal pathogens, particularly the Candida species. Infection, whether from the mouth or other sites, will sometimes cause an increase in blood glucose levels. [8] Treatment of infection in a patient with diabetes requires aggressive antibiotic therapy as follow: 1. Non–insulin-controlled patients may require insulin; consultation with physician required 2. Insulin-controlled patients usually require increased dosage of insulin; consultation with physician required 3. Patient with brittle diabetes or receiving high insulin dosage should have culture(s) taken from the infected area for antibiotic sensitivity testing a. Culture sent for testing b. Antibiotic therapy initiated c. In cases of poor clinical responses to the first antibiotic, a more effective antibiotic is selected according to sensitivity test results d. These patients may require hospitalization during management of an infection. The patient's physician should be consulted and should become a partner during this period. [12] 4. Infection should be treated with the use of standard methods a. Warm intraoral rinses b. Incision and drainage c. Pulpotomy, pulpectomy, extractions, etc. d. Antibiotics MEDICAL MANAGEMENT OF DIABETIC EMERGENCIES Dental practitioners should encourage diabetic patients who self-monitor blood glucose levels to bring their glucometer to the dental office at each visit. If glucose levels are at or below the lower end of the normal fasting range (80 to 120 mg/dL), then it may be necessary for the patient to consume a fast acting carbohydrate. The most common causes of hypoglycemia include injection of excess insulin, delaying or missing meals or snacks with the usual dose of insulin, and increasing exercise without adjusting the insulin dose (exercise reduces the requirement for insulin). The signs and symptoms include confusion, shakiness (tremors), agitation, belligerence, sweating (diaphoresis), and tachycardia. The dentist must know the time, dose, and type of insulin the patient took that day and the time, amount, and type of carbohydrate (simple vs complex) the patient consumed before the dental visit. In this way, the dentist can match the patient’s plasma insulin levels with the food intake, thus determining the likelihood of hypoglycemia.[10] 11 How to manage Hypoglycemia: If a glucometer determination shows hypoglycemia, then the administration of sugar under the tongue usually rapidly reverses the hypoglycemia. The glucose can be rapidly absorbed from the sublingual site. Patients can usually be treated with rapid acting oral carbohydrates, e.g. fruit juice, packets of granulated sugar, glucose powder neat or dissolved in water. After ten minutes this short acting carbohydrate should be followed up with food which contains longer acting carbohydrate. It is important that the patient is not left alone until all danger of hypoglycaemia has passed. If the patient is sedated or unable to take food or drink by mouth, then 25 to 30 mL of 50% dextrose or 1 mg of glucagon can be administered intravenously, intramuscularly, or subcutaneously. A glucagon injection causes glycogenolysis in the liver. It will rapidly reverse hypoglycemia, usually within 15 minutes. How to manage Hyperglycemia: The dentist must be aware of the signs and symptoms of hyperglycemia and be prepared to manage it. If a glucometer determination shows hyperglycemia, then the dentist must contact the patient’s physician and refer the patient for immediate medical evaluation, or the patient can administer a loading dose regular insulin at 0.1 units/kg body weight to a maximum of 10 units followed by an infusion of regular insulin at 0.1 units/kg body weight/hour, to a maximum of 10 units/hour to treat the hyperglycemia. [11] In some cases, hyperglycemia can present with symptoms similar to those of hypoglycemia (eg, confusion and disorientation). If a glucometer is not available to determine blood glucose levels accurately and the conscious patient has symptoms suggestive of hypoglycemia, then the dentist must administer glucose or fruit juice. Treat patients presumptively for hypoglycemia if they experience tremors, diaphoresis, tachycardia, or disorientation and agitation. If the symptoms were from hyperglycemia rather than hypoglycemia, then the additional amount of carbohydrate will generally cause no harm. The best way to determine the true nature of a diabetic emergency quickly is to measure blood glucose levels with a glucometer. The accuracy of the glucometer readings is generally within an error range of 5%. LOCAL ANESTHETICS AND EPINEPHRINE For most patients with diabetes, routine use of local anesthetic with 1:100,000 Epinephrine should be tolerated well. However, epinephrine has a pharmacologic effect that is opposite that of insulin, so blood glucose could rise with the use of epinephrine. In diabetic patients with hypertension, post myocardial similar to those for patients with cardiovascular conditions and may be even more strict for those with diabetes and cardiovascular conditions, as along with determination of functional capacity via metabolic equivalent levels METs. [12] Diabetic patients with more than 4 METs are usually more stable, and when other indicators of physical status are also present (e.g., glycemic control), they are able to tolerate most dental procedures. Conversely, patients with METs values lower than 4 may be more likely to encounter complications and should be approached with caution. Obviously, diabetic patients may fluctuate between these states from time to time and from appointment to appointment. [12] 12 SUMMERY TABLE 1 DIABETES MELLITUS: GENERAL INFORMATION DEFINITION: Diabetes mellitus is a clinical syndrome characterized by hyperglycemia due to absolute or the relative deficiency of insulin. INCIDENCE Approximately 3 to 4 % of the dentist's patients TYPES OF DIABETES MELLITIS PRE-DIABETES: Occurs when a person’s blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. TYPE 1 DIABETES: Results from the body’s failure to produce insulin, TYPE 2 DIABETES: Results from insulin resistance, combined with relative insulin deficiency. GESTATIONAL DIABETES: Represents carbohydrate intolerance with its onset or first recognition during pregnancy. SYMPTOMS Polydipsia Polyuria Polyphagia Weight loss Signs: Glycosuria SUMMERY TABLE 2 AETIOLOGIC CLASSIFICATION OF DIABETES TYPE 1 DIABETES: Immune-mediated Idiopathic TYPE 2 DIABETES: Combination of resistance to the action of insulin in liver and muscle together with impaired pancreatic ᵦ cell function. Many genes are involved and also influenced by environmental factors. Evidence that type 2 diabetes is associated with overeating, especially when combined with obesity and under-activity. OTHER CAUSES OF DIABETES MELLITUS INCLUDE: Genetic defects of islet cell function Genetic defects in insulin action Endocrinopathies such as Cushing’s disease or syndrome Drug- or chemical-induced hyperglycemia Infections Insults to the pancreas from a variety of causes such as: Pancreatic Cancer Cystic Fibrosis Trauma Pancreatitis GESTATIONAL DIABETES: During normal pregnancy, insulin sensitivity is reduced through the action of placental hormones and this affect glucose tolerance. 13 SUMMERY TABLE 3 MEDICAL EVALUATION OF THE PATIENT WITH DIABETES MELLITUS CLINICAL ASSESSMENT Patient complains of symptoms suggesting diabetes LABORATORY EVALUATION: (non- pregnant adults) NORMAL 1. Fasting plasma glucose <100 mg/dl. OR 2. 2. Oral glucose tolerance test (OGTT) <140 mg/dl. PRE-DIABETES 1. A1C range of 5.7–6.4%. OR 2. Fasting plasma glucose of 100–125 mg/dl. OR 3. Impaired glucose tolerance (IGT) = 140–199 mg/dl. DIABETES A1C > 6.5%. OR 2. Fasting plasma glucose >126 mg/dl. OR 3. 2-h plasma glucose >200 mg/dl during an oral glucose tolerance test. OR 4. Symptoms of diabetes and a casual plasma glucose >200 mg/dl. SUMMERY TABLE 4 MEDICAL MANAGEMENT OF DIABETES MELLITUS GOALS: Optimal metabolic control. Prevent Ketoacidosis Prevent hypoglycemia. METHOD OF TREATMENT: Dietary / lifestyle modification. Oral anti-diabetics. Insulin. SUMMERY TABLE 5 DENTAL EVALUATION OF THE PATIENT WITH DIABETES MELLITUS MEDICAL CONSIDERATIONS: Known Diabetic Person: 3. Detection by history: 4. Establishment of severity of disease and degree of “control” Undiagnosed Diabetic Person: 4. History of signs or symptoms of diabetes or its complications 5. High risk for developing diabetes 6. Referral or screening test for diabetes 14 DENTAL CONSIDERATIONS: Risk Categories for Dental Patient with Diabetes Mellitus: 1. Patients at Low risk Fasting blood sugar < 200 mg/dl Hemoglobin A1c level < 7% 2. Patients at Medium risk Fasting blood sugar < 250 mg/dl Hemoglobin A1c level < 7% to 9% 3. Patients at High risk Fasting blood sugar > 250 mg/dl Hemoglobin A1c level > 9% SUMMERY TABLE 6 DENTAL MANAGEMENT OF THE PATIENT WITH DIABETES MELLITUS GENERAL GUIDELINES 1. DIET: patient: patient should eat normal meals before dental appointment Any form of sugar should be available in the dental office 2. MEDICATION: Patients should take their usual insulin dosage 3. MINIMIZATION OF STRESS 4. MINIMIZING THE RISK OF INFECTION: 5. MEDICAL CONSULTATION 6. TREATMENT PLANNING MODIFICATIONS: Dental treatment plan may need to be altered with diabetic patients have serious medical complications. SPECIFIC GUIDELINES Patients at Low risk: Properly controlled diabetes patients usually can undergo all treatment without special precautions Patients at Medium risk: Restorative dentistry utilizing normal protocol Surgical procedures: Extractions, aggressive soft tissue management, periodontal scaling, root planning and periodontal surgery are indicated depending on the level of periodontal disease involvement lengthy, especially surgical procedure is to be undertaken; the patient's physician should be consulted Patient with brittle diabetes or receiving high insulin dosage should have culture(s) taken from the infected area for antibiotic sensitivity testing Patients at High risk: Undergo oral examination after minimize stress. All other procedures should be deferred until the medical status is stabilized 15 SUMMERY Table 7 MEDICAL MANAGEMENT OF DIABETIC EMERGENCIES Fasting blood sugar (Glucometer) reading Hypoglycemia Hyperglycemia < 70 mg/dl >200 mg/dl Defer elective treatment Defer elective treatment Or Or Give Carbohydrates Give hypoglycemic (insulin) Or Refer to physician REFERENCES 1. B.M.FRIER, M. FIHIER. Davidson's Principles and Practice of Medicine 20ed. Pages 805-808. 2. Little JW, Falace DA, Miller CS, Rhodus NL. Diabetes. In: Dental management of the medically compromised patient. 5th ed. St Louis: Mosby; 1997. p. 387-409. 3. Stephen T. Sonis, Robert C. Fazio, Leslie Fang, Principles And Practice Of Oral Medicine 4. AHA American Heart Association D:\systemic diseases \مواضيع طبيةdiabetes mellitis\DIABETES MELLITIS new\Diabetes\Symptoms, Diagnosis & Monitoring of Diabetes.mht 5. B.M.FRIER, M. FIHIER. Davidson's Principles and Practice of Medicine 20ed. Pages 810-815, pages 817-819 and page 829 6. D:\systemic diseases \مواضيع طبيةdiabetes mellitis\DIABETES MELLITIS new\Weld Diabetes Project.mht Copyright 2010 Weld County Govenment | Disclaimer 7. Management of Diabetes - Federal Bureau of Prisons Clinical Practice Guidelines November 2010 8. Dan wollner, Pacific Health Dialog Vol. 10 No.1.2003, view point and perspactives. 9. Dr A.A.S. Alwan, Regional Adviser, Noncommunicable Diseases. Management Of Diabetes Mellitus Standards Of Care And Clinical Practice Guidelines. WHO Regional Office for the Eastern Mediterranean. 10. Mealey B. Impact of advances in diabetes care on dental treatment of the diabetic patient. Comp Dent Ed 1998;19:41-58. Little JW, Falace DA, Miller CS, Rhodus NL. Diabetes. In: Dental management of the medically compromised patient. 5th ed. St Louis: Mosby; 1997. p. 387-409 11. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN: Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32:1335–1343, 2009 12. James W. Little, DMD, MS, Donald A. Falace, DMD, Craig S. Miller, DMD, MS, Nelson L. Rhodus, DMD, MPH, Dental Management of the Medically Compromised Patient, 7th ed. Part Six – Endocrine And Metabolic Disease, Chapter 15 – Diabetes Mellitus Copyright © 2007 Mosby, An Imprint of Elsevier مع تحيات قسم صحة الفم واألسنان في دائرة األمور الفنية dentalhealthmoh@yahoo.com 16