F2_-_Abs_condensed
advertisement

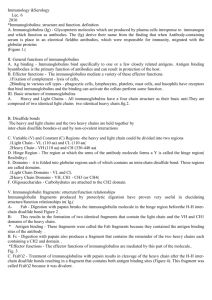
Antibodies (Fleischmann) Adaptive immunity has 2 parts – Humoral (B cells & Plasma cells) & Cell-mediated (CD8+ Tc). Overstimulation leads to autoimmunity or blood cancers while understimulation can create a lack of sufficient memory. o Humoral immunity occurs from monocytes, dendritic cells and other APCs presenting Ag to CD4+Th2 cells Th2 secretes cytokines B-cell activation B-cell differentiation to plasma cells that produce Abs Antigens: infectious agents, toxins & foreign cells that are recognizable by TCRs & Abs of humoral immunity. o Epitopes: are immune recognition sites on Antigens, typically hydrophilic. (more complex the Ag more epitopes). Linear epitopes are 5-7 aa & conformational epitopes can have discontinuous aa groups spread over a 15-22 aa sequence. The paratope of the antibody or TCR binds here. B cells recognize epitopes that are linear or conformational region on antigen surface T cells recognize epitopes that are linear regions cut from Ag & presented to TCR w/ MHC o Thymus-dependent antigens are B cells that need Th2 activation. Proteins are the most immunogenic o Thymus-independent antigens are primitive. Polysaccharides can provoke an immune response (like ABO blood groups). Nucleic acids need to be bound to a protein carrier to be antigenic (when DNA is released following cell death, can provoke immune response), this happens w/ Lupus and other autoimmune diseases. Lipids also need to be bound to proteins to be antigenic. o Haptens are small molecules that are antigens but not immunogens b/c they are too small to stimulate an immune response without a carrier even though they can bind to Ab. Penicillin is an example, it will combine w/ Albumin (blood protein) causing an allergic response. ‘HALF’ Antibodies: members of immunoglobulin family of proteins. Produced by B cells & plasma cells. o When a single plasma cell cancerous cell that causes MYELOMA. These pts overproduce a homogenous Ig. Also have some Ig proteins that spill into their urine = Bence-Jones proteins that are dimers of kappa or lambda light chains o 5 types of Heavy chain ex: IgD w/ δ heavy chain, etc o Fab region = variable region (VDJ / idiotypic / paratope = Ag binding!) o Fc = constant region. Binding to MOS here; also bind & activate C1 here. o Papain cleaves above hinge 2 Fab & 1 Fc (can bind to Ag) o Pepsin cleaves below hinge 1 Fab₂ & degraged Fc (can still cross link Ag – good for Dx tests) o Light chain = 1 variable + 1 constant o Heavy chain = 1 variable + 3-4 constant 3 constant + hinge (δ, , α H chains) = 4 Ig domains (including variable region) 4 constant, no hinge (μ & ) = 5 Ig domains (including variable region) IgM – pentamer – want to keep rigid so none wander away. [hand] IgE – surface of basophil or mast cell – needs to X-link bxt 2 Abs & Ag. Rigid structure here allows the cell to know its bound to membrane b/c membrane will bend. [arm] o Immunoglobulin fold = structure. This is a ‘sandwich’ of 2 β-pleated sheets w/ antiparallel β strands connected by loops giving rigid structure. CDRs (complementarity-determining regions) are in variable region and made up the paratope, also known as hypervariable region b/c give diversity bxt Abs. Antigen-Antibody Binding o This binding is d/t non-covalent forces that have an additive effect strong interaction overall. o Antibody avidity is the sum of all the interactions between Ag and Ab which is dependent on affinity between paratope & epitope as well as the number of epitopes on the antigen as well as the number of paratopes on antibody. o Antigen binding conformational change of Antibody. This allows complement to bind. o Hinge region of Ab (IgG, IgD & IgA) between constant domains allows for a range of separation of the arms of the Ab, allows for interactions between paratopes on different arms of an Ab and epitopes on different antigens, cross-linking can occur if antigen has more than 1 epitope leading to precipitation. IgM Ab can precipitate Ags d/t multimeric structure. Soluble IgE does not b/c its bound to mast cells and basophils, but X-linking of these Abs key to degranulation. o Cross reactivity of antigens occurs when antigens have same aa sequence = common epitope, or when there is a mismatch b/c they are only different by one aa. Medically imp when we make Abs to Strep pyogenes b/c they have a similar protein to heart valves and can cause Post-Strep Rheumatic F o Most Abs are expressed as soluble Abs that are secreted into fluid. But others are on the surface of immune cells (IgD on B cells, some IgM is on B cells, IgE is on mast cells & basophils) Antibody Functions o B cells expressing IgD or IgM bind Ag internalization of Ag:Ab complex Ab degraded; Ag digested to peptides in phagolysosomes specific peptide sequences (epitopes) of Ag are bound to MHC II presented to Th cells either there is more Ab made or Tc cells activated (UPTAKE & PROCESSING) o NEUTRALIZATION OF ANTIGEN by binding to epitopes on antigen blocking it from binding to target o Facilitate uptake of antigens by phagocytic cells. (OPSONIZATION) o AGGLUTINATION OF ANTIGENS Phagocytosis occurs more readily o PRECIPTIATION OFANTIGENS when agglutination grows, are also more readily phagocytosed…but if it doesn’t happen quickly they can activate complement and damage to site of precipitation can occur. o COMPLEMENT ACTIVATION if cross linking of antigen occurs w/ Ab binding lysis of bacteria w/ C9 attack complex Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC) o Activated when Fc portion of Ab binds to Fc receptors on NK cells, eosinophils, neutrophils or MOS leading to death of bacteria, viruses, parasites & tumor cells. Ab is providing specificity for killing. Differs from opsonization b/c Ag is killed without being phagocytosed. Passive Immunity refers to Abs that pass through placenta or are secreted in body fluids. Mom’s IgG passes through placenta to provide systemic protection for the NB. IgA (and some IgG) can be secreted in body fluids to protect v. bacterial colonization & invasion. IgA is in colostrums & milk. Ab Isotypes: different heavy chains = 5 different Ab classes. Light chains Heavy chains Other chains IgM Mu chain J chain IgD Delta chain Kappa chain IgG Gamma 1-4 chains Lambda chain IgE Epsilon chain IgA Alpha 1-2 chains J chain & Secretory component o IgM – monomer on B cell surface; pentamer is in serum, secreted into mucosal secretions. Good at virus neutralization, poor at toxin neutralization. Is bactericidal, causes agglutination & precipitation as well as complement fixation. Doesn’t bind to MOS Fc receptors. Indicative of recent infection, doesn’t cross placenta, not good for IC pts b/c has short half-life, NOT useful to block TNF production or allergens. Not in IS fluids, but is in bodily secretions. o IgD – monomeric – on surface of B cells for Ag recognition – minor serum component. Sometimes overexpressed in myeloma pts. Membrane associationed. o IgG - 2⁰ immune response – most abundant in serum (80%) – imp in pulmonary secretions – 4 subclasses (IgG3 long gamma chain, shortest half life, great C fixation). Neutralizes toxins & viruses, bactericidal, agglutinates & precipitates Ags, fixes complement, DOES bind to MOS Fc receptors. Crosses placenta, can mediate hemolytic disease of NB (Rh), good for IC pts, blocking TNF (Rheumatoid arthritis), blocking allergens. Is in IS fluid, not in bodily secretions. o IgA – in bodily secretions (dimeric), blood (monomeric, dimeric or trimeric). J chain stabilizes when monomeric. Neutralizes viruses & toxins. Bactericidal, agglutinates & precipitates Ag. Doesn’t bind to MOS Fc receptors. Highest daily production, in secretions. High lvls in colostrums = helps NBs protect v. respiratory and intestinal infections. Secretion occurs by dimeric IgA (stabilized by J chain) being secreted into blood by a plasma cell where it binds to Poly-Ig receptor on membrane, then its internalized in an endocytic vesicle where the Poly-Ig receptor is cleaved allowing the larger peptide associated with the IgA to be secreted on luminal side. o IgE – most is bound to Fc epsilon receptors on mast cells or basophils. Cross linking on these cells histamine release, PG synthesis & Cytokine production. Fights parasites & fungal lung infections. Allergies are d/t overexpression of IgE to certain antigens, cross-linking is easier and when antigen is around lots of mast cells are degranulated causing an allergic reaction. Ab allotypes: differences in constant region between strains. Ab idiotypes: differences in variable region. Antibody diversity occurs from errors at joining sites or segments, hypermutation of gene segments and mixing and matching H and L chains. All happens before leaves BM. o Ig Heavy Chains – 2/Ab w/ V, D, J & C gene segments. C = constant. Rearrangement occurs by DNA D & J regions joined via looping out, next V is added to the DJ segment creating the mature H-chain DNA. Transcription occurs giving I⁰ RNA transcript that undergoes polyadenylation & RNA splicing to give mRNA that will undergo translation resulting in a nascent polypeptide w/ leader sequence (L) attached to help it cross the membrane. L sequence is cleaved resulting in either μ or δ heavy chain for IgM and IgD. o Ig Light Chains – 2 types exist (κ or λ) and have V, J and C gene segments. Rearrangement occurs as it did w/ heavy chains, only difference is lack of D segment. o Rearrangement occurs between recombination signal sequences (RSSs) on DNA and is catalyzed by recombination-activating genes: RAG-1 & RAG-2. RSSs have 7 & 9 bp sequences separated by either a 12 or 23 bp spacer and are inverted repeats that forms a stem-loop. RAGs come together, ends cut & DNA that was between them is looped out. P & N-nucleotides are added following cleavage by RAG. Single stranded regions are formed, then copied (P-nucleotides added) hairpin loop that SPRUNGS open N-nucleotides are added until a match is made fills in sequences join if divisible by 3 its readable! Rearrangement is productive if the number of nts added is readable b/c this leads to greater diversity. Its nonproductive if number of nts added causes genetic code to be read out of phase, which is common. Our B cells might be able to rearrange Ig gene on the other chromosome so aren’t totally SOL. Allelic exclusion ensures that a B cell will make an Ab with single specificity by having one allele expressed and 2nd allele can be rearranged if 1st is non-functional. Mature (but not activated) B cells express membranebound IgD & IgM (pre-mRNA transcript has 4 poly-A sites, if 2nd site is read IgM is made after splicing and 4th site IgD), secretory IgM is expressed as B cells are activated by Ag to divide & differentiate (pre-mRNA transcript has 2 poly-A sites w/in Cμ region…if M1, M2 are spliced out sIgM), and with continued division & differentiation they can undergo class switching (DNA rearrangements and looping out of Constant regions) IgM of IgD IgG IgE IgA; cytokines are also involved. Somatic hypermutation causes mutations to accumulate in the variable region of the Ig gene creating diversity. If the mutation causes the Ab to bind Ag more strongly = affinity maturation. Signal strength related to time attached. CML is a disease that gives rise to the Philadelphia Chromosome (novel Chr 22) from a 9:22 translocation. This places a proto-oncogene under control of λ light chain gene promoter on Chr 22 Overproduction Burkitt’s Lymphoma results from a reciprocal translocation of chromosomes 8 & 14, placing c-myc under control of heavy chain promoter on Ch 14. C-myc normally tells cells to divide. We want to be able to use Abs to make vaccines by generating Abs against Ags by creating an Ab to the Ab’s paratope (structural analog of toxin (Ag)) so that your body will think it has memory to it and will have Abs if actual toxin is encountered. Monoclonal Abs can be generated by combining cells of a recently immunized mouse with mouse myeloma cells (that are drug resistant) grow in drug-containing environment see if they make Ab to the Ag used to immunize mice then clone! o Inflixibmab blocks most severe Sx of RA & Crohn’s by targeting TNF. Palivizumb is for RSV esp in male infants – it stimulates immune system & is given in combo w/ Ribavirin. Trastuzamab/Herceptin blocks epidermal GF for breast cancer. To use mice to produce humanized Abs we either have to 1) make mini human chr w/ genes for H & L chains, put in mouse, mouse makes human Abs, extract them. 2) cause mouse to have Ab response, do recombination in test tube, take variable region in mouse and attach to constant region in human (which is what would be attacked). Progenitor B-cells (pro B-cells) express c-Kit B-cell binds to stem cell factor expressed on BM stromal cells = Igα/Igβ expressed (which have ITAMs) Heavy chain gene rearrangement pro B-cell proliferates & differentiates into Precursor B-cells (Pre B-cells) Pre B-cell expresses IL-7R stimulated to divide & differentiate light chain rearrangement: β chain rearrangement then α chain rearrangement Immature B cell IgM mRNA mIgM on cell surface Mature, naïve B cell pre-mRNA differentially spliced into IgM & IgD mRNAs mIgM/mIgD on cell surface B-1 B cells. These are ‘nontraditional’ thymus-independent B cells that are produced before the major group of B cells, are comprise 5% of B cell population. They are mostly found in the peritoneal & pleural cavities. Variable regions – not many of them, bind Ag w/ lower affinity. They are more likely to respond to carbs than to protein Ag, Ab are somewhat multi-specific and can bind several Ags. Class switching isn’t common, no hypermutation occurs = no affinity maturation. They are self renewing (which is different than B-2 cells); can generate more naïve B-1 cells. Clonal deletion (negative selection of self-reactive B cells) occurs in the bone marrow. This helps limit the development of Ab-mediated autoimmunity. Immature B cells that are expressing mIgM will recognize selfAg and undergo apoptosis OR undergo editing of light chain genes to produce a different light chain that when combined w/ the heavy chain doesn’t recognize self-antigen. Negative selection of self-reactive B-cells can also occur in the periphery because not all self-antigens are expressed in the bone marrow. Thymus dependent antigens (TD Ags) require direct contact of B cell w/ Th2 cells to make Ab response. Thymus independent antigens (TI Ags) don’t need Th2 cell activity to induce Ab response. o Type 1 TI Ag = LPS & other bacterial CW components B-cells bind LPS via either toll-like receptor 4 (TLR4) or the B cell receptor (specific Ab + Ig-α and Ig-β) TLR4 binding is non-specific, so polyclonal activation occurs: B cells w/ lots of Abs are activated. Acting as a B cell mitogen. This type of Ag can activate both immature & mature B cells b/c it doesn’t require a surface Ab molecule. Only IgM is produced. Binding of Ag provides signal 1; binding of Th2 cell via CD40:CD40L provides signal 2 o Type 2 TI Ag = highly repetitious molecules like polymeric proteins (flagellin) or bacterial CW polysaccharides w/ repeated subunits. B cells bind Ag by crosslinking of the B cell receptor (specific Ab + Ig-α and Ig-β) Only mature B cells are stimulated Mostly IgM is produced Th2 activity isn’t needed but Cytokine production by Th2 cells is needed for full B cell response & for class switching to other isotypes. Binding of Ag provides both signal 1 and 2 needed for activation Ig-α/Ig-β has an ITAM motif that is activated by Ag cross-linking Ab on the surface of the B cell that can transducer a signal, initiating a cascade of events. This is helpful b/c mIgM & mIgD’s cytoplasmic tails are too short to cross the membrane. o Lots of phosphorylations activate PLP C activate transcription factor NF-κB o BCR activation G proteins activated activation of transcription factors Rho, Rac & Ras C3d (complement bound to Ag) can bind to CR2 (which is part of the BCR) causing phosphorylation of the cytoplasmic tail = further activation! CD22 is activated by Ag bound to Ab sends transmembrane signal to an ITIM (inhibitory factor) making a phosphatase that cuts phosphates off of ITAM prevents further maturation Th cells are important in most B-cell responses. Signal 1 is sent by Ag binding Ag taken up by endocytosis Ag presented on MHC II / B7 is expressed Th2 cell recognizes MHC II bound antigen / costimulatory B7 binding to CD28 = Activation Activated Th2 cell makes CD40L which binds w/ CD40 on B cell = Signal 2 sent B cell making cytokine receptors cytokines made by Th cell (IL-2, IL-4, IL-5) push B cell to proliferate & differentiate Property Primary response Secondary response Responding B cell Naïve B cell Memory B cell Lag time after Ag administration 4-7 days 1-3 days Time of peak response 7-10 days 3-5 days Magnitude of peak Ab response Varies depending on Ag Generally 100-1000x higher than Primary response Isotype produced IgM predominates early IgG predominates Antigens TD & TI TD Ab affinity Lower Higher Lymph node-what is done where: Within cortex -- Primary follicle: B cell activation & Germinal center: B cell proliferation & differentiation. Paracortex: initial T cell and B cell activation. Medulla: Plasma cell secretion of Ab o Ag flows through lymph to lymph node either as free Ag or Ag bound to APC. Free Ag binds to follicular dendritic cells (in follicles & germinal centers), macrophages throughout lymph node, dendritic cells in the paracortex or B cells in the follicles & germinal centers Processed Ag presented to T and B cells that recognize each other at outside of the medulla then bind and move to germinal centers in germinal centers B cells (known as centrocytes) undergo affinity maturation that is mediated by somatic cell mutation, class switching also occurs B cells become plasma cells & exit germinal centers Somatic hypermutation occurs w/in VDJ region each time the cell divides as an activated B cell. This causes changes in the affinity for Ag = affinity maturation. If less affinity, Ab doesn’t bind Ag well apop. If better affinity between Ab & Ag proliferation continues. Class switching. A mIgM bearing cell can either make secreted IgM or it can undergo class switching by recombining DNA. Exchanges occur in the constant region of the Ab molecule (IgMIgG; IgG IgE or IgA). It is driven by B/T cell interactions via the CD40/CD40L interaction and by specific cytokines produced by the T cell. Occurs in the germinal centers of lymph nodes. Ppl whose T cells don’t have CD40L can’t class switch = X-linked hyper-IgM syndrome, only IgM, no memory cells made. Cytokines are also imp. As Ab is made, it causes feedback inhibition of its own production. o Soluble Ab binds Ag preventing it from reaching membrane bound Ab on B cells. o Ag:Ab complexes bind to Fc receptor molecules on the surface of the B cells making it more likely that CD22 down-regulatory events will be triggered. Only a few CD22 molecules are on each cell, there are many molecules of Ab when a lot of Abs are bound to Ag, the complex & CD22 find each other easily.