case
advertisement

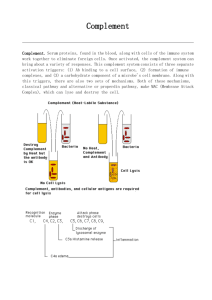
The Complement System Adapted from the Presentation of Jean F. Regal, Ph.D. Medical School - Duluth Learning Objectives Explain the importance of the complement system in host defense and inflammation and the clinical consequences of complement deficiencies. Describe the biochemistry of activation of the three different pathways including the initiators, sequence of reactions, important enzymes, and fragments. List the proteins which control the complement system and where they act. Describe the biological responses mediated by the different complement receptors. Describe the biological effects of complement activation. Megan Morris, age 5, is brought to your clinic by her mother, Mrs. Sarah Morris. Megan and her family have recently moved into your community and this is her first visit to see a physician in your community. Mrs. Morris has brought Megan to your clinic because Megan has been crying off-and-on since yesterday. Megan is cuddled tightly to her mother. 1. Why would a 5 year-old child cry so much? 2. What questions would you wish to ask the child and/or the mother? In answer to your questions, Mrs. Morris indicates that, yesterday evening, Megan began crying and saying that her face hurt. Mrs. Morris indicates that this was an unusual behavior, as Megan is usually a happy child who rarely cries. This morning, Mrs. Morris noticed that Megan’s face was swollen. Initially, she thought that the facial swelling might have been from Megan’s crying. However, it seemed to be too great an amount of swelling for that to have been the cause. 1. What additional questions would you wish to ask the child and/or the mother? At first, Mrs. Morris says that nothing like this has ever happened to Megan before. Then, as she continues to think about your question, she mentions that Megan did have some pain and swelling on her left hand about a year ago but that the swelling was mild. At the time, Mrs. Morris thought that Megan might have been bitten on the left hand by a mosquito, or was stung by a bee or other insect. The swelling went away overnight while Megan slept. Mrs. Morris asks if this past event was related to what is happening now to Megan. 1. What would you say to Mrs. Morris? 2. What additional questions would you wish to ask the child and/or the mother? This is Megan’s appearance, after you ask her to look toward you. 1. What do you note about Megan’s appearance? 2. What additional questions would you wish to ask Megan and her mom? Megan Morris Considering that Megan has a lot of swelling, she may have diminished kidney function or reduced liver function. However, the swelling seems to be limited to Megan’s face, reducing the likelihood of a systemic problem. It appears that there is a local problem that has developed. Complement: Location of Complement Proteins Complement is not a single protein but a complex of proteins that are found constitutively in the plasma. Complement proteins are present in secretions, such as bronchial fluids, where they protect portals of entry. Complement proteins are present in interstitial fluids where they protect against agents that penetrate the protective barriers (skin, mucosal membranes, etc.). Production of Complement Proteins The molecular weights of complement proteins range widely from 24-400 kDa. Complement proteins are synthesized Primarily by liver hepatocytes and by tissue macrophages, Secondarily by epithelial cells, fibroblasts and monocytes. Concentration ranges in plasma: 1 or 2 ug/ml – Mannose-Binding Lectin and Factor D 300 ug/ml – C4 1200 ug/ml – C3 Roles of Complement Complement proteins are activated on demand. Complement proteins are activated in a cascade. In these ways, complement proteins are similar to clotting proteins. Complement proteins are non-specific proteins that play roles both in the innate immune system and in the adaptive immune system. Destroy bacteria Destroy fungi Destroy viruses Importance of Complement The complement system is so important to our defense against microorganisms that there are several pathways by which the complement system can be activated. Classical pathway Alternative pathway Mannose-binding lectin pathway (aka, lectin pathway) Nomenclature of Complement Proteins Complement proteins in the common portions of the Classical Pathway are Denoted with the letter “C” followed by a number and are named C1 through C9. Proteins in the Mannose-Binding Lectin Pathway are Mannan-binding lectin (MBL) MBL-associated serine protease-1 (MASP-1) MBL-associated serine protease-2 (MASP-2) Proteins in the Alternative Pathway that lead to the common portions of the classical complement pathway are Denoted as factors (Factor B and Factor D). Function of the Complement System The complement system acts as an auxiliary system in immunity, both on its own and in conjunction with humoral immunity. In its role in innate immunity, it is a primitive surveillance and defense system for microbes, independent of T cells and antibodies. In its role in adaptive immunity, it is a major effector system for humoral immunity. Specific Functions of the Complement System Chemotactic Agent Activator of Inflammation Complement also augments stimulation of B cells through complement receptor 2 (CR2/CD21) to increase the humoral immune response. Activation of the Classical Pathway Activators Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign Surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activation of C1 C1 is present in plasma as an inactive C1qr2s2 complex Binding of two arms of the complex to immunoglobulin (2 IgG or 1 pentameric IgM) causes conformational change in C1q. This initiates a cascade of events. C1q conformational change C1r conformational change C1r conformational change C1r active enzyme C1r active enzyme C1s enzymatic cleavage C1s enzymatic cleavage C1s active enzyme C1s active enzyme C4 cleavage This result of this cascade is often referred to as the C1 esterase cleavage of C4. Cleavage of C4 is controlled by the C1 inhibitor (C1INH) The absence or mutation of C1 inhibitor leads to hereditary angioedema (swelling of the face and respiratory airways, as well as abdominal cramps). 2 IgG/1 IgM C1q C1q C1r C1r C1s C1s C4 C4b Italics = conformational change Color = enzyme activity Activation of C1 C1 esterase Activation of C4 C1 esterase cleaves C4. C4a can act a chemoattractant C4b has a thioester region which forms covalent bonds with molecules on the target surface. C4b can act as an opsonin and interacts with complement receptors (CR1). Activation of C2 C2 interacts with C4b and is cleaved by C1s, forming a C4b2a complex on the surface. C4b2a is the classical pathway’s C3 convertase. Thus, C4b2a is an enzyme that cleaves C3 to C3a and C3b. Note: There is some disagreement among scientists about the nomenclature for the cleavage products for C2. For example, some scientists identify the C3 convertase as the C4b2b complex. C3 activation C4b2a cleaves C3, activating a labile thioester bond on C3b. This thioester can bind COVALENTLY to free hydroxyl or amino groups, resulting in C3b covalently binding to target surfaces. C3b bound to a surface acts as an opsonin. Key points for the classical pathway Activation occurs in conjunction with specific antibody C3b and C4b covalently bind to target via thioester bonds Because there is a series of enzymatic cleavage events, there is tremendous amplification of the signal as the signal progresses down the series. Review of Activation of the Classical Pathway The sequence of complement protein activation in the classical pathway is 1>4>2>3>5>6>7>8>9 Note that 4b gets “before (b 4)” its expected place. The classical pathway is triggered by antigen binding to (crosslinking) two IgG molecules or two subunit parts of one IgM molecule. The cascade of proteolytic steps in the classical pathway are performed by serine esterases. C4b and C3b bind covalently to surfaces via thioester bonds. Sequential Enzymatic Cleavage Events in Complement Activation Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 Enzymatic Cleavage Events C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activation through C5 Involves proteolytic cleavage steps, liberating smaller fragments from C2 through C5. The smaller fragments are soluble and can have biologic effects. The larger fragments remain bound in a complex required for the next activation step. By convention, Smaller fragments are denoted by the letter ‘a’ (e.g., C3a, C5a) Larger fragments by ‘b’ (e.g., C3b, C5b) Notable exception is C2 (C2a is the larger, active fragment). Complexes with enzymatic activity are often denoted by a line over the top of the numbers or letters, as in • (C4b2a) Activation of the Mannose-Binding Pathway MBL Pathway Activation of the MBL Pathway is primarily mediated by a protein constituent in the plasma called mannan-binding lectin (also called the mannose-binding lectin or MBL). Activation of the MBL Pathway does not require specific antibody for activation. Activation of the MBL Pathway occurs by a C1-independent mechanism. Activation of the MBL pathway occurs when MBL binds to specific sugar residues like N-acetyl glucosamine or mannose that are present in the cell wall polysaccharides of microorganisms such as Salmonella, Listeria, Neisseria, Candida, etc. MBL, which resembles C1q, interacts with MASP-1 and MASP-2 by a mechanism similar to C1q interaction with C1r and C1s, resulting in the formation of the classical pathway C3 convertase (C4b2a). Activators Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign Surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activation of the Alternative Pathway Alternative Pathway Phylogenetically the oldest of the C3 activating pathways. Does not require specific antibody/antigen binding for activation. Can be triggered by a low level of spontaneous lysis of C3 by water to C3i that functions in a manner similar to C3b. Can be amplified by C3b binding to foreign surface structures (LPS) or by additional cleavage by bacterial proteases. Some Initiators or Activators of the Alternative Pathway of Complement Activation Many Gram-negative and Gram-positive bacteria LPS from Gram-negative bacteria Teichoic acid from Gram-positive cell walls Fungal and yeast cell walls (zymosan) Some viruses and virus-infected cells Some tumor cells Some parasites Human IgA, IgG and IgE in complexes Anionic polymers (dextran sulfate) Pure carbohydrates (agarose, inulin) Activators Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign Surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex C5a (Anaphylatoxins) Formation of the Alternative Pathway C3 Convertase (C3bBb) C3 tickover - spontaneous conformational change of a few C3 molecules, leading to water hydrolyzing the thiolester bond of C3 to form C3 H20 or C3i. C3i is then deposited in a random and non-specific manner on the surfaces of host cells and pathogenic organisms alike. On the normal host cell, bound C3i can inactivated by binding to Factor I and Factor H. On the pathogenic organism, bound C3i can be further activated by binding to Factor B to form C3iB which is then cleaved by Factor D to form C3iBb (C3 convertase). Properdin acts to stabilize the alternative pathway C3 convertase (C3bBb) Surfaces rich in carbohydrate and deficient in sialic acid tend to be the best activators. Activation and Inactivation of C3b C3 = Complement C3 FB = Factor B FD = Factor D FI = Factor I (in conjuction with Factor H, inactivates soluble C3b and C4b when deposited on the surface of a normal cell) FH = Factor H (cofactor of Factor I in mediating cleavage of C3b to its inactive form C3bi aka C3i Stablized by properdin Target Cell Membrane Normal Cell Membrane Amplification of C3 Cleavage by Membrane-Bound C3bBb Activation of C5 and the Terminal Complement Pathway C5 is cleaved by either the Classical Pathway C5 convertase (C4b2aC3b) or by the Alternative Pathway C5 convertase (C3bBbC3b) into 2 fragments: C5a and C5b. Cleavage of C5 is the last enzymatic step C5b binds to a target and then interacts with C6, C7, C8 and C9 to form the Membrane Attack Complex in the lipid membrane. The Membrane Attack Complex forms a transmembrane channel that allows passage of ions, compromises of the semi-permeable membrane, and causes lysis of the cell. Activation of C5 C5 is cleaved into 2 fragments (C5a and C5b) by either The Alternative Pathway C5 convertase (C3bBbC3b) or The Classical/Lectin Pathway C5 convertase (C4b2aC3b). Cleavage of C5 is the last enzymatic step. Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) (Anaphylatoxins) C5a C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex Non-Cleavage Events Involved in MAC Assembly Non-Cleavage Events in Assembly of the Membrane Attack Complex C5b then interacts with C6, C7, and C8. Lysis can occur in the absence of binding of C9 but it is slower. Activators Complement Sensors Classical Pathway Lectin Pathway Alternative Pathway Antigen Antibody Complexes (IgG/IgM) Polysaccharides on Microbes; Also IgA Foreign surfaces (LPS); Spontaneous (Nucleophiles) C1q MBL MASP-1, MASP-2 C1r2 C1s2 C3 + H2O Factor B Factor D C4 C2 C3 C3 convertase (C4b2a) C3b (Opsonin) C3a C5 convertase (C4b2a3b) (Anaphylatoxins) C5a C5 Terminal lytic Pathway C5b C6 C7 C8 C9 Membrane Attack Complex Punches Hole in Bacterial or Viral Membrane Assembly of C9 Channel If C9 molecules are bound to the C5bC6C7C8 complex, they form the Membrane Attack Complex that can punch a hole in the lipid membrane. Since the Membrane Attack Complex is a transmembrane channel that allows passage of ions, it will compromise the semi-permeability of the membrane and result in lysis of the cell. Notes on C9 Assembly If the interaction with C5b through C9 occurs in proximity to a membrane, then the MAC assembly occurs in that membrane and lysis is the end result. Alternatively, C5b-9 can bind to S protein in the fluid phase. In this case, lysis does not occur. Summary of Pathways of Activation Three Primary Pathways of Activation with different start signals Classical – antigen antibody Mannose binding lectin - mannose Alternative – LPS, carbohydrates, etc Proteolytic cleavages of complement components operate through C5 Non-proteolytic events for assembly of C6789 membrane attack complex Summary of Names You Need to Know Classical Pathway: C1q, C1r, C1s, C4, C2 Mannose Binding lectin pathway: MBL (mannose binding lectin) MASP-1 (MBL-associated serine protease) MASP-2 Alternative Pathway: Factor B Factor D Properdin Common to all pathways: C3 Terminal Lytic pathway: C5, C6, C7, C8, C9 Control What stops the activation? Or Why don’t we lyse all of our own cells? Things That Limit Complement Activation Short half life of the enzymes formed Properties of non-activator surfaces Inhibitors Fluid phase inhibitors • So active fragments don’t go too far Membrane bound inhibitors • On our own membranes • So C3b and C4b don’t attach or don’t lead to lysis of our own cells Activation and Inactivation of C3b C3 = Complement C3 FB = Factor B FD = Factor D FI = Factor I ( inconjuction with Factor H, inactivates soluble C3b and C4b when deposited on the surface of a normal cell) FH = Factor H (cofactor of Factor I in mediating cleavage of C3b to its inactive form C3bi aka C3i Stablized by properdin Target Cell Membrane Normal Cell Membrane Modes of Action of Complement Control Proteins Control Protein Main Site of Action C4 Activation – Classical Pathway C1-INH Plasma Formation of the membrane attack complex S Protein Plasma CD59 or HRF (homologous restriction factor) C3 and C5 Activation Factor H C4bp CR1 c Self membranes (wide tissue distribution) Plasma and nonactivator membranes Plasma c Self membranes (restricted tissue distribution) c Self membranes (wide tissue distribution) c Self membranes (wide tissue distribution Mode of Action Binds covalently to active C1s and C1r so C4 is not cleaved Binds to soluble C5b-7 and blocks its integration into membranes Inhibits binding of C9 and its polymerization Decay Acceleration of a Convertases C3b,Bb C4b,2a + - Cofactor Activity C3b C4b + - + + + + b + + MCP (Membrane + + cofactor protein) DAF or CD55 + + (Decay accelerating factor) a Decay acceleration is the ability to dissociate the C3 convertases C3b, Bb or C4b,2a. b Cofactor activity for the cleavage of C3b or C4b by factor I. C In this context, “self” stands for “within the same species.” Control proteins are mostly inactive for complement of other species. What If You Lack Control? Deficiencies of complement control proteins can lead to uncontrolled activation of the complement system Consequences of activation – lysis, etc Consumption (exhaustion) of the complement components can lead to the consequences of secondary complement deficiency (immunecomplex disease and infections) C1 Inhibitor Deficiency Roles of the C1 inhibitor Inhibits C1 esterase Also inhibits kallikrein, plasmin, Factor XIa and Factor XIIa Deficiency in C1 inhibitor leads to recurrent episodes of localized edema in skin, GI tract, or larynx Results in HAE (hereditary angioedema) Prevalence: 2-10 per 100,000 Hereditary angioedema Megan Morris You suspect that Megan might have hereditary angioedema due to a deficiency of C1 inhibitor. Analysis of her blood confirms C1 inhibitor deficiency. Several treatment options are available. Treatment with anabolic steroids to increase synthesis of C1 inhibitor Injections with purified C1 inhibitor You begin Megan on a regularly scheduled inoculation schedule for C1 inhibitor injections. Deficiency in Decay Accelerating Factor (CD55) & CD59 DAF deficiency causes increased susceptibility of erythrocytes to membrane attack complex-mediated lysis See as complement-mediated intravascular hemolysis in paroxysmal nocturnal hemoglobinuria (PNH) DAF deficiency is due to a defect in a posttranslational modification of the peptide anchors that bind the proteins to the cell membrane Recent studies suggest that DAF deficiency can be treated with an antibody to C5 reduces hemolysis What If You Lack a Complement Protein? Review: What does complement do? Lyses cells (MAC) Inflammatory mediators (C3a, C5a) Opsonization Solubilization and clearance of immune complexes Augmentation of humoral immunity Review: What does complement do? Lyses cells (MAC) Inflammatory mediators (C3a, C5a) Opsonization Solubilization and clearance of immune complexes Augmentation of humoral immunity Anaphylatoxins C3a C3a receptor Response C5a C5a receptor Response C3a and C5a can mimic the symptoms of inflammation and anaphylaxis Chemotaxis, smooth muscle contraction, increased vascular permeability, degranulation of mast cells, etc. Distinct receptors on many cell types Anaphylatoxin Receptors CD88 Review: What does complement do? Lyses cells (MAC) Inflammatory mediators (C3a, C5a) Opsonization Solubilization and clearance of immune complexes Augmentation of humoral immunity Things C4b and C3b can do Complement Activation C4b and/or C3b on surfaces Participate in continued pathway activation leading to MAC Interact with CR1 Degraded to fragments Interact with CR2 and CR3 Lysis Opsonization Clearance of IC Opsonization Clearance of IC Augmentation of humoral immunity CR1 (CD35) Major ligands C3b, C4b Monocytes, macrophages, PMN, Eosinophil, RBC, B and T cells Transport of immune complexes by RBC Promotes immune adherence (binding of opsonized microbes to primate RBCs) Promotes phagocytosis in cooperation with Fc receptors Blocks formation of C3 convertase Complement Receptors Receptor Major Ligands CR1 (CD35) C3b, C4b CR2 (CD21) C3d, C3dg, iC3b CR3 (CD11b/CD18) CR4 (CD11c/CD18) iC3b Activity Cellular distribution Blocks formation of C3 convertase; Binds immune complexes to cells RBC, PMN, monocyte, macrophage, eos, follicular DC, B cell, some T cells B cell co-receptor Binds EBV B cells, follicular DC, some T cells Cell adhesion Binds immune complexes Monocytes, macrophages, neutrophils, NK, some T cells Review: What does complement do? Lyses cells (MAC) Inflammatory mediators (C3a, C5a) Opsonization Solubilization and clearance of immune complexes Augmentation of humoral immunity C3 fragment interaction with Complement Receptors Bacteria or IC Clearance of Immune Complex Augments humoral immunity Immune Complex Disease High incidence of Immune Complex disease in individuals who are deficient in C1, C4, C2 or C3 Immune complexes are not solubilized and cleared Complement can also play a significant role in tissue damage in Immune Complex diseases such as SLE (systemic lupus erythematosus) Excess immune complexes cause pathological complement activation inflammation, tissue damage Immune Complex Solubilization And Transport Complement prevents formation of insoluble immune complexes (solubilization). Deposition of insoluble aggregates in the tissues can cause damage and immune complex disease. Binding of C3b to the antigen antibody complex interferes with lattice formation, limits its growth, prevents precipitation of the antigen antibody complexes and keeps them soluble. Immune complex transport The complement system is a major mechanism for removal of immune complexes (transport). Immune complexes coated with C3b bind to CR1. More than 85% of the CR1 in the circulation is on the RBC. CR1 receptors on the erythrocyte are responsible for the transport of immune complexes to the reticuloendothelial system for clearance (macrophages in spleen, etc). The immune complex coated with C3b is transferred from the RBC CR1 receptor to the macrophage CR1 receptor. The immune complex is then internalized and degraded. Review: What does complement do? Lyses cells (MAC) Inflammatory mediators (C3a, C5a) Opsonization Solubilization and clearance of immune complexes Augmentation of humoral immunity CR2 (CD21) Major ligands C3d, C3dg, iC3b B cells, activated T cells, epithelial cells CR2 forms an additional signal with antibody to augment stimulation of the B cell to increase the humoral immune response (CR2/CD19/CD81). CR2 has high affinity for an envelope protein of Epstein Barr virus, allowing the virus to enter the B cell. Complement Deficiencies Deficiencies of the various complement components often present as infections Pyogenic infections and infections with encapsulated bacteria (classical and alternative) Opsonization and phagocytosis are a primary host defense. Neisseria infections (C3, alternative pathway and terminal lytic pathway) Immune complex or autoimmune disease Classical pathway or C3 deficiencies Complement Deficiencies and Associated Diseases Component Classical pathway C1q C1r or C1s C4 C2 MBL pathway MBL MASP-2 C3 and alternative pathway C3 B D Properdin I H Number of cases or Incidence 41 19 26 IC Diseasea High incidence 1:10,000-1:20,000 2-7% UK population 9 Caucasians Undefined 27 1 <10 Glomerulonephritis>SLE - >100 - 31 22b 1 HUSc Membrane attack complex C5 30e e C6 80 e C7 70 e C8 70 C9 1:1000 a IC disease, SLE, SLE-like syndromes, glomerulonephritis, vasculitis. c HUS, Hemolytic uremic syndrome. e Higher incidence in Japanese (0.001-0.004%) Infections Encapsulated bacterial infections or pyogenic infections Increased susceptibility to bacterial infection Undefined Pyogenic and Neisseria Meningococcal infection Meningococcal and encapsulated bacterial infection Meningococcal infection Encapsulated bacterial infection Meningococcal infection Meningococcal infection Meningococcal infection Meningococcal infection Meningococcal infection Factor H is One Fluid Phase Inhibitor of C3 Convertase • Factor H is a fluid phase inhibitor of C3 convertase. If it sees C3bBb floating around, it binds and dissociates the Bb, thus inactivating the C3bBb. ‘Decay acceleration of the convertase’ Factor H Can Inactivate C3bBb on the Surface of a Normal Cell • If Factor H sees C3bBb on a membrane with sialic acid (like our membranes), it will bind to the sialic acid residue and C3b, displacing Bb from the convertase and inactivating C3bBb. Factor I than can degrade the C3b, with Factor H as a cofactor. • An activator surface (such as bacteria) does not have sialic acid and therefore Factor H cannot bind and displace the Bb. In this case, the Factor H does not inhibit the C3 convertase activity.