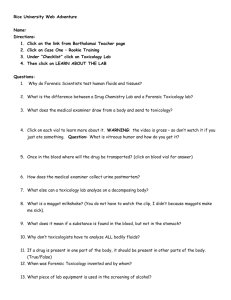
Approach to Self poisoning
advertisement

General Approach to the Toxicology Patient Risk/Benefit + Evidence =Practice Andrew Dawson NSW Poisons Information Centre Royal Prince Alfred Hospital SACTRC Case 1…Late one 1992 night The phone rings. A doctor informs us that they have just ceased resuscitating a 14 year old girl who presented following a chloroquine overdose. He asks, " if there was anything I could of done". We reply, "##@/etc there is little you can do now, because she is dead” South Asian Clinical Toxicology Research Collaboration Take home messages • Poisons are simple • Patients are complicated • Toxicology Care is mostly supportive • When you don’t know…….phone a friend Understand the Mechanism Overview • Epidemiology • Clinical Approach – Important Poisonings • Red Flag messages What do the patients look like? • 300 presentations /per year/ 100,000 – 10% ICU – 20% repeat within a year • Previous sexual assault • 70% women • 30% men • Drug and alcohol • Psychiatric • Social issues Drug Deaths? • Death is Rare < 0.5% • Psychiatric drugs are now designed for overdose • Cardiovascular drugs are not designed for overdose • Verapamil, diltiazem,beta blockers, digoxin, antiarrythmics • Cellular Poisons (colchicine, cyanide, paracetamol, metals) • Medical complications • Pulmonary Embolus, aspiration • Cardiac and CNS Toxicity pharmaceutical toxicity Extension of its therapeutic effect – + Additional toxic effects – Variation within a pharmaceutical class Rapid onset is the rule – EXCEPT Controlled Release Drugs Cellular poisons eg paracetamol • • Risk Assessment Overdose • Patient – – – – Dose Time Pre-existing illness Signs of toxicity • Vital signs • Examination • Simple tests • Doctor – Is this toxicity • Prior knowledge • Authoritative information • 131126 Effect Concentration Where on the curve are we? • Assess risk • Resuscitate • ? Specific Treatment • ? Decontaminate Time Clinical Risk Assessment • Cardiovasular – Pulse & BP • Airway and Oxygenation • Neurological – Level of consciousness – Reflexes • Investigations – ECG – Blood gases – Glucose – Specific assays Time Effect Concentration Volume, Pressor or Inotrope ? Many agents have myocardial depressant and peripheral vasodilatory effects In severe poisoning: EARLY assessment of myocardial function important ECG – is there QRS widening? Na+ channel toxicity Bed-side ECHO Cardiac output assessment – PICO QRS prolongation – Bicarb and Hypertonic Saline LOW CO = inotropes LOW SVR = pressors South Asian Clinical Toxicology Research Collaboration Normal Repolarization Na Ca K K +30 mV Ventricular Myocyte / Purkinje Cell Action Potential -40 mV Absolute Refractory Period -70 mV -90 mV Corresponding ECG Waves Relative Refractory Period P PR QRS T ST Segments QT What do gases tell us? • ? CO2 • ? O2 • Acid Base • Lactate: explain ?anion gap (in mmol/L) = (Na+ K) - (HCO3 + Cl) MUDPILES methanol, uremia, diabetic ketoacidosis, propylene glycol, isoniazid, lactic acidosis, ethylene glycol, salicylates Benzyl alcohol Beta-adrenergic agents Caffeine Carbon monoxide Cyanide Ethanol Ethylene glycol Hydrogen sulfide Ibuprofen Iron Isoniazid (INH) Lithium Metformin Methanol Paracetamol Paraldehyde Phenformin Salicylates Strychnine Sympathomimetic amines Toluene Psychiatry Pre 1950 • • • • • • • • • Opium Bromides Barbiturates Hysocine Paraldehyde Antihistamines Benzedrine Amphetamine Thyroxine Psychotic patient 1932 Promethazine 1950 Chlorpromazine 1954 Imipramine 1971 Clozapine 1980 Olanzapine 1972 Fluoxetine 1990 Quetiapine 1993 Venlafaxine If the ECG is important….. Is man smarter than a machine? Is it NormalMachine ? reading QTc 430ms Hand-measurement and QTc by Bazett formula 640ms The Next Minute - Tdp • Measure manually • 3 limb leads • (I, II, and one other) • 3 Chest leads • V2, V4, and V6 • Use QT not QTc "not all QT prolongation is equal" Acquired long QT Important List (5A + CLAM) • Antiarrhythmia • Antidepressants • Antipsychotic • Antihistamine • Antimicrobial • Macrolides, Antifungal • Others (CLAM) • Cisapride / Cesium, Li, Arsenic Trioxide, Methadone Extensive List : www.qtdrugs.org What? If the QRS>100msec suspect Na Channel block I S in I, aVL aVR Sinus Tachycardia Response to NaHCO3 QRS 190ms TCA: pH = 7.1 TCA: pH= 7.3 • 200 mEq bicarbona te TCA: pH =7.4 • 200 mEq bicarbonat e Altering Ionization HA + H +A Equilibrium influenced by external pH The balance of the equilibrium can be expressed by pKa The pKa is the pH where [ionized] = [unionized] South Asian Clinical Toxicology Research Collaboration QRS 126 ms Bicarbonate / Alkalinisation: pH manipulation Indications Should be trialled in any broad complex rhythm associated with poisoning South Asian Clinical Toxicology Research Collaboration Bicarbonate / Alkalinisation Indications Tricyclic antidepressants & Phenothiazines Chloroquine Antiarrythmics Cocaine Calcium Channel Blockers ? Organophosphates Dose 1-2 meq/kg in repeated bolus doses Titrated ECG Target pH 7.5-7.55 South Asian Clinical Toxicology Research Collaboration Case 2 • 15 year old boy • Took 80 x 40 mg propranolol at a bus stop and called ambulance 5 mins later • On ambulance arrival; he had recurrent seizures, GCS 3. • Ensuing bradycardia and lost output enroute to hospital – CPR commenced • Broad idioventricular rhythm on arrival Thoughts/Risk assessment • 15 y.o. – assume adult weight • >40 mg/kg dose – toxic dose? • Is clinical course described expected for propanolol toxidrome? • What immediate adjuncts to ALS can be offered Initial measures • RESUSICTAION • Secure airway • Bicarbonate • Hyperventilate • 2mmol/kg initally • Establish further access • 1-2mmol/kg bolus every 3-5 mins • Cont PALS algorithm • Atropine • 0.5 – 1.5 mg IV • Titrated to ECG • Target pH 7.55, Na <160 Healthy Myocardial Metabolism Myocardial metabolism under normal conditions Stores of ATP in myocardium are low Oxidative metabolism Citric acid cycle Primarily FFA (80%) + carbohydrates (15%) = 95% FFA 80% at rest – more ATP produced but more O2 needed ATP production 30 moles per mole of glucose South Asian Clinical Toxicology Research Collaboration Hantson P Clinical Toxicology (2012), 50, 166–171 Stressed Myocardial Metabolism Myocardial depression Reduced BP, reduced O2 delivery Increased endogenous CCA release Increased glycogenolysis and hyperglycemia Increased lipolysis Inhibition of insulin secretion Decreased sensitivity of tissues to insulin Reduced myocardial FFA uptake and oxidation Reliance on anaerobic glycolysis for energy effective ATP production – 2 moles per mole of glucose Less South Asian Clinical Toxicology Research Collaboration Anaerobic glycolysis High-dose Insulin-Euglycaemia - HIE HIE Myocardial energy normally derived from FFAs In shock states energy derived from glucose CCB poisoning inhibits pancreatic insulin secretion BBs reduce myocardial FFA uptake and transfer to mitochondria Insulin thought to Improve delivery of glucose to myocardium Improve coronary blood flow, contractility Increase lactate uptake Improve Ca flux into myocardial cells May have direct inotropic effect in high doses South Asian Clinical Toxicology Research Collaboration HIE Onset of effect delayed by 15 to 60 minutes Probably should be commenced sooner rather than later with other inotropic agents Insulin dose No studies to determine optimal dose Most cases use 0.5-1.0 U/kg loading and 0.5 to 1.0 U/kg/h Reports of up to 10 U/kg/h Glucose Usually already elevated Bolus dose 25 g + infusion to maintain BSL 6 -14 mmol/L Potassium Will fall – suggested to replace if < 2.5 mmol/L South Asian Clinical Toxicology Research Collaboration 2hrs later…. • Successful return of output at 30mins • What about decontamination • Remains hypotensive • Ongoing therapies • Inotropes vs HIET • Then he has a further seizure Case 3 • 22 y.o. female (wt 50kg) • Ingests 90 x 500mg paracetamol (standard release prep) at 2030 • Empty 2L cask of wine found on the counter • Presents to hospital at 2330; drowsy and confused • Initial Vital Signs HR 110, BP 100/60, RR 18, afebrile Sats 98% RA, GCS 11 • Further History • Presented with a paracetamol overdose 5 days prior. Level found to be non-toxic. Did not receive any further treatment or follow up. • No other medications found on premises Assay Level Assay Level Paracetamol Na+ 140 ALT 3000 (micromol/L) 57 K+ 4.1 AST 60 Creat 59 INR 1.4 BAL 0.08% paO2 130 pCO2 30 HCO3 18 pH 7.1 Risk Assessment • Significant toxicity • Decontamination? • Airway protection • Appropriate NAC regimen • Commence on arrival vs wait for level Gastrointestinal Decontamination don’t confuse mess with efficacy Gastrointestinal Decontamination • • • • • Nothing Emesis Efficacy decreases with time Gastric Lavage Rarely indicated routinely Or after 2 hours Activated Charcoal UNLESS massive ingestions Whole bowel irrigation Other thoughts • Cause for reduced level of consciousness? • Alcohol intoxication • Related to paracetamol alone • Other co-ingestant • Cause for early acidosis? • Liver failure • Co-ingestants • Effect of toxic paracetamol level? Late one 1992 night The phone rings. A doctor informs us that they have just ceased resuscitating a 14 year old girl who presented following a chloroquine overdose. He asks, " if there was anything I could of done". We reply, "##@/etc there is little you can do now, because she is dead” South Asian Clinical Toxicology Research Collaboration Case 1…Late one 1992 night The phone rings. A doctor informs us that they have just ceased resuscitating a 14 year old girl who presented following a chloroquine overdose. He asks, " if there was anything I could of done". We reply, "##@/etc there is little you can do now, because she is dead” South Asian Clinical Toxicology Research Collaboration The question is: When faced with an unknown toxic cardiovascular surprise what interventions would we think of using before we would cease resuscitation? Can we develop a mnemonic? If we have a mnemonic will we get air tickets to exotic locations to use it? We decide to use the alphabet to identify antidotes South Asian Clinical Toxicology Research Collaboration The Toxic CVS mnemonic A B C D E F G H I J K L M N O P South Asian Clinical Toxicology Research Collaboration The Toxic CVS mnemonic Atropine Bicarbonate Calcium Diazepam Epinephrine Extracorporal Fab Antibodies Glucose Glucagon Human Insulin Euglycaemia Joules K potassium Lipids?? Magnesium N Oxygen Phone a friend South Asian Clinical Toxicology Research Collaboration A DRUG INDICATION DOSE Atropine Vagal 0.6 - 1.2mgs Organophosphates 50-100mgs B Bicarbonate Alkalinsation Tricyclic, Antipsychotics, Cocaine, Verapamil 1-2 meq/kg in repeated bolus doses. Target pH 7.5-7.55 C Calcium Chloride/ Gluconate Calcium Channel Blockers 1 gram bolus repeated every 3 minutes. Target calcium double normal level D Diazepam Chloroquine Cocaine & Amphetamine Up to 3 mgs/kg in chloroquine, unitl sedated in cocaine E Epinephrine & Inotropics Chloroquine F Fab Antibodies Digoxin & Cardiac Glycosides Dose based on ingestion or concentration or titrated against effect G Glucagon Beta Blockers,Calcium Channel Blockers 5-10 mgs IVI stat then infusion if response HI Human Insulin Euglycaemia Calcium Channel Blockers, Beta Blockers 0.5 us/kg plus glucose see protocol South Asian Clinical Toxicology Research Collaboration Red Flags • All slow, extended or control release drugs are TOXIC • Delayed onset of action • Vital signs are vital • Change because of ongoing absorption • Man is smarter than the machine • Measure the ECG • When in doubt…phone a friend