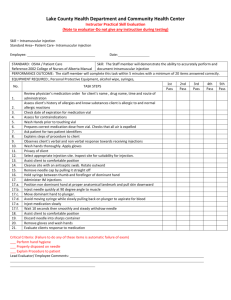
Pediatric medication adminsrtration
advertisement

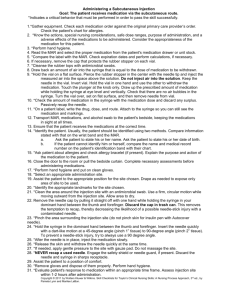
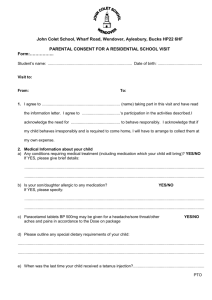
Prepared by: Dr. Salma Elgazzar Physiologic differences make children more sensitive to drugs and more at risk for adverse drug reactions. Pharmacokinetics and pharmacodynamics are affected by changes in body fluid composition, differences in the cardiovascular, GIT, renal, and neurological systems. PHYSIOLOGIC DIFFERENCES Physiologic differences between children and adults Infants have immature kidneys and liver delays metabolism and elimination of many drugs. Slow gastric emptying time and decreased gastric acid secretion may delay absorption. Infants have lower concentration of plasma proteins, therefore toxicity can occur with drugs that need to be bound to proteins. Infants have less total body fat and more total body water. Therefore, lipid soluble drugs require smaller doses with less fat present, and water soluble drugs require larger dosages. As children grow, the changes in fat, muscle, body water, and organ maturity will alter the pharmacokinetics of drugs. Oral Rectal Ophthalmic Otic Topcial Intramuscular Intravenous Be truthful Minimally threatening Use the 5 rights: pt, drug, dose, route, time. Discrepancies must be determined Lab results or levels may need to be consulted before administration. Do not use if child has vomiting, malabsorption or refusal. Dropper/oral syringe/teaspoon/cup/nipple Give small amounts down side of mouth in an infant Encourage swallowing with a pacifier in an infant. Crushed meds are put in a small amount of soft food: ice cream, apple-sauce, yogurt; must take it all. Do not mix meds with foods, or formula. Do not try to trick child; be honest. For liquid medications, an oral syringe or medication cup should be used to ensure accurate dosage measurement. Use of a household teaspoon or tablespoon may result in dosage error because they are inaccurate. •Depress the chin with the thumb to open infant’s mouth •Using the dropper or syringe, direct the medication toward the inner aspect of the infant’s cheek and release the flow of medication slowly. •Note: child’s hands are held by the nurse and child is held securely against the nurses body. Rarely used in the acute setting. Immunizations Antibiotics Use emla A local skin anaesthetic that is applied to the skin prior to procedures such as needles, to help prevent pain. IM INJECTION SITES Vastus Lateralis is the preferred site in young children Birth to 2yrs: vastus lateralis only Except: DTaP given IM in deltoid at 5yrs. Ventrogluteal site can be used if muscle is well developed and amount is 0.5-2ml. Gluteus maximus (dorsal gluteal site) must not be used in the child less than 1 yr or before the child has been walking for one year; but vastus lateralis is the preferred site. Largest muscle in infant / small child. 0.5 ml in infant 1 ml in toddler 2 ml in pre-school Use 5/8 to 1 inch (2.5 cm) needle Compress muscle tissue at upper aspect of thigh, pointing the nurse’s fingers toward the infant’s feet Needle is inserted at a 90-degree angle. Use ½ to 1 (2.5 cm) inch needle 0.5 to 1 ml injection volumes More rapid absorption than gluteal regions. Gluteal muscle does not develop until a child begins to walk; should be used for injections only after the child has been walking for a year or more ½ to 1 ½ inch needle 1.5 to 2 ml of injected volume. -IV route provides direct access into the vascular system. -Adverse effects of IV medication administration: • Extravasation of drug into surrounding tissue. • Immediate reaction to drug. -Check for compatibilities with IV solution and other IV medications. -Flush well between administration of incompatible drugs. -IV medications are usually diluted. -Infusion pumps are required -At least hourly fluid monitoring is required -Medication volume should not fluid overload the child. -Agency specific policies for IV medication administration -Given via peripheral or central line -If a maintenance IV isn’t running, the medication needs to be flushed with saline, before and after. -Central lines require a terminal flush with Heparin when no longer in use (SASH). IV push = directly into the tubing Syringe pump = continuous administration Buretrol = used to further dilute drug •Morphine •Solu-medrol •Lasix Drug that can safely be administered over 3 to 5 minutes. Accurate delivery system for administering very small volumes ICU NICU A buretrol or volutrol is an intravenous delivery device attached between the IV fluid bag and the intravenous catheter. It is used to deliver IV fluids in a safe manner to children and medications in some nursing units. Usual volume capacity is 150 ml. Some units have a policy that a buretrol will be used on all children under 10 kg while others may state 20 kg. Individual units vary on policy. Current theory is that buretrols should be used for children weighing <10-15 kg. A large bore catheter that are inserted either percutaneously or by cut down and advanced into the superior or inferior vena cava Umbilical line may be used in the neonate -Used for long term administration of meds -Used for chemotherapy -Total parental nutrition Central line equipment, in order of typical usage: 1. Syringe with local anesthetic 2. Scalpel in case venous cutdown is needed 3. Sterile gel for ultrasound guidance 4. Introducer needle (here 18 Ga) on syringe with saline to detect backflow of blood upon vein penetration 5. Guide wire 6. Tissue dilator 7. Indwelling catheter (here 16 Ga) 8. Additional fasteners, and corresponding surgical thread 9. Dressing Infiltration Catheter occlusion Air embolism Phlebitis Infection In children younger than age 3 years the pinna is pulled down and back to straighten the ear canal In the child older than 3 years, the pinna is pulled up and back. Instilling eye drops Room temp May need to wash eye Supine and look up Pull down lower lid Rest hand holding the dropper with the medication on the child’s forehead to reduce risk of trauma to the eye. Allow child to blink Dim lights allow child to open their eye more easily Act as vasoconstrictors excessive use may be harmful Discontinued after 72 hours Congested nose will impair infants ability to suck Give 20 minutes before feeding Have kleenex Keep child’s head below the level of shoulders for 1 to 2 minutes after instillation Position child with the head hyper extended to prevent strangling sensation caused by medication trickling into the throat. Usually sedatives and antiemetic Use little finger Insert beyond anal sphincter Apply pressure to anus by gently holding buttocks together until desire to expel subsides Vaccine Type BCG Live attenuated Bacteria DTP D&T = Toxoids Route Intradermal (preferred) Intramuscular P = inactivated bacteria Hepatitis B(HBV) Inactivated viral antigen Intramuscular Haemophilus Influenza b (Hib) Polysaccharide Intramuscular MMR Live attenuated viruses Subcutaneous