File - Kelly Marchant RN
advertisement

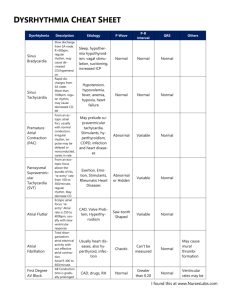
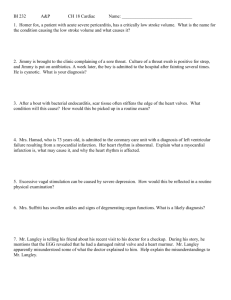
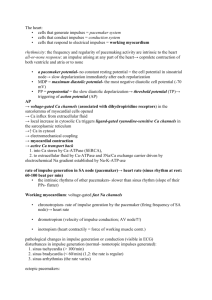
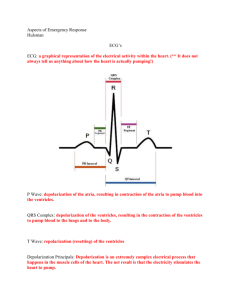
Cardiac Dysrhythmias Nuro 438 February 2015 Learning Objectives At the completion of this presentation, the nursing student will be able to successfully Describe cardiac anatomy and physiology Describe the function of the heart, including circulation and automaticity Describe and define the major cardiac waves in an EKG Define normal sinus rhythm Differentiate between rate, conduction, atrial, and ventricular arrhythmias Recognize life-threatening dysrhythmias Identify nursing considerations related to various cardiac dysrhythmias Differentiate types of medications to treat arrhythmias Identify risks for cardiac arrhythmias Identify adverse effects associated with cardiac dysrhythmias Analyze EKG Rhythm strips Cardiac Anatomy Cardiac Anatomy 4 Chambers, 2 Atria, 2 Ventricles 4 Valves Acts as a PUMP Receives deoxygenated blood from body, pumps to lungs Receives oxygenated blood from lungs, pumps to body Cardiac Circulation Cardiac Function Heart functions a pump to deliver blood to the body Automaticity Impulse Generation Under Usual circumstances Impulse generated from pacemaker cells in SA node Impulse then travels to AV node Impulse then travels to Bundle of His Impulse then travels to Right and Left Bundle Branches Impulse travels to Perkinje Cells that innervate ventricles Components of an EKG EKG Graph X Axis = time Y Axis = amplitude Displays electrical activity of heart Electrical impulse precedes contraction Depolarization and repolarization are depicted as waves Atrial Depolarization = P wave Atrial repolarization occurs during ventricular depolarization Ventricular depolarization = QRS complex Ventricular repolarization = T wave EKG Basics Bipolar lead: positive and negative electrode. Measures electrical potential between the electrodes AKA ‘Standard Limb Leads’ Leads I,II,III Used to monitor only for dysrhythmias Lead II most commonly used Telemetry Placement Red = Brake (right), Green = Gas (left) Smoke (black) over Fire (red), Snow (white) on the Trees (green) Stars and Stripes Lead II 12 Lead EKG 3 Standard (bipolar) Limb Leads 3 Augmented (unipolar) Leads (aVR, aVL, aVF) Triaxial reference- measures the difference in electrical potential between one of three extremity electrodes and the central terminal 6 Precordial (unipolar) Leads (V1, V2, V3, V4, V5, V6) aVR, aVL, aVF The V Leads Cardiac Waves The P wave Pacemaker is SA node, rate 60 - 100 Correlates with atrial depolarization (begins in SA node moves R-> L and down) PR interval 0.12-0.2 Determine atrial rate Compare atrial rate to ventricular rate The QRS Complex Represents normal depolarization of the ventricles Normal duration 0.06- 0.12 Measured from Q wave (first deviation from isoelectric line) to S wave (the return to isoelectric line) Abnormal QRS is abnormal depolarization BBB Ventricular pre-excitation Cardiac pacemaker The T Wave Represents Ventricular repolarization Occurs during end of ventricular systole Typically in same direction as QRS complex Lasts 0.10 – 0.25 U Wave Final stage of repolarization, thought to be repolarization of Perkinje Fibers Not usually seen May indicate Hypokalemia Cardiomyopathy LVH Dig toxicity EKG Paper At the 25 mm speed, Each mark at top is 3 seconds There are three large boxes between each mark Each large box is 1 second or 25 mm Each large box has 5 medium boxes in it Each medium box is 0.2 seconds or 5 mm Each medium box is made up of 5 small boxes (or dots) Each small box (dot) = 0.04 seconds or 1 mm EKG Paper Steps to Interpreting Cardiac Rhythms Determine the Heart Rate Determine the Regularity Identify and analyze P waves or flutter Determine PR interval and AV conduction Identify and analyze QRS complex Determine site of origin of dysrhythmia Identify dysrhythmia Evaluate significance of dysrhythmia Determine the Heart Rate The Six-second Method Most common/least accurate Simplest, quickest Heart Rate Calculator The Rule of 300 Must be regular R-R Interval Method Rhythm must be regular Distance between peaks of 2 R waves and /60 Describe the Rate & Rhythm Normal = 60-100 Tacchycardia >100 Bradycardia <60 Regular Irregular Regularly-irregular Sinus Arrhythmias ST = HR >100 SB = HR ,60 Steps to Interpreting Cardiac Rhythms Determine the Heart Rate Determine the Regularity Identify and analyze P waves or flutter Determine PR interval and AV conduction Identify and analyze QRS complex Determine site of origin of dysrhythmia Identify dysrhythmia Evaluate significance of dysrhythmia Measuring the Waves PR Interval Represents progression of electrical impulse from the SA node or an ectopic pacemaker (in atria or AV junction) through entire conduction system of the heart to the ventricular myocardium Normal duration 0.12 – 0.20 PR >0.20 represents delayed conduction of impulse Irregular P Wave Remember P wave represents atrial depolarization Irregular P represents altered, damaged, or abnormal atria Increased Right Atrial Pressure or hypertrophy as seen in COPD and CHF = tall peaked P wave Increased left atrial pressure or hypertrophy = wide notched P wave Ectopic P Wave Electrical impulse for ectopic P wave originated outside SA node or in AV junction Occur in PAC’s Atrial tacchycardia SVT PAC’s Premature Atrial Contraction P wave followed by normal QRS Generally followed by noncompensatory pause P waves vary, PR intervals normal AV Ratio 1:1 Conduction Causes of PAC’s Increased sympathetic tone Infection Emotional Stress Stimulants Medications; epinephrine Hypoxia Digitalis toxicity ACS or CHF QRS Complex Represents normal depolarization of the ventricles Onset is point where first wave (Q) deviates from isoelectric line End is where last wave (S) returns to isoelectric line Duration 0.06 – 0.12 Irregular QRS Represents abnormal depolarization of ventricles Irregular QRS present in Bundle Branch Block Ventricular preexcitation Cardiac pacemaker QT Interval Represents time it takes for ventricles to depolarize and repolarize Prolonged QT associated with pericarditis, myocarditis, MI, LVH, hypothermia, CVA, increased IC trauma or hemorrhage, medication SE, electrolyte imbalances (K, Ca), or liquid protein diets ST Segment Represents early part of repolarization of right and left ventricles Duration < 0.20 Normally ST segment is flat Elevation can be evidence of myocardial ischemia or infarction, coronary vasospasm, pericarditis, LBBB, LVH, raised ICP Steps to Interpreting Cardiac Rhythms Determine the Heart Rate Determine the Regularity Identify and analyze P waves or flutter Determine PR interval and AV conduction Identify and analyze QRS complex Determine site of origin of dysrhythmia Identify dysrhythmia Evaluate significance of dysrhythmia Arrhythmias Rate Arrhythmias Tachycardia Bradycardia Atrial Arrhythmias Afib/Aflutter WPW SVT Conduction Arrhythmias Bundle Branch Blocks AV Conduction Block (1st, 2nd, 3rd Degree) Life Threatening Arrhythmias V Fib Complete Heart Block Asystole Living Arrhythmias https://www.youtube.com/watch?v=TJR2AfxVHs M Atrial Arrhythmias Atrial Tacchycardia Atrial fibrilation Atrial flutter Supra Ventricular Tacchycardia Wolf-Parkinson-White 8 Steps ID P or F waves Conduction ratio, is every P followed by QRS Atrial Tachycardia Rate is usually 160-240 beats Type of SVT, where generation for impulse is outside SA node A Fib and Aflutter are most common forms P waves are uniform PR intervals are normal AV conduction is 1:1 Atrial Tachycardia Clinical significance Dependent on presence and extent of heart disease Palpitations, nervousness, anxiety Perfusion Syncope Workload of heart Nursing Assessment Atrial Tachycardia A Flutter Causes Cardiomyopathy Atrial dilation Valve Disease Thyrotoxicities Hypoxia CHF ETOH Abuse A Flutter Risks; Incomplete emptying of ventricles Thrombi formation Loss of atrial kick Syncope, hypotension CHF Treatments Beta Blockers CCB Digoxin Warfarin Cardioversion if uncontrolled Ablation Atrial Flutter Impulse generated by ectopic pacemaker or reentry pathway F waves have a saw-tooth appearance Rate; Atrial 240-360, Ventricular half the atrial rate Rate is regular Normal P waves absent Unable to measure PR intervals Expressed as ratio 4: 1 Flutter Atrial Fibrillation Atrial Rate 350-600 Ventricular rate < 100 = controlled, >100 = uncontrolled Irregularly irregular rate P waves absent, F waves absent Atrial Fib Causes and treatments similar to A Flutter SVT Rapid rhythm (>100) that generated outside the ventricles AKA Paroxysmal Atrial Tach (PAT) Symptoms Palpitations Lightheadedness Dizziness Maybe symptomless, self limiting Treatments Beta Blockers, CCB,antiarrhythmics SVT WPW Ventricular pre-excitation; early activation of ventricles by impulse that bypasses the AV node Impulse can be generated in accessory pathway or bypass tract that abnormally Most frequent AV bypass tract in WPW is Bundle of Kent Presence of Delta wave Wandering Atrial Pacemaker Dysrhythmia originating in multiple pacemaker sites that shift between SA node and AV junction Rate 60 – 100 Irregular P waves vary in size and shape PR intervals are normal to very short AV Conduction ratio 1:1 Wandering Atrial Pacemaker Conduction Arrhythmias Conduction Block/ AV Block Bundle Branch Block AV Blocks First Degree AV Block Second Degree Type I AV Block Second Degree Type II AV Block Third Degree AV Block First Degree AV Block Delay in conduction of electrical impulse, usually through the AV node Most common Heart Block Prolonged PR (> 0.20) Rate and Rhythm Regular AV Conduction 1:1 Causes 1* AV Block Acute Inferior Wall MI Ischemic Heart Disease Digitalis Toxicity Medications (B Blockers, CCB) Hyperkalemia First Degree AV Block Second Degree Type I AV Block AKA Wenckebach Usually temporary condition, and asymptomatic Prolonging PR form one QRS to the next until one QRS is not conducted or “dropped” then pattern starts over again P to P intervals are regular R to R intervals are irregular More P waves than QRS complexes Causes; Acute inerior wall MI, Ischemic heart disease, Dig Toxicity, BB, CCB, Hyperkalemia Second Degree AVB, Type I Second Degree Type II AV Block Dysrhythmia with constant P-R interval with missing QRS complexes Complete block of conduction in one bundle branch and an intermittent block in the other bundle branch Can present as pattern, ie 2:1 block or 3: 1 block OR without pattern of QRS/ unstable QRS Causes; Damage to Bundle Branches p MI, Very high potential to convert to Third Degree (Complete) Heart Block Excessively slows HRMay require pacemaker, Atropine not effective Second Degree AVB Third Degree COMPLETE HB Complete absence of conduction of electrical impulse through AV node, Bundle of His, and BB Atria rhythm independent from Ventricular rhythm; Regular P-P and regular R-R LIFETHREATENING Rhythm, will lead to asystole Requires Pacing Causes; Inferior wall MI, Ischemic Heart Disease, Medications (Dig, BB, CCB), hyperkalemia Complete Heart Block Treatment of CHB Cardioversion or Defibrillation Transcutaneous pacing for symptomatic bradycardia Medications Atropine Vasopressors CCB BB Nursing Assessment Bundle Branch Block Irregular conduction or block of electrical pathway through bundle branches Ventricles do not contract simultaneously QRS > 0.12, appears “notched” Ventricular Arrhythmias PVC’s Ventricular Tachycardia Ventricular Fibrillation Premature Ventricular Contraction, PVC’S Abnormally wide, bizarre QRS complex, not associated with P wave Electrical impulse generated in ventricle, Bundle Branch, or Perkinje Fibers Does not lead to contraction of ventricles, therefor not “perfused” Usually followed by compensatory pause Can be observed with or without a pattern Causes of PVCs Increased Catecholamine and increased sympathetic tone Stimulants Amphetamine and cocaine Myocardial ischemia or infarction CHF Hypoxemia Acidosis Dig Toxicity Hypokalemia Hypomagnesemia Significance of PVCs Isolated PVC without hx heart disease are usually insignificant, and require no treatment May indicate presence of ventricular abnormality Can lead to V tach or V fib Single PVC Ventricular Bigeminy Ventricular Trigeminy Couplet Run PVC Ventricular Tachycardia AKA V Tach Dysrhythmia originating in an ectopic pacemaker in the bundle branches, perkinje fibers, or ventricular myocardium Rate 100 – 250 bpm P wave absent QRS abnormally wide and bizarre V Tach Causes of V Tach Significant Cardiac Disease CAD ACS Cardiomyopathy LVH Dig Toxicity QT interval Prolongation Electrolyte disturbances Liquid protein diets Clinical Significance of V Tach Determine inset and termination More than 3 PVCs is sustained V Tach Can be short, nonsustained and asymptomatic Increased frequency can lead to Ventricular Fibrillation which is LIFETHREATENING PULSELESS V TACH IS TREATED THE SAME AS V FIB! Ventricular Fibrillation No coordinated ventricular beats are present No P wave or QRS complexes noted Electrical Chaos in Heart Ventricles ‘contract’ at rate of 300 – 500 bpm EMERGENCY Cardiac output CEASES Nursing Considerations V FIB Asystole Total Absence of electrical activity in heart Pt is clinically dead Absence of P wave and QRS complex Flat line Remember, if your patient is speaking to you then they are NOT in a systole Treatments Cardioversion and Defibrillation Medical Management Atropine Vasopressors Calcium Channel Blockers Beta Blockers Nursing Considerations Oxygen, Pain management Atropine Blocks parasympathetic nervous system influence on the heart Accelerates SA node firing rate Increases HR Increases conduction velocity Administered by IV bolus Used in Symptomatic Bradycardia Second Degree Type I AVB Second Degree 2:1 AVB Third Degree AVB with narrow QRS complexes Atropine Ineffective in Second Degree Type II AVB Advanced AVB with wide QRS complexes Third Degree AVB with wide QRS Complexes Use with Caution Acute MI Worsening myocardial ischemia Heart Transplant patient Vasopressors Cause vasoconstriction on arterioles and venous circulation Improves blood pressure Increases HR and Strength of Contraction Epinephrine Vasopressin (DOC in asystole) Dopamine Norepinephrine Dobutamine Isopreterenol Antidysrhythmics Adenosine; depress AV node and Sinus node activity SVT, Tachycardia Will not terminate Afib/flutter but will slow rate Amiodarone; Affects NA, K, and Ca channels SVT VT Vfib Lidocaine; Widely used, ? Effectiveness in VT SE; altered consciousness, seizures, bradycardia Procainamide; supresses atrial and ventricular dysrhythmias by slowing conduction VT, control of rate in AF/AF, PVST Calcium Channel Blockers Diltiazem and Verapamil Slow conduction and increase conduction time through AV node Used in Afib and A flutter with rapid ventricular response Contraindicated in 2nd and 3rd Degree AVB With Beta Blocker Therapy Use with caution on CHF and hypotension Beta Blockers Decrease HR and BP Used in SVT To control rate in Afib Aflutter Time for a Game EKG Jeopardy! jeopardylabs.com/play/ekgjeopardy#.VOLPYmdso-w.gmail Fifteen Question EKG Rhythm Strip Analysis http://www.12leadecg.com/arrhythmias/index.cf m Wave Matching 1. Ventricular Depolarization 2. Irregular Ventricular Beat 3. Atrial Depolarization 4. 0.12-0.20 5. Ventricular Repolarization 6. Backup pacemaker Rate 40-60 10. Sets Normal Heart Rate A. AV Node B. T wave C. PAC D. SA Node E. PVC 7. Early atrial beat F. P wave 8. Pacemaker site G. QRS Complex 9. 0.06-0.12 Take Home Points EKG is measurement of ELECTRICAL activity Look at the patient Irregular activity can progress from asymptomatic to life threatening Causes are similar (electrolytes, hypoxia, ischemia…) Treatments also very similar (BB, CCB, antiarrhythmic) References http://lifeinthefastlane.com/ecg-library/ http://ekg.academy/learnekg.aspx?seq=11&courseid=315 http://my.clevelandclinic.org/services/heart/pati ent-education