Attention-Deficit Hyperactivity Disorder (ADHD)
Attention-Deficit Hyperactivity
Disorder (ADHD)
B Y M I C H A E L P E L S T E R A N D
S A R A H L E G G E T T
Some Basics
ADHD = ADD
Global prevalence is approximately 5%.
Boys vs. Girls?
Considered to be a chronic disease (30%-50%)
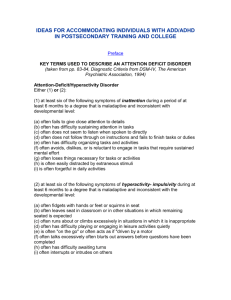
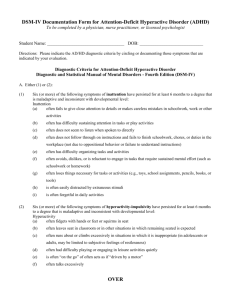
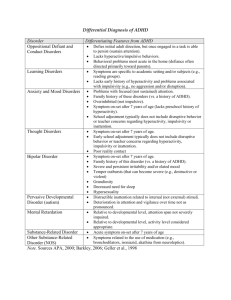
Diagnostic Criteria (DSM-IV)
Diagnostic criteria for Attention-Deficit/Hyperactivity Disorder
( cautionary statement )
A. Either (1) or (2):
(1) inattention: six (or more) of the following symptoms of inattention have persisted for at least 6 months to a degree that is maladaptive and inconsistent with developmental level:
(a) often fails to give close attention to details or makes careless mistakes in schoolwork, work, or other activities
(b) often has difficulty sustaining attention in tasks or play activities
(c) often does not seem to listen when spoken to directly
(d) often does not follow through on instructions and fails to finish school work, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions)
(e) often has difficulty organizing tasks and activities
(f) often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (such as schoolwork or homework)
(g) often loses things necessary for tasks or activities (e.g., toys, school assignments, pencils, books, or tools)
(h) is often easily distracted by extraneous stimuli
(i) is often forgetful in daily activities
Diagnostic Criteria (DSM-IV), continued…
(2) hyperactivity-impulsivity: six (or more) of the following symptoms of hyperactivity-impulsivity have persisted for at least 6 months to a degree that is maladaptive and inconsistent with developmental level:
Hyperactivity
(a) often fidgets with hands or feet or squirms in seat
(b) often leaves seat in classroom or in other situations in which remaining seated is expected
(c) often runs about or climbs excessively in situations in which it is inappropriate (in adolescents or adults, may be limited to subjective feelings of restlessness)
(d) often has difficulty playing or engaging in leisure activities quietly
(e) is often "on the go" or often acts as if "driven by a motor"
(f) often talks excessively
Impulsivity
(g) often blurts out answers before questions have been completed
(h) often has difficulty awaiting turn
(i) often interrupts or intrudes on others (e.g., butts into conversations or games)
B. Some hyperactive-impulsive or inattentive symptoms that caused impairment were present before age 7 years.
C. Some impairment from the symptoms is present in two or more settings (e.g., at school [or work] and at home).
D. There must be clear evidence of clinically significant impairment in social, academic, or occupational functioning.
E. The symptoms do not occur exclusively during the course of a Pervasive Developmental Disorder , Schizophrenia , or other
Psychotic Disorder and are not better accounted for by another mental disorder (e.g., Mood Disorder , Anxiety Disorder ,
Dissociative Disorders , or a Personality Disorder ).
Code based on type:
314.01 Attention-Deficit/Hyperactivity Disorder, Combined Type: if both Criteria A1 and A2 are met for the past 6 months
314.00 Attention-Deficit/Hyperactivity Disorder, Predominantly Inattentive Type: if Criterion A1 is met but Criterion
A2 is not met for the past 6 months
314.01 Attention-Deficit/Hyperactivity Disorder, Predominantly Hyperactive-Impulsive Type: if Criterion A2 is met but Criterion A1 is not met for the past 6 months
Causes
Genetics?
Pre-natal Environment?
Diet?
Environmental/Social Factors?
Criticism
Hunter vs. Farmer Theory
Neurodiversity / Social Construct
Why is it so controversial? (from McMaster U.)
1. No precise test
2. Frequently-changing diagnostic standards
3. Not able to be cured
??? (flawed)
4. Type of therapy (stimulants)
5. Diagnostic rates differ by country.
Pharmacological Treatment
Stimulants: Adderall and Ritalin (methylphenidate)
Adderall: inhibits mono-amine transporters (increasing levels of dopamine, norepinephrine, and serotonin) and MAO’s at high doses
Ritalin (methylphenidate): norepinephrine and domanine reuptake inhibitor
-closest pharmaceutical analog to cocaine; however, cocaine has a higher infinity for the dopamine transporter, contributing to euphoria; the method of ingestion is almost important here.
Pharmacological Treatment
Non-stimulant: Strattera (atomoxetine)
Selective norepinephrine reuptake inhibitor
Lower abuse potential, but not as effective
Potential Side Effects
Common side effects of stimulants for ADD & ADHD:
Feeling restless and jittery
Difficulty sleeping
Loss of appetite
Headaches
Upset stomach
Irritability, mood swings
Depression
Dizziness
Racing heartbeat
Tics
Stimulant medications may also cause personality changes. Some people become withdrawn, listless, rigid, or less spontaneous and talkative. Others develop obsessive-compulsive symptoms.
Potential Side Effects (continued…)
Stimulant safety concerns
Beyond the potential side effects, there are a number of safety concerns associated with the stimulant medications for ADD / ADHD.
Effect on the developing brain — The long-term impact of ADD / ADHD medication on the youthful, developing brain is not yet known. Some researchers are concerned that the use of drugs such as Ritalin in children and teens might interfere with normal brain development.
Heart-related problems — ADD / ADHD stimulant medications have been found to cause sudden death in children and adults with heart conditions. The American Heart Association recommends that all individuals, including children, have a cardiac evaluation prior to starting a stimulant. An electrocardiogram is recommended if the person has a history of heart problems.
Psychiatric problems — Stimulants for ADD / ADHD can trigger or exacerbate symptoms of hostility, aggression, anxiety, depression, and paranoia. People with a personal or family history of suicide, depression, or bipolar disorder are at a particularly high risk, and should be carefully monitored when taking stimulants.
Potential for abuse — Stimulant abuse is a growing problem, particularly among teens and young adults. College students take them for a boost when cramming for exams or pulling allnighters. Others abuse stimulant meds for their weight-loss properties. If your child is taking stimulants, make sure he or she isn’t sharing the pills or selling them.
From today’s NY Times
“A small study of children with attention deficit hyperactivity disorder last year found that walks outdoors appeared to improve scores on tests of attention and concentration. Notably, children who took walks in natural settings did better than those who walked in urban areas, according to the report, published online in August in The Journal of Attention Disorders. The researchers found that a dose of nature worked as well as a dose of medication to improve concentration, or even better.
Andrea Faber Taylor, a child environment and behavior researcher at the Landscape and Human Health Laboratory at the University of Illinois , says other research suggests that all children, not just those with attention problems, can benefit from spending time in nature during the school day. In another study of children who live in public housing, girls who had access to green courtyards scored better on concentration tests than those who did not.”