Innate Immunity: Nonspecific Defenses of the Host Chapter 15 of the
advertisement
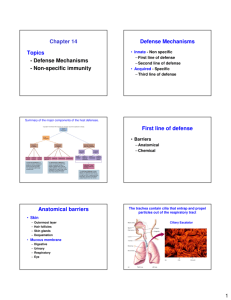
Innate Immunity: Nonspecific Defenses of the Host Chapter 15 of the Host The Concept of Immunity • A pathogen can cause disease only if – It gains access, by penetrating the surface of the skin or entering another portal of entry – Attach itself to host cells – Evade the body’s defense mechanisms long enough to produce harmful changes The Concept of Immunity • The structures, cells, and chemicals that act against pathogens are categorized into 3 main lines of defense • – First line defenses • External physical barriers – Second line defenses • Cells, blood chemicals, and processes to kill invaders • – Third line of defense • Responds uniquely to species or strains of pathogens First Line of Defense: Skin and Mucous Membranes Physical Factors • • _________consists of tightly packed cells with – Keratin, a protective protein – Outer layer is dead • Slough off bacteria along with dead skin cells • Dermis – Difficult to penetrate Skin continued • Skin tends to be ______ – Inhibits cell growth • Microorganisms rarely penetrate skin on their own • Most bacteria live in warm moist areas on skin • Staphylococcus species – Normally inhabit epidermis (hair follicles and sweat glands) – Most likely organisms to cause infections Physical Factors • Mucous membranes – Line gastrointestinal, respiratory, and urinary tracts – Mucus: – Ciliary escalator: Ciliated cells of the respiratory system infected with Bordetella pertussis. The ciliary escalator. Trapped particles in mucus Cilia Ciliated cells Goblet cells Insert Fig 16.4 Ciliated cells propel dust and microbes that have been trapped in mucus upward toward throat. 1-3cm per hour Cigarette smoke toxic to ciliated cells which impairs function Physical Factors • Lacrimal apparatus: washes eye • Saliva: dilute and wash microbes off of mouth surfaces • Urine: flows out • Vaginal secretions: flow out • Peristalsis (coordinated contractions of the GI tract), defecation, and vomiting expel microbes The lacrimal apparatus. Lacrimal glands Upper eyelid Lacrimal canal Nasolacrimal duct Nose Chemical Factors • Skin: – Fungi and bacteriostatic fatty acid in sebum (oily substance) – • Lysozyme in perspiration, tears, saliva, and urine – • Saliva – Urea and uric acid • Low pH (1.2–3.0) of gastric juice in Stomach • Low pH (3–5) of vaginal secretions • Urine low pH (6) Normal Microbiota and Innate Immunity • Competitive exclusion: Second Line of Defense • Operates when pathogens penetrate the skin or mucous membranes • Second line defenses include cells and antimicrobial compounds The Body’s Second Line of Defense • Defense Components of Blood – Lactoferrin- iron-binding compounds • Bind to iron which is an important part of some enzymes and important for growth – – Antibodies (adaptive system) Figure 15.4 A schematic representation of hematopoiesis Blood stem cell in bone marrow Myeloid stem cell Erythroid stem cell Erythrocyte Platelets Basophil Inflammation Clotting, inflammation Gas transportation Neutrophil Lymphoid stem cell Eosinophil Monocyte Lymphocyte Phagocytosis Innate immunity, second line of defense Leukocytes Adaptive immunity The Body’s Second Line of Defense • Defense Components of Blood – Granulocytes • Contain large granules that stain different colors • Three types – » Phagocytize pathogens » Capable of migrating out of blood vessels into surrounding tissue – _______________ can leave the blood releasing inflammatory chemicals » Not phagocytic The Body’s Second Line of Defense • Defense Components of Blood – Agranulocytes • Two types – » Most involved in adaptive immunity – » Leave the blood and mature into macrophages » Macrophages are phagocytic cells that devour foreign objects, including bacteria, fungi, spores, dust, and dead body cells The Body’s Second Line of Defense • Defense Components of Blood – Lab analysis of leukocytes • Differential white blood cell count can signal signs of disease – Increased eosinophils indicate allergies or parasitic worm infection – Bacterial diseases often show increase in leukocytes and neutrophils Effects of Complement Activation • • • Outcomes of Complement Activation. 1 Inactivated C3 splits into activated C3 C3a and C3b. 2 C3b binds to microbe, resulting in opsonization. C3b C3a C3b proteins 3 C3b also splits C5 into C5a and C5b 5 C3a and C5a cause mast cells to release histamine, resulting in inflammation; C5a also attracts phagocytes. opsonization C5 Enhancement of phagocytosis by coating with C3b C5b Histamine C5a Insert Fig 16.9 Mast cell 4 C5b, C6, C7, and C8 bind together sequentially and insert into the microbial plasma membrane, where they function as a receptor to attract a C9 fragment; additional C9 fragments are added to form a channel. Together, C5b through C8 and the multiple C9 fragments form the membrane attack complex, resulting in cytolysis. C5a receptor C5a C6 C3a receptor C3a inflammation C7 C8 Increase of blood vessel permeability and chemotactic attraction of phagocytes C9 Microbial plasma membrane Channel C6 C7 C5b C8 C9 Formation of membrane attack complex (MAC) C6 C5b C7 C8 C9 Cytolysis cytolysis Bursting of microbe due to inflow of extracellular fluid through transmembrane channel formed by membrane attack complex Interferons (IFNs) – Interferons • • Cause many symptoms associated with viral infections – alpha and beta » Cause cells to produce antiviral proteins that inhibit viral replication Figure 15.7 The actions of alpha and beta interferons Virus infects cell. Virus Doublestranded RNA Viral replication in cell triggers transcription and translation of IFN- or IFN-, depending on type of host cell. IFN gene Time passes Meanwhile, the infected cell dies, releasing viruses. Nucleus mRNA IFN Infected cell Infected cell at a later time Interferon is released, diffuses to neighboring uninfected cells, and binds to receptors. Interferon receptor When the second cell becomes infected with viruses, doublestranded RNA of the virus activates AVP. Inactive AVP Binding triggers transcription and translation of inactive antiviral proteins (AVPs). AVP gene Doublestranded viral RNA Active AVPs Time passes Ribosome mRNA mRNA Inactive AVPs Uninfected neighboring cell Same neighboring cell now protected at the later time Active AVPs degrade mRNA and bind to ribosomes, which stops protein synthesis and viral replication. Phagocytosis • Ingestion of microbes or particles by a cell, performed by phagocytes Macrophage Bacterium Pseudopods Phagocytosis • Neutrophils and Eosinophils • Macrophages- specialize in phagocytosismature monocytes Blood stem cell in bone marrow Myeloid stem cell Neutrophil Eosinophil Monocyte Phagocytosis Phagocytosis • Phagocytosis – Cells capable of phagocytosis are called phagocytes – Can be divided into 6 steps • • • • • • Figure 15.6 The events in phagocytosis Chemotaxis of phagocyte Neisseria to microbes (microbes) Adherence Pseudopodia move (chemotaxis) Ingestion of microbes by phagocytes Fusion of a series of vesicles, including lysosomes Phagosome TEM 1m Killing of microbes by enzymes and other chemicals Golgi body Lysosome Nucleus Phagolysosome Residual body Pseudopod Phagocyte Elimination (exocytosis) Inflammation • – Sun burn, cuts, chemicals, abrasions • Acute inflammation – – Is typically beneficial – Elimination of whatever condition precipitated it • Chronic inflammation – – Causes damage to tissue resulting in disease Signs of Inflammation • • • • Redness Swelling (edema) Pain Heat Inflammation process • Dilation and increased permeability of the blood vessels • Migration of phagocytes into infected tissue • Tissue Repair Fever • Pyrogens trigger the hypothalamus to increase the body’s core temperature • Hypothalamus is normally set at 37°C • Body increases rate of metabolism, and shivering occurs, which raise temperature • Various types of pyrogens • • • Fever • Advantages – Produces interferon – Thought to enhance perfomance of phagocytes – Increases temperature above optimal for the microorganism • Disadvantages – Dehydration – 44–46°C fatal