Cardiac Electrophysiology and its Regulation Carmel M. McNicholas
advertisement

BIOLOGICAL MEMBRANES
AND PRINCIPLES OF
SOLUTE AND WATER
MOVEMENT
Carmel M. McNicholas, Ph.D.
Department of Physiology & Biophysics
Contact Information:
MCLM 868
934 1785
cbevense@uab.edu
Sept. ‘11
OUTLINE
•Biological Membranes and Principles of Solute
and Water Movement
•Diffusion and Osmosis
•Principles of Ion Movement
•Membrane Transport
•Nerve Action Potential
•HANDOUT AND PROBLEM SET
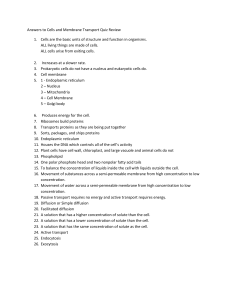
The Cell: The basic unit of life
(i) obtaining food and
oxygen, which are used
to generate energy
(ii) eliminating waste
substances
(iii) protein synthesis
(iv) responding to
environmental changes
(v) controlling exchange
of substances
(vi) trafficking
materials
(vii) reproduction.
The fluid compartments of a 70kg adult human
EXTRACELLULAR (~40%)
BLOOD
PLASMA
~3 L
[Na+] = 142 mM
[K+] = 4.4 mM
[Cl-] = 102 mM
[protein] = 1 mM
Osmolality =
290 mOsm
Capillary endothelium
INTRACELLULAR (~60%)
INTERSTITIAL FLUID
~13 L
[Na+] = 145 mM
[K+] = 4.5 mM
[Cl-] = 116 mM
[protein] = 0 mM
Osmolality = 290 mOsm
TRANSCELLULAR FLUID
~1 L
Composition:
variable
Epithelial cells
INTRACELLULAR
FLUID
~25 L
[Na+] = 15 mM
[K+] = 120 mM
[Cl-] = 20 mM
[protein] = 4 mM
Osmolality = 290
mOsm
Plasma membrane
TOTAL BODY WATER (~42 L)
Modified from: Boron & Boulpaep, Medical Physiology, Saunders, 2003.
Solute composition of key fluid compartments
•Osmolality
constant
•Cell proteins –
10-20% of the
cell mass
•Structural and
functional
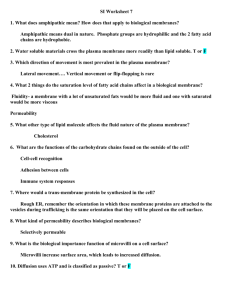
Membranes are selectively permeable
Gas molecules are
freely permeable
Small uncharged
molecules are freely
permeable
Large / charged
molecules need
‘assistance’ to
traverse the plasma
membrane
Structure of the Plasma Membrane
The Extracellular Matrix
Epithelial cell
Basement
membrane
Capillary
endothelium
Connective
tissue and
ECM
Fibroblast
The extracellular matrix
(ECM) of animal cells
functions in support,
adhesion, movement and
regulation
The Extracellular Matrix
The ECM is an organized meshwork of polysaccharides
and proteins secreted by fibroblasts. Commonly
referred to as connective tissue.
COMPOSITION:
Proteins: Collagen (major protein comprising the ECM),
fibronectin, laminin, elastin
Two functions: structural or adhesive
Polysaccharides: Glycosaminoglycans, which are mostly
found covalently bound to protein backbone
(proteoglycans).
Cells attach to the ECM by means of transmembrane
glycoproteins called integrins
• Extracellular portion of integrins binds to collagen,
laminin and fibronectin.
• Intracellular portion binds to actin filaments of the
cytoskeleton
The Cytoskeleton
Intracellular network of protein filaments
Role
Supports and stiffens
the cell
Provides anchorage for
proteins
Contributes to dynamic
whole cell activities (e.g.,
dividing and crawling of
cells and moving vesicles
and chromosomes)
Three Types Of
Cytoskeletal
Fibers
Microtubules (tubulin - green)
Microfilaments (actin-red)
Intermediate filaments
Structural Junctions
Tight
Junctions
Adhering
Junctions
Desmosome
Zonula Adherens
(belt)
Gap Junctions
ROLE: Passage of solutes (MW<1000) from cell to cell.
• Cell-cell communication
• Propagation of electrical signal
The Membrane Glycocalyx - cell coat
Alberts et al., Molecular Biology of the
Cell, 4th Ed. Garland Science, 2002)
Carbohydrates are:
• Covalently attached to membrane proteins and lipids
• Sugar chains added in the ER and modified in the golgi
Oligo and polysaccharide chains absorb water and form a
slimy surface coating, which protects cell from mechanical and
chemical damage.
Membrane Carbohydrates and Cell-Cell Recognition
– crucial in the functioning of an organism. It is the
basis for:
> Sorting embryonic cells into tissues and organs.
> Rejecting foreign cells by the immune system.
Transport of large molecules
EXOCYTOSIS: Transport molecules migrate to the
plasma membrane, fuse with it, and release their
contents.
ENDOCYTOSIS: The incorporation of materials from
outside the cell by the formation of vesicles in the plasma
membrane. The vesicles surround the material so the cell
can engulf it.
Exocytosis
Endocytosis
Principles of Solute
and Water Movement
Diffusion and Osmosis
Membranes are selectively permeable
Gas molecules are
freely permeable
Small uncharged
molecules are freely
permeable
Large / charged
molecules need
‘assistance’ to
traverse the plasma
membrane
Diffusion
Diffusion is the net movement of a substance (liquid
or gas) from an area of higher conc. to one of lower
conc. due to random thermal motion.
Kinetic characteristic of diffusion
of an uncharged solute
Model: compartments separated by permeable glass
x
Cs1
compartment 1
Cs2
compartment 2
A = cross sectional area of the glass disc
Cs = concentration of uncharged solute
x = thickness
x
Cs1
compartment 1
Cs2
compartment 2
According to kinetics, the rate of movement can be
described as follows:
rate of diffusion from 1 2 = kCs1
-{rate of diffusion from 2 1 = kCs2}
----------------------------------------------------------------------------
net rate of diffusion across barrier
= k(Cs1-Cs2) = kCs
where k is a proportionality constant.
Diffusion is proportional to the surface area
of the barrier (A) and inversely proportional
to its thickness (x).
k can thus be expressed as ADs/x, where Ds
is the diffusion coefficient of the solute.
The concentration gradient across the
membrane is the driving force for net
diffusion.
FLUX (Js) describes how fast a solute moves, i.e. the
number of moles crossing a unit area of membrane per
unit time (moles/cm2.s)
Therefore, net diffusion rate = ADsCs/x.
Dividing both sides by A (to obtain flux), we obtain:
Fick’s first law of diffusion:
Flux = Js = DsCs/x
“The rate of flow of an uncharged solute due to
diffusion is directly proportional to the rate of change
of concentration with distance in direction of flow”
When the concentration gradient of a substance is zero
the system must be in equilibrium and the net flux must
also be zero.
Diffusion of an uncharged solute
Model: compartments separated by a lipid
bilayer
x
Cs1
compartment 1
Cs2
compartment 2
Biological membranes are composed of a lipid bilayer of
phospholipids interspersed with integral and peripheral
proteins (“Fluid Mosaic Model”).
Partitioning of an uncharged solute
across a lipid bilayer
The partition coefficient, Ks will increase or decrease the
driving force of the solute S across the membrane:
Js = KsDsCs/x
Cs1
Lipophilic
Ks > 1
Hydrophilic
Ks < 1
Ks lies between
0 and 1
Cs2
Because it is difficult to measure Ks, Ds and x, these
terms are often combined into a permeability coefficient,
Ps = KsDs/x.
It follows that:
Js = PsCs
Solute movement across a lipid
bilayer through entry into the lipid
phase occurs by simple diffusion.
This movement occurs downhill and
is passive.
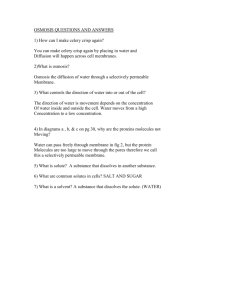
Osmosis: The flow of volume
Osmosis refers to the net movement of water across
a semi-permeable membrane (or displacement of
volume) due to the solute concentration difference.
Osmosis. The flow of volume
The solute concentration difference causes water to
move from compartment 2 1. The pressure
required to prevent this movement is the osmotic
pressure.
Time
1
2
1
2
Osmosis. The flow of volume
AN IDEAL MEMBRANE
(Meniscus)
Piston
(The piston applies
pressure to stop
water flow)
H2O
Cs
1
Compartment 1
Cs
2
(Compartment 2
is open to the
atmosphere)
Compartment 2
Here the membrane is only permeable to water which will
flow down its concentration gradient from 2 1.
The volume flow can be prevented by applying pressure to
the piston. The pressure required to stop the flow of
water is the osmotic pressure of solution 1.
The osmotic pressure () required is
determined from the van’t Hoff equation:
= RTCS = (25.4)CS atm at 37°C.
Where, R = the gas constant (0.082 L.atm.K-1.mol-1),
T = absolute temperature (310 K @ 37 ºC) and CS (mol.L-1)
is the concentration difference of the uncharged solute
Osmosis. Importance of osmolarity
φic = osmotically effective concentration
φ is the osmotic coefficient
‘i’ is the number of ions formed by
dissociation of a single solute molecule
‘c’ is the molar concentration of solute
(moles of solute per liter of solution)
e.g. what is the osmolarity of a 154
mM NaCl solution, where φ = 0.93
→
154 x 2 x 0.93 = 286.4 mOsm/l
Osmosis. The flow of volume
A NONIDEAL MEMBRANE
Piston
S
Cs1
H2O
Cs2
The osmotic pressure depends on the ability of the
membrane to distinguish between solute and solvent.
If the membrane is entirely permeable to both, then
intercompartmental mixing occurs and = 0.
The ability of the membrane to “reflect” solute S is
defined by a reflection coefficient S that has values
from 0 (no reflection) to 1 (complete reflection).
Thus, the effective osmotic pressure for nonideal
membranes is:
eff = SRTCS
Osmotic and hydrostatic pressure
differences in volume flow
Volume flow across a membrane is described by:
JV = KfP
where Kf is the membrane’s hydraulic conductivity and P
is the sum of pressure differences.
These pressure differences can be hydrostatic (PH),
osmotic (eff) or a combination of both. There is
equivalence of osmotic and hydrostatic pressure as
driving forces for volume flow, hence Kf applies to both
forces.
Thus, JV = Kf(eff – PH) (Starling equation)
and (eff – PH) is the driving force for volume flow.
Starling Forces
Arteriole
Interstitial fluid
pressure under
normal conditions
~0 mmHg
Venule
Interstitial
space
= fluid
movement
Filtration dominates
Absorption dominates
Osmotic (oncotic) pressure
Importance of plasma proteins!
Tonicity
Principles of Ion Movement
Diffusion of Electrolytes
K+
Ac-
Cs1=100mM
Cs2=10mM
–
V
+
For charged species, both electrical and
chemical forces govern diffusion.
The Principle of Bulk Electroneutrality
All solutions must obey the principle of bulk
electroneutrality: the number of positive charges in a
solution must be the same as the number of negative
charges.
Diffusion of Electrolytes
Cs1=100mM
Cs2=10mM
K+
Ac– V +
Ac-
K+
Law of electroneutrality (for a bulk solution) must be
maintained. In the above model in which the membrane
becomes permeable to sodium (K+) and acetate (Ac–), both ions
will move from side 1 2.
The concentration gradient between compartment 1 and 2 is
the driving force.
K+ (with the smaller radius) will move slightly ahead of Ac–,
thereby creating a diffusing dipole. A series of dipoles will
generate a diffusion potential.
Eventually, equilibrium is reached and Cs1 = Cs2 = 55mM
Diffusion of Electrolytes
Cs1=100mM
K+
Cs2=10mM
Ac– V +
When the membrane is permeable to only one of the ions (e.g.,
K+) an equilibrium potential is reached. Here, the chemical and
electrical driving forces are equal and opposite.
Equilibrium potentials (in mV) are calculated using the Nernst
equation:
Eion
CS1
2.3RT
log 2
zF
CS
Eion
CS1
60
log 2
z
CS
R = gas constant; T = absolute temp.; F = Faraday’s constant; z = charge
on the ion (valence); 2.3RT/F = 60 mV at 37ºC
The Nernst Equation is satisfied for ions at
equilibrium and is used to compute the electrical
force that is equal and opposite to the
concentration force.
Eion
C
60
log
z
C
1
S
2
S
At the Nernst equilibrium potential for an ion,
there is no net movement because the electrical
and chemical driving forces are equal and
opposite.
• Even when there is a potential difference
across a membrane, charge balance of the bulk
solution is maintained.
• This is because potential differences are
created by the separation of a few charges
adjacent to the membrane.
Calculating a Nernst Equilibrium Potential
Cs1 = 100mM
Na+
Cs2 = 10mM
Ac– V +
Eion
C
60
log
z
C
1
S
2
S
For the model above, the Nernst potential for Na+,
ENa = 60 log(100/10) = +60 mV
Taking valence of the ion into account
in calculating a Nernst potential
Here, z = -1
ECl 60 log
ECl
Cl o
Cl i
[Cl-]i = 10 mM [Cl-]o = 100 mM
100
60 log
60 mV
10
EK 60 log
[ K ]o
[K ] i
[K+]i = 100 mM [K+]o = 10 mM
10
EK 60 log
60 mV
100
Equilibrium potentials of various ions for a mammalian cell
ION Extracellular
Conc. (mM)
Na+
145
Cl116
K+
4.5
Ca2+
1
Intracellular
Conc. (mM)
12
4.2
155
1x10-4
Equilibrium
Potential (mV)
+67
-89
-95
+123
Remember:
Log 10/100 = log 0.1 = –1
Log 100/10 = log 10 = +1
A 10-fold concentration gradient
of a monovalent ion is equivalent,
as a driving force, to an electrical
potential of 60 mV.
Membrane potential vs. equilibrium potential
When a cell is permeable to more than one ion then
all permeable ions contribute to the membrane
potential (Vm).
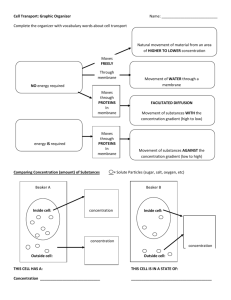
Membrane Transport
Mechanisms I
1. Most biologic membranes are virtually impermeable to:
Hydrophilic molecues having molecular radii > 4Å
e.g. glucose, amino acids)
Charged molecules
2. The intracellular concentration of many water soluble
solutes differ from the medium in which they are bathed.
Thus, mechanisms other than simple diffusion across
the lipid bilayer are required for the passage of
solutes across the membrane.
Transport across cell membranes
Transport through pores
A general characteristic of pores
is that they are always open.
Examples:
1) Porins are found in the outer
membrane of gram-negative
bacteria and mitochondria..
2) Monomers of Perforin are
released by cytotoxic T
lymphocytes to kill target cells
from: Boron, W.F. & Boulpaep, E.L., eds., Medical Physiology, 2003.
Transport Through Channels
General Characteristics of
ion channels:
1) Gating determines the
extent to which the
channel is open or
closed.
2) Sensors respond to
changes in Vm, second
messengers, or ligands.
3) Selectivity filter
determines which ions
can access the pore.
Source: Boron, W.F. & Boulpaep, E.L., eds., Medical Physiology, 2003.
4) The channel pore
determines selectivity.
Why do we need to know how ion channels
influence cells……..?
Macular degeneration
Na+ channel blocker
Solute movement through pores
and channels occurs via simple
diffusion, is passive and
downhill. Metabolic energy is not
required.
Transport through carriers
Carriers never display a continuous transmembrane path.
Transport is relatively slow (compared to pores and channels)
because solute movement across the membrane requires a
cycling of conformation changes of the carrier to allow the
binding and unbinding of a limited number of solutes.
Carrier mediated transport
Cotransporter Exchanger
Facilitated diffusion: the carrier transports solute from a
region of higher to lower concentration. No additional energy
sources are required.
Carrier-mediated transport:
Facilitated diffusion
Such proteins are important for:
1) the transport of cell nutrients and multivalent ions
2) ion and solute asymmetry across membranes
While diffusion processes display a linear relationship between
flux and solute concentration, carrier transport exhibit saturation
kinetics.
Hyperbolic plots of transport activity Jx vs. [X] are indicative
of Michaelis-Menten enzyme kinetics.
Carrier-mediated transporters display competitive inhibition
Fick’s 1st law
J max [ X ]
Jx
Km [ X ]
Carrier mediated transport:
Active Transport
• Movement of an uncharged solute from a region of lower
concentration to higher concentration (uphill)
• Movement of a charged solute against combined chemical
and electrical driving forces
• Requires metabolic energy
• Two classes: primary and secondary
Primary Active Transport – Na-K ATPase
• ATP-dependent
• Electrogenic
• Important for maintaining ionic gradients (conduction,
nutrient uptake)
• Important for maintaining osmotic balance
Secondary Active Transport-Symport
An example of a secondary active transporter is the
electroneutral Na/Cl cotransporter.
Na+
Cl-
Na+
The energy released from Na+ moving down its electrochemical gradient is
used to fuel the transport of Cl– against its electrochemical gradient. Note
that the Na+ pump plays an important role in maintaining a continual Na+
gradient.
Comparison of Pores, Channels, and Carriers
PORE
CHANNEL
CARRIER
Conduit through
membrane
Always open
Intermittently
open
Never open
Unitary event
None
(Continuously
open)
Open/close
Cycle of
conformational
changes
Particles
translocated
per ‘event’
---
60,000 *
1-5
Particles
translocated
per second
Up to 2
billion
1-100 million
200-50,000
* Assuming a 100 pS channel, a driving force of 100 mV and an open time of 1 ms
The “pump-leak” model
(generating the membrane potential)
Na+
K+
~
Na+
K+
Cl–
Pr–
The Na-pump that pumps 2 K+ into the cell in exchange for 3 Na+ out.
Under steady-state conditions, the diffusion of each ion in the opposite
direction through its channel-mediated “leak” must be equal to the amount
transported.
For most cells, however, PK > Pna. In the absence of a membrane potential, K+
would diffuse out of the cell faster than Na+ would diffuse in, thereby
violating the law of electroneutrality. Thus, a Vm is generated that reduces
the diffusion of K+ out of the cell and simultaneously increases the
diffusion of Na+ in.
Vm is generated by the ionic asymmetries across the membrane, which are
established by the Na-pump.
Gibbs-Donnan Membrane
Equilibrium
•Proteins are not only large, osmotically active
particles but they are also negatively charged
anions
•Proteins can influence the distribution of other
ions so that electrochemical equilibrium is
maintained
Gibbs-Donnan Equilibrium
Na+
Cl–
Na+
P–
1
Initially
Na+
Cl–
2
1
Na+
Cl–
P–
2
Equilibrium
In the simple model system above, Cl– will diffuse from 1
2, and Na+ will follow to maintain electroneutrality. In
compartment 2 then, Cl– will be present and [Na+]equil. >
[Na+]initial at Donnan equilibrium.
Because of the asymmetrical distribution of the
permeant ions, there must be a Vm that simultaneously
satisfies their equilibrium distributions.
Gibbs-Donnan equilibrium
(the tendency for cells to swell)
At equilibrium, the increase in osmotically active particles
leads to the flow of water into compartment 2.
Na+
Cl–
Equil.:
Na+
Cl–
H2O
1
P–
2
In animal cells, the presence of large impermeant
intracellular anions tends to lead to cell swelling due to
Donnan forces. However, the Na+ pump actively extrudes
osmotic solutes and counteracts the cell swelling.
The Na-pump (Na-K pump) is essential
for maintaining cell volume
K+
Na+
2K+
ClH 2O
~
K+
Na+
P-
[Na+]
+]
[K
3Na+ [Cl ]
Equal number of +ve and
–ve charges move:
Equilibrium
~
Cl-
P-
↑[Na+]
↓[K+]
↑[Cl-]
H2O
Inhibition of the Napump (ouabain) → cell
swelling
Membrane Transport
Mechanisms II
and the Nerve Action
Potential
Apical
Epithelia
Microvilli
Tight junction
Basal Lamina
Basolateral
• Lie on a sheet of connective tissue (basal lamina)
• Tight Junctional Complexes:
Structural
Allow paracellular transport
• Apical membrane; brush border (microvilli) –
increases surface area
• Apical (mucosal, brush border, lumenal) and
basolateral (serosal, peritubular) membranes have
different transport functions
• Capable of vectorial transport
Models of Ion Transport in Mammalian Cells
e.g. Cl- secretory cell
Transepithelial potential difference
NEGATIVE
POSITIVE
Na+
APICAL/
MUCOSAL
SIDE
K+
ClNa+
Na+ BASOLATERAL/
K+
SEROSAL/
ClBLOOD SIDE
K+
H2O
Paracellular
Transcellular
Absorptive Epithelia - e.g. Villus cell
of the small intestine
Na+-driven glucose
symport
Lateral domain
Carrier protein
mediating passive
transport of glucose
Basal domain
(Modified from: Alberts et al., Molecular Biology of the Cell, 4th Ed. Garland Science, 2002)
Common Gating Modes of Ion Channels
(Source: Alberts et al., Molecular Biology of the Cell, 4th Ed. Garland Science, 2002)
Diffusion of electrolytes through
membrane channels
The following are three important features of ion channels
that influence flux :
1) Open probability (Po). Opening and closing of channels are
random processes. The Po is the probability that the channel is
in an open state.
2) Conductance. 1/R to the movement of ions. Where V=IR
(Ohms law)
I
V
3) Selectivity. The channel pore allows only certain ions to
pass through.
Electrophysiological Technique: Patch Clamp
Terminology and Electrophysiological Conventions
Membrane
potential (Vm)
+100 mV
(Positive)
Depolarize
OUTWARD
CURRENT
I
V
0 mV
-100 mV
-100 mV
Hyperpolarize
+100 mV
Reversal
Potential
(I=0)
(Negative)
INWARD
CURRENT
How the behavior of an ion channels can be
modified to permit an increased ion flux:
Control/ Wild-type:
Closed state
Open state
An increase in conductance (more current flows/opening)
but the open probability stays the same:
Closed state
Open state
An increase in open probability (the channel spends more
time in the open state, or less time in the closed state)
but the conductance stays the same:
Closed state
Open state
Ionic currents through a single channel
sum to make macroscopic currents
TIMEdependent
closure
Na+ Channel
K+ Channel
VOLTAGE-GATED CHANNELS
VOLTAGEdependent
closure
The resting membrane potential (Vm) describes a
steady state condition with no flow of electrical
current across the membrane.
Vm depends at any time depends upon the
distribution of permeant ions and the permeability
of the membrane to these ions relative to the
Nernst equilibrium potential for each.
Overshoot
20
0
-20
-40
-60
-80
Resting
potential
Depolarizing phase
Membrane Potential (mV)
The Nerve Action Potential
Threshold
-5
0
Repolarizing
Phase
5
10 15 20
Time (ms)
After-hyperpolarization
Changes in the underlying
conductance of Na+ and K+ underlie
the nerve action potential
Chemical and electrical gradients prior
to initiation of an action potential
Na+
K+
+
•At rest, the cell membrane
potential (Vm-rest) is generated
by ion gradients established by
the Na- pump.
•The K+ conductance
(permeability) is high, Na+
conductance is extremely low,
hence Vm-rest is strongly negative.
A stimulus raises the intracellular potential to a threshold
level and voltage-gated Na+ channels open instantaneously
Stimulus
Na+
Na+
Na+
+
+
+ +
+ +
+
Na+
+
Na+
+
1. The membrane becomes permeable to Na+ and
there is a rapid Na+ influx due to due to both
electrical and chemical gradients. The cell
membrane potential becomes progressively, but
rapidly, more positive - i.e. it depolarizes
Membrane Potential (mV)
20
0
-20
-40
-60
-80
0
5
10
15
Time (ms)
The rapid upstroke, or
depolarizing phase, is due to
an increase in Na+ conductance
of the cell membrane due to
activation of voltage-gated
Na+ channels. An all-or-none
response. The cell potential
moves toward ENa due to
20 chemical and electrical driving
forces. Vm does not reach ENa.
Na+
K+ Cl-100
-50
0
+50
+100
+150
Eion
2. Na+ channels Na+
begin to close:
+
+
+
+
+
+
Na+
+
+
+
+
+
+
K++
+
+
+
3. Outward K+ gradient
K+
4. Outward
flux
as voltagedependent K+
K+
channels open
hyperpolarization
K+
- -
- -
-
K+
K+
5. Cell repolarizes
Membrane Potential (mV)
20
0
-20
-40
-60
-80
0
5
10 15
Time (ms)
20
As the cell depolarizes, the
Na+ channels inactivate and
the permeability to Na+ is
reduced. Voltage-gated K+
channels open and the cell
membrane potential becomes
permeable to K+ thereby
driving Vm toward EK. The
continued opening of K+
channel causes a brief afterhyperpolarization before the
cell returns to its resting
membrane potential.
K+ Cl-100
-50
Na+
0
+50
+100
Ca2+
+150
Eion
Gates Regulating Ion Flow Through
Voltage-gated Na+ Channels
DEPOLARIZING Vm
REST
ACTIVATED
(UPSTROKE)
INACTIVATED
out
in
Na+
REPOLARIZATION
→HYPERPOLARIZATION
Activation gate
Inactivation gate
REFRACTORY PERIODS
During RP the cell is incapable of eliciting a normal
action potential
• Absolute RP: no matter how great the stimulus an
AP cannot be elicited. Na+ channel inactivation gate is
closed.
• Relative RP: Begins at the end of the absolute PR
and overlaps with the after-hyperpolarization. An
action potential can be elicited but a larger than
normal stimulus is required to bring the cell to
threshold.
REVIEW AND PROBLEM SET
Review Question 1
Solute
A+
B+
C++
DEFG (uncharged)
H (uncharged)
Intracellular
conc. (mM)
7
110
1
5
10
2
4
3
Extracellular
conc. (mM)
104
8
0.01
10
100
2
4
1
A. If the membrane potential of a hypothetical cell is –60 mV (cell
interior negative):
a) Given the extracellular concentration listed on the table
above, what would the predicted intracellular concentration
of each of the solutes A-H have to be for passive diffusion
across the membrane.
b) Given the intracellular concentrations calculated in part a),
what can we conclude about the transport mode of each of
the solutes that are not passively distributed.
B. Calculate the Nernst equilibrium potential for each solute.
Review Question 2
Consider a closed system bound by rigid walls and a rigid membrane
separated the two compartments. Assume the membrane is freely
permeable to water and impermeable to sucrose.
Piston
A
B
A) If both compartments contain pure water and a pressure is applied to
the piston establishing a hydrostatic pressure difference across the
membrane, which direction will water flow in? What will the initial rate of
water flow depend on?
B) If no force is applied to the piston and 100 mM sucrose is placed in
compartment A, which direction will the meniscus in compartment B move?
What concentration of NaCl (also impermeant) would have to be added to
compartment B to prevent volume displacement? What hydrostatic
pressure must be applied to the solution in compartment A to prevent this
volume flow?
Review Question 3
Consider two compartments of equal volume separated by a membrane that
is impermeant to anions and water
A
100 mM
NaCl
10 mM KCl
100 mM KCl
10 mM NaCl
B
A) If in addition the membrane is not permeant to Na+, what is the
orientation and the magnitude of the potential difference across the
membrane at 37C? What is the composition of compartment B when the
system reaches equilibrium?
B) If the properties of the membrane change and now the membrane is only
permeant to Na+, what is the orientation and magnitude of the potential
difference?
C) If both Na+ and K+ are permeable, but PNa>PK what will be the orientation
of the potential difference initially? What will be the orientation of the
potential difference and the composition of compartments A and B when
electrochemical equilibrium is reached?