respiratory cycle - emseducation.info
advertisement

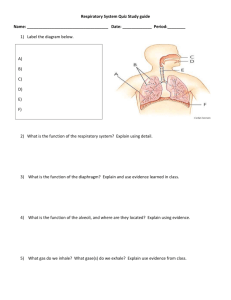
Respiratory Emergencies A Comprehensive Look Respiratory system Provided for the passage of O2 to enter Necessary for energy production and for CO2 to exit Waste product of body’s metabolism. Upper airway Mouth and nose to larynx Nasopharynx: Tonsils, uvula Oropharynx: Tongue Uvula composed of connective tissue containing a number of racemose glands, and some muscular fibers Lower Airway Below the larynx to the alveoli Pharynx Muscular tube Extends vertically from back of the soft palate to superior aspect of the esophagus Allows air to flow in and out of the respiratory tract and food to pass into the digestive tract Larynx Joins the pharynx with the trachea Consists of the thyroid and cricoid cartilage, glottic opening, vocal cords, cricothyroid membrane. Trachea: 10 to 12 centimeter long tube that connects the larynx to the two mainstem bronchi. Lined with respiratory epithelium containing cilia and mucous producing cells. Mucous traps particles that the upper airway did not filter. Cilia move the trapped particles up into the mouth where it is expelled or swallowed. Bronchi: At the carina bifurcates into the right a left mainstem bronchi. Alveoli Bronchioles divide into the alveolar ducts and terminates into the alveoli Comprise the key functional unit of the respiratory system Contain an alveolar membrane that is only 2 cells thick Most CO2 and O2 exchange takes place Become thinner as they expand Surface area totals more than 20 square meters, enough to cover half a tennis court The hollow structure resists collapse due to the presence of a surfactant, a chemical that decreases their surface tension and makes it easier for them to expand. Carina Atelectasis Aveolar collapse Lung Parenchyma Parenchyma: Principal or essential parts of an organ Organized into the lobes Right lung has three lobes where as the left lung has only two as it shares thoracic space with the heart. Pleura Membranous connective tissue that covers the lungs Visceral: Envelopes the lungs and does not contain nerve tissue Parietal: Lines the Thoracic cavity and contains nerve fibers RESPIRATION AND VENTILATION Ventilation: The mechanical process that moves air into and out of the lungs Pulmonary or external respiration: Alveoli Cellular or internal respiration occurs in the peripheral capillaries It is the exchange of respiratory gases between the RBCs and various body tissues Cellular respiration in the peripheral tissue produces CO2 which is picked up by the blood in the capillaries and transports it as bicarbonate ions through the venous system to the lungs. RESPIRATORY CYCLE Nothing within the lung parenchyma makes it contract or expand Ventilation depends upon changes of pressure within the thoracic cavity Begins when the lungs have achieved a normal expiration and the pressure inside the thoracic cavity is equal to the atmospheric pressure Respiratory centers in the brain communicate with the diaphragm by way of the phrenic nerve, signaling it to contract. This initiates the respiratory cycle Then………. Thorax increases; pressure within decreases; becomes lower than atmospheric pressure; with the negative pressure, air rushes in; the alveoli inflate with the lungs, becoming thinner allowing oxygen and CO2 to diffuse across their membranes. When the pressure in the thoracic cavity is again that of the atmospheric pressure, the alveoli are maximally inflated. Pulmonary expansion stimulates microscopic stretch receptors in the bronchi and bronchioles that signal the respiratory center by way of the vegus nerve to inhibit respiration and the influx of air stops. At the end of respiration: Respiratory muscles relax Size of the chest cavity decreases Elastic lungs recoil forcing air out of the lungs (expiration) Expiration is passive Respiration is active process using energy Use of Accessory muscles: Strap muscles of the neck, and abdominal muscles to augment efforts to expand the thoracic cavity Pulmonary Circulation During each cardiac cycle, the heart pumps just as much blood to the lungs as it does to the peripheral tissues. Bronchial arteries that branch from the aorta supply most of their blood. Bronchial veins return blood from the lungs to the superior vena cava. Hypoventilation: Reduction in breathing rate and depth Pneumothorax: Air or gas in the pleural cavity Hemothorax: Accumulation of blood or fluid containing blood in the pleural cavity Pulmonary embolism: Blood clot that travels to the pulmonary circulation and hinders oxygenation of blood Hypoxic Drive The body constantly monitors the PaO2 and the pH. COPD Chronically elevated PaCO2 Body no longer uses PaCO2 levels to stimulate breathing Hypoxic drive increases respiratory stimulation when PaO2 level falls and inhibits respiratory stimulation when PaO2 levels increase. Hypoxemia: Decreases partial pressure of oxygen in the blood Respiratory Acidosis: Retention of CO2 can result from impaired ventilation due to problems occurring in either the lungs or in the respiratory center of the brain. Respiratory Alkalosis results from increased respiration and excessive elimination of CO2. MEASURES OF RESPIRATORY FUNCTION Respiratory rate: Adults 12 to 20 Children 18 to 24 Infants 40 to 60 Eupnea: Normal Respiration Fever Increases Emotion Increases Pain Increases Hypoxia Increases Acidosis Increases Stimulant Drugs Increases Depressant Drugs Decreases Sleep Decreases Total Lung Capacity Total amount of air contained in the lung at the end of the maximal respiration 6L Tidal Volume Average volume of gas inhaled or exhaled in one respiratory cycle 500 mL (5 to 7 cc/kg) Dead Space Volume The amount of gas in the tidal volume that remains in the air passageways unavailable for gas exchange. Anatomic dead space includes the trachea and bronchi Physiologic dead space from COPD, obstruction or atelactesis 150 ml Minute Volume Amount of gas moved in and out of the respiratory tract in one minute Vmin = VT x Respiratory Rate Alveolar Minute Volume Amount of gas that reaches the alveoli for gas exchange in one minute VA-min = (VT – VD) X Respiratory rate RESPIRATORY PROBLEMS Dyspnea: An abnormality of breathing rate, pattern, or effort Hypoxia: Oxygen deficiency Anoxia: The absence or near-absence of oxygen Modified forms of respiration Coughing: forceful exhalation of a large volume of air form the lungs, expelling foreign materials from the lungs Sneezing: Sudden forceful exhalation from the nose. Nasal irritation Hiccoughing: Sudden inspiration; caused by spasmodic contraction of the diaphragm with spasmodic closure of the glottis. No physiologic purpose. Occasionally been associated with MI on the inferior (diaphragmatic) surface of the heart Sighing: Slow, deep, involuntary inspiration followed by a prolonged expiration; hyperventilates the lungs and reexpands atlectatic alveoli; occurs once a minute Grunting: Forceful expiration; occurs against a partially closed epiglottis; usually an indication of respiratory distress. Accessory Respiratory Muscles: Intercostal Suprasternal Supraclavicular Subcostal retractions Abdominal muscles In Infants Nasal flaring Grunting COPD Purse their lips Pulsus Paradoxus Comparison of blood pressure between that of inspiration and that of exhalation A drop in blood pressure greater than 10 torr Drop in blood pressure during inspiration Drop is due to increased pressure in the thoracic cavity that impairs the inability of the ventricles to fill. ABNORMAL RESPIRATORY PATTERNS Kusssmaul’s Respirations Deep, slow or rapid, gasping breathing, Commonly found in diabetic ketoacidosis Cheyne-Stokes Respirations Progressively deeper, faster breathing alternating gradually with shallow, slower breathing. Indicates brain-stem injury Biot’s Respirations Irregular pattern of rate and depth with sudden, periodic episodes of apnea Indicates increased intracranial pressure Central Neurogenic hyperventilation Deep, rapid respirations Indicates increased intracranial pressure Agonal Respirations Shallow, slow, or infrequent breathing Indicates brain anoxia Rales: Fine, bubbling sound; on inspiration; fluid in smaller bronchioles Rhonchi; Course, rattling noise on inspiration; associated with inflammation, mucous or fluid in the bronchioles Stridor: Harsh, high-pitched heard on inhalation; laryngeal edema or constriction Snoring: Partial obstruction of the upper airway by the tongue Gurgling: Accumulation of blood, vomitus, or other secretions in the upper airway Tension Pnuemothorax Any tear in the lung parenchyma can cause a pneumothorax. Tension: Large pneumothorax that affects other structures in the chest Progressively worsening compliance when bagging Diminished unilateral breath sounds Hypoxia with hypotension Distended neck veins Marked increase in pressure can prevent ventricles from adequately filling decreasing cardiac output Tracheal deviation Tachypnea/Bradypnea Respiratory effort: How hard a patient has to work to breathe Orthopnea: Difficulty breathing while lying supine Hypothermia Combines the mechanisms of convection, radiation, and evaporation Accounts for a large proportion of the body’s heat loss Heat is transferred to from the lungs to inspired air by convection and radiation Evaporation in the lungs humidifies the inspired air. During expiration, warm humidified air is released into the environment, creating heat loss Respiratory Shock Respiratory system is not able to bring oxygen into the alveoli and remove CO2 Blood leaves the pulmonary circulation without adequate oxygen and with an excess of CO2 The cells become hypoxic while the bloodstream becomes acidic RESPIRATORY CONTROL Respiratory centers within the brainstem control respiration Inspiration and expiration occur automatically and are triggered by impulses generated in the respiratory center of the medulla oblongata during normal respiration The medullary respiratory system contains chemoreceptors that respond to changes in the CO2 and pH levels in the CSF CO2 rapidly diffuses across the blood-brain barrier in to the CSF while H+ and bicarbonate ions do not. Two Respiratory Centers in the Pons Apneustic Located in the lower pons Acts as a shut-off switch to inspiration If non-functional, prolonged inspiration interrupted by occasional expiration Pneumotaxic Center Located in the upper pons Moderates the activity of the apneustic center and provide fine tuning Medulla Oblongata CO2 receptors Internal Carotid Arteries CO2, O2 and B/P receptors Aorta CO2, O2 and B/P receptors Lungs Stretch receptors Pons Modifies rate and depth of breathing Medulla Oblongata Sets basic rate and depth of breathing Nasal Canulae 4 to 6 liters per minute 22 to 44% oxygen Non-rebreather 10 to 15 liters per minute 80 to 100% oxygen Inhaler: Bronchodilator Inhaler: Stimulation of the Sympathetic Nervous System One metered dose Inhaler purse lips around inhaler depress inhaler as patient inhales deeply Patient hold their breath for a few seconds Inhaler: Breathing difficulties with history of COPD/Asthma Inhaler The patient is not responsive enough The maximum dose has been taken