Capnography UC San Diego
advertisement

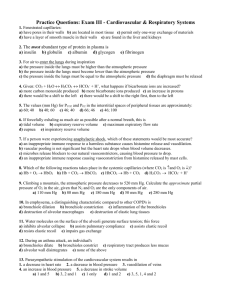
Capnography Tom Archer, MD, MBA Clinical Professor Director, Obstetric Anesthesia UCSD July 3, 2012 Capnography • Detection, display and measurement of CO2 in respiratory gases. • CO2 vs. time (commonest, what we have). • CO2 vs. expired volume (useful, but rarely used). Gas is sampled from the airway (ETT, nose, mask, etc.) and CO2 concentration is displayed over time. Normal capnogram, intubated patient, controlled ventilation Capnography is mostly about expiration • This is logical since inspired gas should not contain CO2. • Inspired gas does contain CO2 with exhausted CO2 absorbent or faulty valves in the circle system. • So both phases matter. Capnography can detect disorders of CO2 production or elimination due to abnormal metabolism (fever, MH, thyrotoxicosis), cardiac arrest, hypotension, pulmonary embolism of clot or air, V/Q mismatch (bronchospasm, COPD), CO2 rebreathing (bad valves in circle system), exhausted CO2 absorbent, ventilator disconnect, etc. Picture from Capnography.com Sidestream capnography Advantages— Sensor does not get damaged or discarded. Heavy sensor does not pull on the ETT. Easier to clean and discard tubing Mainstream capnography Advantages— Does not take gas from the airway (pediatrics). Rapidity of response. Pictures from Capnography.com Normal capnogram. Note that expiration begins before CO2 appears, because of anatomical dead space gas, which contains no CO2 and comes out before alveolar gas. ETCO2 Normal capnogram, controlled ventilation Hyperventilation Normal capnogram, spontaneous ventilation Hypoventilation V/Q mismatch (bronchospasm, COPD): Alveoli emptying early have less CO2. Alveoli emptying late have more CO2. “Curare cleft”: muscle relaxant is wearing off and patient takes a weak breath during exhalation, temporarily decreasing sampled CO2 concentration. “Cardiogenic oscillations”: Cardiac activity moves tracheal gas column enough to vary the sampled CO2 concentration. Absent capnogram • No CO2 production (death). • Cardiac arrest (no CO2 transport to lungs despite ongoing metabolism). • No ventilation (circuit disconnect, esophageal intubation, upper airway obstruction). • Capnograph dysfunction: sampling tube disconnect, loose or blocked filter, etc. Capnography • Detects gross changes in ventilation such as esophageal intubation, disconnection or airway obstruction. • Morphology picks up bronchospasm, patient breathing against ventilator, cardiogenic oscillations, etc. • End-tidal CO2 (ETCO2) has special importance because abrupt decreases in this value can alert us to dangerous events. ETCO2 is the highest CO2 value, which occurs at endexpiration. ETCO2 ETCO2 • This measurement is important because in healthy, well-perfused people, ETCO2 approximates arterial PaCO2. • ETCO2 is also important because when it decreases rapidly it suggests an abrupt change in pulmonary perfusion, due to increased alveolar dead space. Significance of ETCO2. • PaCO2 is always higher than ETCO2– sometimes much higher (see below). • Commonest cause of abrupt fall in ETCO2 is hypotension causing decreased pulmonary artery (PA) pressure. • Low PA pressure cannot perfuse upper parts of lung, creating increased alveolar dead space (DS). • Much less common cause of increased alveolar DS is pulmonary embolism. What is dead space (DS)? • Volume of expired gas which has not participated in gas exchange (i.e. carries no CO2). • Physiological DS = Anatomical DS + Alveolar DS. • Unfortunately, you need to know this. Anatomical dead space consists of the volume of the conducting airways-which never participate in gas exchange and which always empty before the alveoli. Gas from anatomical DS contains no CO2. faculty.alverno.edu Normal capnogram. Note that expiration begins before CO2 appears, because of anatomical dead space gas (AnatDSG), which contains no CO2. ETCO2 AnatDSG Alveolar dead space consists of the volume of the alveoli which are not currently participating in gas exchange. These unperfused alveoli empty at the same time as the alveoli which are participating in gas exchange and the gas inside them dilutes the CO2 in expired gas and decreases ETCO2. www.lib.mcg.edu/.../section4/4ch3/s4ch3_15.htm Normal capnogram. Note that alveolar dead space gas (AlvDSG) comes out at same time as other alveolar gas containing CO2 and serves to dilute expired CO2 and to lower ETCO2. AlvDSG Anatomic and alveolar dead space • Anatomic dead space gas comes out before alveolar CO2. • Alveolar dead space gas comes out at the same time as CO2 from perfused alveoli. • Alveolar dead space gas dilutes CO2 from perfused alveoli. This is why PaCO2 > ETCO2. Rapid decrease in ETCO2 implies rapid decrease in pulmonary perfusion and rapid increase in alveolar dead space, possibly due to: – Hypotension (hemorrhage, pump failure, anaphylaxis, etc.) – Clot or gas embolus – Cardiac arrest 40 ETCO2 = 40 mm Hg ETCO2 = 20 mm Hg With no alveolar dead space With 50% alveolar dead space (e.g.severe hypotension) 20 40 20 Alveolar dead space gas (with no CO2) dilutes other alveolar gas. 40 46 40 46 0 0 40 46 Hemorrhage abruptly reduces pulmonary perfusion and increases alveolar dead space, abruptly reducing ETCO2. Hemorrhage is a common cause of rapid decrease in ETCO2. Thromboembolus abruptly reduces pulmonary perfusion and increases alveolar dead space, abruptly reducing ETCO2. Air embolus abruptly reduces pulmonary perfusion and increases alveolar dead space, abruptly reducing ETCO2. Why does increased alveolar dead space reduce the ETCO2? • The gas in alveolar dead space does not have CO2 in it. • Therefore, alveolar dead space gas dilutes the CO2 coming from the perfused alveoli. • This dilution of expired CO2 during the “alveolar plateau” is the key idea. So, capnography is really cool and useful, but…. Limitations of capnography • “Mesmerism”– don’t forget to watch and examine the patient. Good advice for the rest of your career. • Watch the chest rise and fall (Symmetrical?). • Listen to the chest (bilateral BS? Wheezing? Rales?). • Feel the bag as you hand ventilate (Easy air flow in and out?) Limitations of capnography • Presence of expired CO2 does not protect the airway from aspiration of stomach contents! • During MACs and blocks (including neuraxial), watch the patient! “Never turn your back on a spinal.” • Talk with the patient if she is awake. How does she feel she is breathing? Summary • Capnography is very useful, but hard to understand thoroughly. • Capnography deserves extended and careful study. • Close and informed examination of the capnogram can detect breathing problems early and help prevent patient harm. Capnography.com • An amazingly cool and useful website by Bhavani Shankar Kodali, MD. This website has won many awards and is worth hours of study. • Please use this website if you want to understand capnography in greater depth! The End