Prevention of Non-Ventilator Hospital Acquired
advertisement

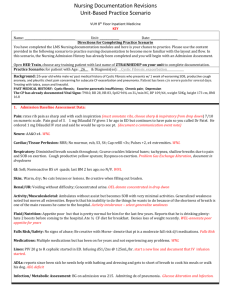
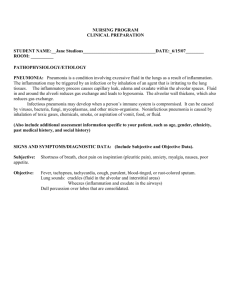
Prevention of Non-Ventilator Hospital Acquired Pneumonia (NV-HAP) ANN-MICHELLE SHERMAN RN, BSN, CMSRN WSU MSN- EDUCATION PRACTICUM PROJECT JANET FREY APRN Objectives State the significance of non-ventilator hospital acquired pneumonia (NV-HAP) Name 3 nurse driven interventions to prevent NVHAP Demonstrate proper technique for IS utilization Explain impact oral care has on prevention of NVHAP Pneumonia Pneumonia Background Under-reported, under studied VAP – well defined prevention measures NV-HAP – studies focus on post surgical and immunocompromised Defined Pneumonia occurring > 48 hours after admission Criteria for HAP (CDC) Cxr – new infiltrate, cavitation or consolidation Immune response – temp > 100.4, leukopenia (<4,000), leukocytosis >12,000, AMS in those >70 yo S&S – new purulent sputum, change in sputum, increased secretions, increased suctioning requirement, new or worsening cough, dyspnea, tachypnea, rales, worsening gas exchange (O2 sat) Mechanical ventilation not in place 48 hours prior to pneumonia diagnosis Background At risk population 3 Common condition categories 1. Enhanced colonization of oropharynx or stomach Use of antacids – gastro pulmonary route • Alkalization of stomach provides environment for bacterial growth Micro aspiration - oropharyngeal colonization Conditions that favor aspiration Decreased CNS 2. • Impaired cough, gag and swallowing Disease process Medications 3. Host factors Age Outliers Risk analysis does not provide enough sensitivity and specificity NV-HAP found outside the risk parameters and in all hospital units Background Significance 18.9 – 29% mortality Cost $28K-$109K Increased length of stay 4-9 days Spread of infection surface contact Droplets Infectious secretions from a sneeze linger in air for hours 4 Interventions Missed opportunities for nursing intervention Elevated head of bed Mobility 59% not mobilized each shift Oral care 34% 73% did not receive each shift IS/C&DB 84% did not receive coaching 4 Interventions Nursing leads the way! Simple interventions can significantly impact your patient! Oral care 1. Decreases oral bacteria Early ambulation Elevate head of bed > 30 degrees Incentive spirometer 2. 3. 4. For patients who have IS ordered 4 interventions Oral care – simple intervention Dental plaque provides microhabitat for growth of bacteria Colonization of bacteria causing pneumonia has been found in oral cavity Mechanical pathway from mouth to lungs provides easy access for bacteria Up to 45% are silent or micro aspirators Hospitalized patients are often immunosuppressed, have poor cough or multiple comorbidities Wide variances in practice (HOB, swab, brush) NV-HAP prevention May be reduced by improving oral care Toothbrush removes plaque, swabs don’t Brush 1-2 minutes Frequency - ? Current standard is 2x/day Antiseptic mouth wash 4 Interventions Early Mobilization and Ambulation Walking to the bathroom is not ambulation Encourage those who are able to walk in the hall NV-HAP prevention Mobilizes secretions Opens collapsed alveoli • Increases lung capacity 4 Interventions Head of Bed elevation 30-45% Patients in prolonged supine position are at risk for GERD Elevation of head of bed promotes esophageal drainage of secretions by gravity For all patients meals should be eaten while upright in chair to decrease aspiration risk o If getting out of bed is contraindicated, place bed in most upright position NV-HAP prevention Prevents aspiration IS simulation Pre-brief Tickets Simulation of techniques to prevent pneumonia Incorporation of current knowledge IS Scenario 58 yo female patient is 3 hours post op right hip replacement for RA. PMH: COPD, current smoker, RA, anxiety. You enter room to do your assessment. VS 124/63, HR 82 regular, RR 16, temp 100.2, pain 2/10. Lungs sounds are coarse crackles, skin warm and dry, peripheral pulses 2+, right hip dressing is dry and intact. Debrief Mosby’s skills Incentive spirometer 4 Steps to Prevention IS NV-HAP prevention • Q 1 hour while awake - May increase frequency if desired • Prevents atelectasis (collapsing of alveoli) • Keeps secretions from pooling in alveoli 4 Interventions IS Instructions for use 1. 2. 3. 4. 5. 6. 7. 8. Identify patient target volume using chart packaged with IS Have patient sit upright in bed or chair Place lips tightly around mouthpiece Take in slow deep breath - maintain constant flow At maximal inspiration hold breath for 5 seconds Allow rest between IS breaths to prevent hyperventilation Perform IS 10 x/hour while awake (more if patient is willing) Enlist family to provide support and coach patients Conclusion HAP occurs in non-ventilated patients Patients on all units are at risk Improved identification and prevention Decreased mortality Increased quality of life Better patient outcomes Fiscal savings Decreased length of hospital stays Impact of nursing actions Don’t miss your chance to prevent pneumonia References Curtis, L. (2008). Review: Prevention of hospital-acquired infections: review of non-pharmacological interventions. Journal Of Hospital Infection, 69(Special edition: Surveillance of Hospital Acquired Infection), 204-219. doi:10.1016/j.jhin.2008.03.018 Echevarría, I. M., & Schwoebel, A. (2012). Development of an Intervention Model for the Prevention of Aspiration Pneumonia in High-Risk Patients on a Medical-Surgical Unit. MEDSURG Nursing, 21(5), 303-308. Fortaleza, C., Abati, P., Batista, M., & Dias, A. (n.d). Risk Factors for Hospital-Acquired Pneumonia in Nonventilated Adults. Brazilian Journal Of Infectious Diseases, 13(4), 284-288. Mehta, Y., Gupta, A., Todi, S., Myatra, S. N., Samaddar, D. P., Patil, V., & ... Ramasubban, S. (2014). Guidelines for prevention of hospital acquired infections. Indian Journal Of Critical Care Medicine, 18(3), 149-163. doi:10.4103/0972-5229.128705 Niederman, M. S. (2010). Hospital-Acquired Pneumonia, Health Care-Associated Pneumonia, Ventilator-Associated Pneumonia, and Ventilator-Associated Tracheobronchitis: Definitions and Challenges in Trial Design. Clinical Infectious Diseases, 51S12-S17. doi:10.1086/653035 Robertson, T., & Carter, D. (2013). Oral intensity: Reducing non-ventilator-associated hospital-acquired pneumonia in care-dependent, neurologically impaired patients. Canadian Journal Of Neuroscience Nursing, 35(2), 10-17. Quinn, B., Baker, D. L., Cohen, S., Stewart, J. L., Lima, C. A., & Parise, C. (2014). Basic Nursing Care to Prevent Nonventilator Hospital-Acquired Pneumonia. Journal Of Nursing Scholarship, 46(1), 11-19. doi:10.1111/jnu.12050