NURSING PROGRAM
advertisement

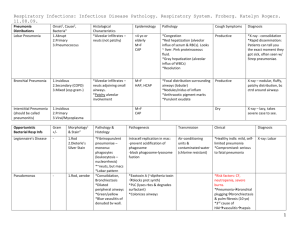
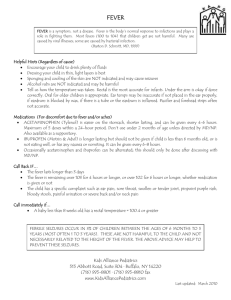
NURSING PROGRAM CLINICAL PREPARATION STUDENT NAME:__Jane Studious________________________________DATE:_6/15/07________ ROOM: __________ PATHOPHYSIOLOGY/ETIOLOGY PNEUMONIA: Pneumonia is a condition involving excessive fluid in the lungs as a result of inflammation. The inflammation may be triggered by an infection or by inhalation of an agent that is irritating to the lung tissues. The inflammatory process causes capillary leak, edema and exudate within the alveolar spaces. Fluid in and around the alveoli reduces gas exchange and leads to hypoxemia. The alveolar wall thickens, which also reduces gas exchange. Infectious pneumonia may develop when a person’s immune system is compromised. It can be caused by viruses, bacteria, fungi, mycoplasmas, and other micro-organisms. Noninfectious pneumonia is caused by inhalation of toxic gases, chemicals, smoke, or aspiration of vomit, food, or fluid. (Also include additional assessment information specific to your patient, such as age, gender, ethnicity, past medical history, and social history) SIGNS AND SYMPTOMS/DIAGNOSTIC DATA: (Include Subjective and Objective Data). Subjective: appetite. Shortness of breath, chest pain on inspiration (pleuritic pain), anxiety, myalgia, nausea, poor Objective: Fever, tachypnea, tachycardia, cough, purulent, blood-tinged, or rust-colored sputum. Lung sounds: crackles (fluid in the alveolar and interstitial areas) Wheezes (inflammation and exudate in the airways) Dull percussion over lobes that are consolidated. DIAGNOSTIC TESTS: (Include implications of abnormal labs, signs and symptoms to observe for, teaching of patient/family regarding abnormal labs). Chest X-ray: Appears as an area of increased density in a lung segment or lobe. May involve one or both lungs. Pulse oximetry: < 95%; (decreased gas exchange due to inflammation and fluid in the lungs) Sputum culture and sensitivity, Gram stain to identify the infectious organism. Bronchoscopy or needle aspiration may be used to obtain lower airway specimens for culture. Labs: CBC shows elevated WBC (leukocytosis) Arterial blood gases (ABGs) to determine baseline levels and determine need for supplemental oxygen. Serum BUN, creatinine, and electrolytes to determine hydration status. (include actual lab values of your patient) TREATMENTS Incentive spirometry – to facilitate deep breathing and reverse atelectasis; coughing and deep breathing. Adequate hydration; monitor intake and output. Supplemental oxygen. Maintain airway patency. Bronchodilators IV antibiotics followed by oral therapy (for infectious pneumonia). Steroids and non-steroidal anti-inflammatory agents may be used for aspiration pneumonia. Pain management Treatment of fever MEDICATIONS: (INCLUDE PURPOSE FOR SPECIFIC TO THIS PATIENT, SIDE EFFECTS, SPECIAL INSTRUCTIONS) Albuterol inhaler – bronchodilator; increases bronchiolar smooth muscle relaxation. Teach correct technique for using inhaler. May cause tachycardia; teach client to monitor heart rate. May cause mouth dryness; increase fluid intake. Levaquin (levofloxacin) - antibiotic; fluoroquinolone – inhibits bacterial DNA synthesis. Side effects: headache, nausea, constipation, dry mouth, difficulty sleeping. Teaching: Take one hour before or two hours after meals with a full glass of water (taking with food, antacids, or dairy products may decrease absorption). Take the antibiotic exactly as directed, even if feeling better. If you stop the mediation, the infection may come back. Tylenol (acetaminophen) – for relief of pain and/or fever (antipyretic, analgesic). Inhibits the synthesis of prostaglandins that serve as mediators of pain and fever in the CNS. Teaching: Take 325 - 650 mg every 4 -6 hours as needed for pain and fever. Do not take more than the recommended amount. Advise client to avoid alcohol intake while taking acetaminophen (3 or more glasses of alcohol/day increases the risk of liver damage). If client is diabetic, warn that acetaminophen may alter results of blood glucose monitoring. (include the dosage that is prescribed for your patient) COMPLICATIONS Hypoxemia Ventilatory failure Pleural effusion Pleurisy Sepsis NURSING PROGRAM CLINICAL PRIORITIZED NEEDS LIST STUDENT NAME:________________________________ DATE:___________ ROOM: _____________ Prioritized Needs List: (Physiological, psychosocial, teaching/learning) Physiological: 1. Maintain adequate gas exchange (give O2 at 2L nc, position with HOB elevated) 2. Maintain patent airway (coughing and deep breathing exercises, incentive spirometry) 3. Maintain hydration/nutrition status Psychosocial: 1. Anxiety related to unfamiliar environment and procedures Teaching/Learning: 1. Understanding of disease process and complications 2. Measures to prevent spread of infection – handwashing, disposal of tissues. 3. Measures to prevent recurrence - finish antibiotics - f/u appointments - C & DB - Planned rest periods - Influenza and pneumococcal vaccinations - Adequate hydration and nutrition - Smoking cessation