X-Ray Interaction with Matter, Human Biology & Radiobiology
advertisement

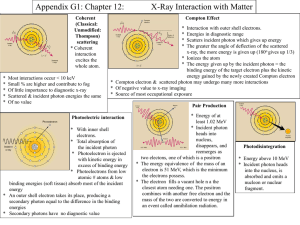
X-Ray Interaction with Matter & Human Biology IMAGE CREATION ATOMS INTERACTION WITH “MATTER” ATOMIC NUMBER Patient Interactions **Photoelectric** Classic Coherent Scatter **Compton Scattering** Pair Production Photodisintegration Interaction in The body begin at the atomic level Atoms Molecules Cells Tissues Organ structures Interactions of X-rays with matter • No interaction; X-ray passes completely through tissue and into the image recording device. • Complete absorption; X-ray energy is completely absorbed by the tissue. No imaging information results. • Partial absorption with scatter; Scattering involves a partial transfer of energy to tissue, with the resulting scattered X-ray having less energy and a different trajectory. Scattered radiation tends to degrade image quality and is the primary source of radiation exposure to operator and staff. Coherent Scattering Also called: Classical scattering or Thompson scattering Occurs with energies below 10 keV Incident x-ray interacts with an atom of matter, causing it to become excited. Immediately the atom releases this excess energy and the scattered x-ray. Coherent Scattering The wavelength is equal to the incident x-ray or equal energy. The only difference is the direction of travel Energy in = Energy out - Only changes is direction Classical (Coherent) Scattering Excitation of the total complement of atomic electrons occurs as a result of interaction with the incident photon No ionization takes place Electrons in shells “vibrate” Small heat is released The photon is scattered in different directions No loss of E Compton Effect or Compton Scattering Occurs throughout the diagnostic imaging range The incident x-ray interacts with the outer electron shell on an atom of matter, removing it. It not only causes ionization but scatters the incident x-ray causing a reductions in energy and the change of direction. Compton scatter A fairly high energy (high kVp) x-ray photon ejects an outer shell electron. Though the x-ray photon is deflected with somewhat reduced energy (modified scatter), it retains most of its original energy and exits the body as an energetic scattered photon. A Compton e- is also released Since the scattered photon exits the body, it does not pose a radiation hazard to the patient. It can, however, contribute to film fog and pose a radiation hazard to personnel (as in fluoroscopic procedures). XXXXX Compton scatter Both the scattered x-ray and the Compton electron have enough energy to cause more ionization before loosing all their energy In the end the scattered photon is absorbed photoelectrically Compton Effect The Compton electron looses all of its kinetic energy by ionization and excitation and drops into a vacancy in an electron shell previously created by some other ionizing event The probability of Compton effect increases as photon energy increases, however the atomic number does not affect the chances of the Compton effect Compton Scatter Compton is just as likely to occur with soft tissue as bone. Compton can occur with any given photon in any tissue Compton is very important in Radiography, but not in a good way. Scattered photons provides no useful diagnostic information Compton Effect Scattered radiation produces a uniform optical density on the radiograph that reduces image contrast Scattered radiation from Compton contributes to the majority of technologists exposure, especially during fluoroscopy STAY AWAY FROM YOUR PATIENT ! Scatter from the Patient during Fluoroscopy ISOEXPOSURE CURVES Photoelectric Effect or Absorption Inner-shell ionization The photon is not scattered it is totally absorbed The e- removed from the atom of matter is called a photoelectron, with an energy level equal to the difference between the incident photon and the e- binding energy. Binding Energy is very important Table 10-2 PHOTOELECTRIC ABSORBTION IN THE PATIENT (CASCADE OF ELECTRONS) Photoelectric effect • A relatively low energy (low kVp) x-ray photon uses all its energy (true absorption) to eject an inner shell electron, • leaving an orbital vacancy. • An electron from the shell above drops down to fill the vacancy and, in doing so, gives up energy in the form of a characteristic ray. • The photoelectric effect is more likely to occur in absorbers of high atomic number (eg, bone, positive contrast media) • and contributes significantly to patient dose, • as all the photon energy is absorbed by the patient (and for the latter reason, is responsible for the production of short-scale contrast). Electron transitions Are accompanied by the emission of more x- rays – secondary radiation Secondary radiation behaves much like scatter radiation Secondary contributes nothing to the image The probability that any given photon will undergo a photoelectric interaction is dependent on the photon energy and the atomic number of the atom CASCADE Photodisintegration • PHOTOELECTRIC ABSORBTION IS WHAT GIVES US THE CONTRAST ON THE FILM Important X-ray Interactions Of the five interactions only two are important to radiology Photoelectric effect or photoelectric absorption Compton scatter Which two tube interactions are important? Compton scatter Contributes to no useful information Is independent of the atomic number of tissue. The probability of Compton is the same for bone atoms and for soft tissue atoms The probability for Compton is more dependent on kVp or x-ray energy Compton Scatter Results in image fog by optical densities not representing diagnostic information Photon are Photons IR is does not know the difference Photoelectric Absorption Provides information to the IR because photons do not reach the IR This represents anatomic structures with high x-ray absorption characteristics; radiopaque structures; tissue with high atomic number; or tissue with high mass density Attenuation – The total reduction in the # of photons remaining in an x-ray beam after penetration through tissue Absorption = x-ray disappears (Photoelectric, Pair production & Photodisintegration) Scattering = partially absorbed, x-ray emerges from the interaction traveling in a different direction (sometimes with less energy) Absorption + Scattering = Attenuation 3 Types of x-rays are important for IMAGE FORMATION DIFFERENTIAL ABSORPTION = the difference between those x-rays absorbed and those transmitted to the IR Compton scatter (no useful information) Photoelectric absorption (produces the light areas on the image) Transmitted x-rays (produces the grey/dark areas on the image) • The probability of radiation interaction is a function of tissue electron density/ atomic number, tissue thickness/density, and x-ray energy (kVp). • Dense material like bone and contrast dye attenuates more X-rays from the beam than less dense material (muscle, fat, air). • The differential rate of attenuation provides the contrast necessary to form an image. • Table 10-10 & 12-4 Differential Absorption Increases as the kVp is reduced Approximately 1% of photons that interact with the patient (primary beam) reach the IR. Of that 1% approximately 0.5% interact to form the image Differential Absorption The difference in x-ray interactions Fundamental for image formation Occurs because of Compton Scattering, Photoelectric absorption, and X-ray transmission Differential Absorption Compton vs. Photoelectric Below 60 kVp Photoelectric absorption is predominant above 60 kVp Compton scatter begins to increase. Dependent on the tissue attenuation properties Table 10-13 Differential absorption factors High atomic number = larger atoms Mass Density = how tightly the atoms of tissue are packed Z # for air and soft tissue are about the same the OD changes are due to mass density difference Table 12–3 & 12-5 Radiation Protection Producing high-quality radiographs require careful technique selection, reducing kVp improves differential absorption and image contrast However, patient dose is increased because more photons are absorbed by the body