PP Chapter 22 Part I
advertisement

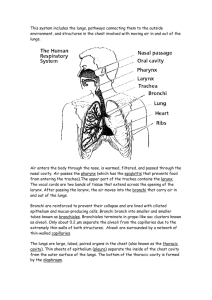
Respiratory System Chapter 22 Biology 2122 Respiratory System Functions 1. Pulmonary Ventilation 2. External Respiration 3. Respiratory Gas 4. Internal Respiration Functional Zones 1. Respiratory 2. Conducting Animation Nose and Para-nasal Sinuses Functions: Airway Warmth and moisture Filter and cleaning Resonation – speech Site of olfactory organs External nose Internal nose ○ Lined with olfactory mucosa ○ Mucus contains lysozyme (antibacterial) ○ Epithelial cells secrete defensins (natural antibiotic) Conchae Paranasal sinuses Pharaynx Nasopharynx Oropharynx Laryngopharynx Nasal Cavity From the 4th to the 6th vertebrae attached to hyoid bone (superiorly) Functions: Opens airway Route air and food into correct passageways Voice production Structure 9 cartilage (hyaline) rings Thyroid cartilage fuses (two plates) and forms the laryngeal prominence (adam’s apple) Arytenoid (anchors vocal cords), cuneiform and corniculate cartilages Larynx Larynx • Ninth cartilage - epiglottis (elastic cartilage) • Vocal folds (true vocal cords) contain no BVs so appear white; vibrate and produce sound – vestibular folds (false vocal cords) – glottis • Superior part of the larynx – stratified squamous: protection from food Trachea 4 inches (10-12 cm) long and 1 inch (2.5 cm) in diameter Contains: (1). Mucosa (goblet cells and P.S. epithelium) (2). Submucosa (CT) (3). Adventitia (CT reinforced by 1620 Cartilage rings –hyaline cartilage) Final cartilage is larger - Carina Trachea branches at the T-7 level Right bronchi is wider, shorter and more vertical Bronchi branch into secondary and tertiary bronchi When the size becomes less than 1 mm in diameter - bronchiole Terminal bronchioles - less than 0.5 mm in diameter Bronchi and Bronchial Tree Respiratory Zone Structures 1. Terminal bronchioles ----- respiratory bronchioles ---- alveoli 2. Alveolar ducts lead into the alveolar sacs (terminal); gas exchange 3. 300 million alveoli Alveoli wall contain – Type-I cells (simple squamous) – Type-II-secrete fluid The alveolar and capillary walls form the respiratory membrane (air-blood barrier) Other features of the alveoli: – Pores between alveoli allow for equalized air pressure – Contain macrophages Respiratory Membrane Lungs Suspended in pleural cavity connected to mediastinum by vascular and bronchial attachments called roots. Costal surface of lungs lie in contact with ribs Hilus Left lung is smaller - the cardiac notch accommodates the heart Fissures Lung ‘odds and ends’ Each lobe of lung contains pyramid-shaped bronchopulmonary segments separated by CT septa – Each is served by own artery and vein Lobules are smallest segments of lungs – Each is served by a large bronchiole and branches Lungs also contain elastic CT – spongy and elastic Lung Circulation Pulmonary and bronchial circulation Pulmonary arteries • bring in blood to be oxygenated • feed into the pulmonary capillary networks surrounded by the alveoli Fresh oxygenated blood - returned to the heart via the pulmonary veins Innervation - Lungs Parasympathetic, Sympathetic motor fibers and visceral sensory fibers enter the lungs via the pulmonary plexus on the lung root Parasympathetic fibers constrict air tubes Sympathetic fibers dilate air tubes Ventilation Inspiration (air into the lungs) Expiration (out of the lungs) Respiratory pressures - atm pressure Atmospheric Pressure (Patm) 760 mmHg sea level=1 atm Pressure exerted by gases surrounding the body Any pressure less than 760 mmHg is less than atmospheric pressure Mechanics of Breathing Thoracic Cavity Pressure Intrapulmonary Pressure (Ppul) (a). Pressure in the alveoli (b). May rise or fall (short periods) but always equalizes out to equal Patm Intrapleural Pressure (Pip) (a). Pressure in the pleural cavity fluctuates with breathing (b). 4 mmHg Less than Ppul and Patm (negative pressure) How is the Intrapleural pressure established? Forces that pull lungs away from wall (cause collapse) Force 1: Lungs Recoil Force 2: Surface Tension of Alevolar Fluid What opposes these forces? Thoracic Cavity Pressure 1. Which force will win? Neither! Due to the adhesive force between the parietal and visceral pleura 2. What is the significance? Pressure differences inside and out side the lungs allow for breathing to take place Air will move down the pressure concentration gradient Pressure is greater outside so air will move into the lungs 3. Consequences of a collapsed lung! The Breathing Process- Ventilation 1. Inspiration Enlargement of the thorax increases volume Boyle’s Law Greater the volume - number of gas particles per unit volume decrease Pressure is greater outside of the lungs! 2. Expiration Volume of thorax decreases pressure increases 1 mm Hg higher than outer pressure Breathe out Changes in Thoracic Volume Pressure Changes and Resistance Factors that Influence Pulmonary Ventilation (1). Airway Resistance (non elastic source of resistance) Drag decreases gas flow Upper respiratory tract is larger; midsize bronchi offer most resistance; terminal bronchioles air flow basically stops (2). Aveolar Surface Tension Liquids drawn together create surface tension Water: strong surface tension If left alone, water create ST on the alveoli and would collapse the alveoli Production of surfactant Less force needed to overcome forces needed to expand lungs Factors that Influence Pulmonary Ventilation 3. Lungs stretch due to elastic fibers- Lung Compliance – (a). Expansion of lungs increases compliance – (b). Determined by • Distensibility of lung tissue • Alveolar surface tension (must be kept low) 4. Diminished by – (a). Fibrosis, scar tissue – (b). Blockages – (c). Reduced production of surfactants – (d). Reduced flexibility of rib cage Respiratory Volumes Links for Ventilation • Ventilation