Helminths & Protozoa
advertisement
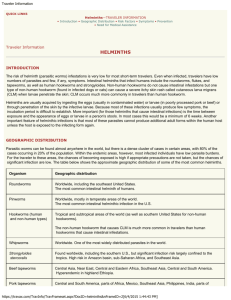
MEDICAL PARASITOLOGY HELMINTHS & PROTOZOA INFORMATION EMPHASIS • Agent and Group ID; general importance • Epidemiology (distribution, transmission, etc) • Pathogenic capability • Diagnosis • Control BASIC TERMINOLOGY & PRINCIPLES • Symbiosis: Living together • Commensalism: One symbiont benefits, other unaffected • Mutualism: Both symbionts benefit • Parasitism: One symbiont benefits, other is damaged COMMON TERMS • • • • • • • • Obligate vs Facultative Parasites Endo- vs Ecto-parasites Pseudo- vs Spurious Parasites Zoonotic Parasites Host-specific vs Non-host-specific Parasites Definitive vs Intermediate Hosts Paratenic/Transfer Hosts Vectors PARASITE SURVIVAL FACTORS • Parasites have successfully adapted to (all?) environmental “niches” in hosts • Parasites best adapted are least pathogenic • Parasite-host relationships are typically longterm/chronic/”intimate” CONDITIONS NECESSARY FOR SUCCESSFUL ENDEMIC PARASITISM • Reservoir of infection • Means of transmission from infected to susceptible, “new” hosts • Ability to invade and successfully reside in “new” hosts • Ability to reproduce HELMINTH/WORM TERMINOLOGY • Adults: sexually reproductive life cycle stage • Larvae: developmental or asexually reproductive life cycle stage • Eggs: stage protective of zygote &/or embryo • Cysts: usually a larval stage encapsulated in tissues of an intermediate host • Hypobiosis: worms in temporary developmental arrest • Monoecious/hermaphroditic: both sexes 1 body • Dioecious: sexes separate; males & females • Parthenogenesis: ability to produce offspring without fertilization of eggs Helminths, continued Worm-terms, continued • Oviparous: production of eggs, discharged from uterus of female • Ovoviviparous: production of eggs which hatch prior to discharge from uterus of female • Viviparous: production of embryos/L1 larvae, no rigid encapsulation of embryo Enteric helminths, continued GENERALIZED NEMATODE LIFE CYCLE Adults Eggs Embryos L1 L2 larva L3 larva L4 larva L5 juvenile Enteric Helminths Ascaris lumbricoides • SI roundworm transmitted fecal-oral via eggs • Pathogenic potential low to high, depending on host species and condition, number of eggs ingested, secondary bacterial agents carried • Clinical signs: larval migration; none, pneumonitis, asthmatic reaction. Adults; SI blockage, plugging of bile duct, perforation of SI, appendix or other site, malnourishment • Reservoir: human DH • Damage potential: dependent on worm #s, host susceptibility to larval and adult action Enteric helminths, continued A. lumbricoides, continued • Prevalence: world-wide, temperate and tropical regions, possibly 1 billion infected • Diagnosis: eggs in feces, observation of ‘dropout’ adult worms • Treatment: piperazine, albendazole, mebendazole, pyrantel pamoate Enteric helminths, continued Ascaris lumbricoides life cycle Extra-enteric helminths, continued Toxocara canis, Toxocara cati, Balisascaris columnaris, others (Visceral Larval Migrans) • Transmission: fecal-oral, ingestion of infective ova • Pathogenic potential high, dependent on #s of larvae, migrational destination(s) • Clinical signs determined by #s of larvae, sites infected; cough, fever, hypereosinophilia, retinochoroiditis, epilepsy, myocarditis, other • Reservoir hosts: canines, felines, mustelids, raccoons, badgers, oppossums, other • Damage potential high: carriers of bacterial contaminants, direct toxicity & tissue destruct. Extra-enteric helminths, continued T. canis, T. cati, B. columnaris, et.al. • Prevalence worldwide, sanitation dependent, cold/cool temperate regions to equator • Diagnosis: serology, lesion/abcess pathological examination (gross & histo), high eosinophil count is strongly suggestive • Treatment: systemic anthelmintics have been used with varying degrees of success, depending on diagnostic timing; fenbendazole & other benzimidazoles, probably avermectins Toxocara canis life cycle Enteric helminths, continued Ancylostoma duodenale & Necator americanus (hookworms) • Transmission via contact of skin with L3 larva • Pathogenic potential: population dependent, each worm sucks blood from mucosa in SI, larval migration usually insignificant • Clinical signs: minor reaction (ground itch), # dependent, at larval entry; pneumonitis via migrating larvae, if large #s; eosinophilia, occult blood in stools, diarrhea, anemia, edema, et.al. • Reservoir: humans, possibly other anthropoids • Damage potential depends on condition & sensitivity of host, and #s of worms Enteric helminths, continued A. Duodenale & N. americanus, continued • Prevalence world-wide, in tropics, subtropics, and warm temperate regions; some zonal variation by species • Diagnosis by ID of ova in feces • Treatment: albendazole, mebendazole, pyrantel pamoate, piperazine (probably) Hookworm Life Cycle Extra-enteric helminths, continued Ancylostoma caninum, A. braziliense, Uncinaria stenocephala, et.al. (cutaneous larval migrans) • Transmission: penetration of skin by direct contact with infective L3 larvae • Pathogenic potential: low, transient • Clinical signs: “serpiginous tracks”/”creeping eruption” on skin near invasion sites • Reservoir hosts: canines, felines, other animals with host-specific species of hookworms • Damage potential: limited to numbers of worms involved, host sensitivity to cutaneous trauma Extra-enteric helminths, continued A. caninum, A. braziliense, U. stenocephala, et.al • Prevalence: worldwide distribution, tropical, subtropical, warm & cool temperate, sub-arctic (Uncinaria) • Diagnosis: visual observation of characteristic “tracks/burrows” on skin surface • Treatment: albenazole, other benzimidazoles Enteric helminths, continued Trichuris trichiura (whipworm) • Transmission: fecal-oral via embryonated ova • Pathogenic potential: low to moderate, dependent on worm numbers & location in LI • Clinical signs: dependent on worm #s; none, bloody(frank)/mucoid diarrhea, abdominal pain & distention, rect. prolapse, anemia, weakness, eosinophilia • Reservoir: mainly human, others possible but host specificity not well documented • Damage hinges on results & numbers of worm mucosal perforations, bacterial/viral involvement, degrees of blood loss, worm location Enteric helminths, continued T. trichiura, continued • Prevalence: worldwide tropical, subtropical, warm temperate sanitation dependent; SE USA, spotty in other states with large populations of infected immigrants • Diagnosis: microscopic ID of ova in feces • Treatment: albendazole is drug of choice Trichuris trichiura life cycle Enteric helminths, continued Capillaria phillipinensis • Transmission: ingestion of larvae in fresh and brackish-water fish • Pathogenic potential high due to worm site and autoinfection factors • Symptoms: abdominal pain, borborygmus, diarrhea early; anorexia, nausea, vomiting, et.al • Reservoir unknown: probably many fish-eating mammals • Damage potential high: populations build via autoinfection; adults and larvae migrate through mucosal tissue in (mainly) jujunal SI Enteric helminths, continued C. phillipinensis, continued • Prevalence high/moderate in Phillipine areas where eating raw fish is a cultural event • Diagnosis: microscopic ID of ova in feces, differentiation from whipworm eggs (Trichuris) • Treatment: mebendazole drug of choice, other benzimidazoles also efficacious Enteric helminths, continued Enterobius vermicularis (pinworm) • Transmission by ingestion of embryonated ova • Pathogenic potential 0/low • Clinical signs: occasional anal itching from night-time exit migration of female worm for oviposition; occasional host skin pruritis to egg ‘glue’; rare migration & disintegration of female worms into urogenital tract of female, with lesions in abdominal cavity via oviducts • Reservoir hosts human (family & friends) • Damage potential 0; no tissue invasion/insult, no apparently toxic by-product production Enteric helminths, continued E. vermicularis, continued • Prevalence world-wide, arctic to equator • Diagnosis: microscopic ID of ova &/or worms on transparent cellophane tape swab of perineum • Treatment: albendazole, and others Enterobius vermicularis life cycle Extra-enteric Helminths Strongyloides stercoralis • Transmission: ingestion of, or skin contact with L3 larva, possibly congenital & transmammary • Pathogenic potential very high due to autoinfection, infection site, parasite-host incompatibility • Clinical signs: skin reaction at larval entry (ground itch), pneumonitis re primary larval migration, diarrhea/dysentery, malabsorption, mucosal ulceration, frank or occult bloody stool • Reservoir hosts: none necessary, free-living agent with invasion capability (facultative P) Extra-enteric helminths, continued S. stercoralis, continued • Damage potential high/extreme: direct damage to SI villar epithelium extensive; worm population buildup intensifies, eventually colonizes colonic mucosa, nutritional absorption restricted/eliminated, dehydration intense • Prevalence: free-living colonies numerous, distribution similar to hookworms, human infections rare, sporadic, but significant • Diagnosis; isolation, microscopic ID of ova, larvae in feces or intestinal biopsies • Treatment: albendazole, ivermectin, others Strongyloides stercoralis life cycle Extra-enteric helminths, continued Trichinella spiralis • Transmission: ingestion of encysted larvae in meat • Pathogenic potential: moderate in majority of infected hosts; # of infective larvae, host tolerance are major factors • Clinical signs: occasional diarrhea during early stages; fever, eosinophilia, muscle pain/stiffness during larval invasion of muscle • Damage potential: low/moderate in ‘healthy’ hosts, high in those in which myocarditis, encephalitis or chronic pneumonitis occur Extra-enteric helminths, continued T. spiralis, continued • Prevalence: low to high, dependent on cultural preferences regarding meat selection & preparation; no climatic factors are involved • Diagnosis: serologic testing, histologic ID of larvae in muscle biopsy • Treatment: corticosteroids, mebendazole, albendazole Trichinella spiralis life cycle Extraenteric helminths, continued Dracunculus medinensis • Transmitted by ingestion of copepod IH • Clinical signs: skin “blister” followed by ulcer with anterior end of female worm visible, cutaneous bulge of skin over body of worm, various immune responses (rashes, asthma) • Reservoir hosts: canines, many other mammals • Damage potential: low to moderate, depending on sensitivity of host to worm excretions and other worm-related antigens • Prevalence worldwide, from equator into cool temperate climatic areas Extraenteric helminths, continued D. medinensis, continued • Diagnosis: observation of skin ulcer, at bottom of which end of female worm is visible • Treatment: removal of worm by gentle extraction from burrow by winding on a stick, with concomitant use of metronidazole or thiabendazole Dracunculus medinensis life cycle Filarid helminths Filarid Helminth Life Cycle DH Adults L4 larva L5 larva microfilariae L1 Vector L2 larva L3 larva Filarid helminths Wuchereria bancrofti (filariasis/elephantiasis) • Transmission by mosquito vectors • Pathogenic potential moderate - high, long term • Clinical signs: variable re host factors and worm species/strains; none, renal disease, hematuria, proteinuria, hyperimmune reactivity, eosinophilia, lymphangitis (soft edematous swelling of extremeties, followed by eventual hardening) • Reservoir hosts: humans, some monkeys • Damage potential variable: immune reactions to worms & worm products varies with individuals, long-term, plugging of lymph vessels Filarid helminths, continued W. bancrofti, continued • Prevalence: throughout tropical and subtropical countries, into some warm temperate areas • Diagnosis: recovery and microscopic ID of microfilaria from blood samples • Treatment: diethylcarbamazine, followed by ivermectin for prevention of reinfection Wuchereria bancrofti life cycle Filarid helminths, continued Brugia malayi, et.al. • Transmission by mosquito species different from those involved with W. bancrofti • Pathogenic potential essentially similar to that described for W. bancrofti • Clinical signs similar to those of W. bancrofti • Damage potential similar to that of W. bancrofti • Prevalence similar to W. bancrofti, regional differences dependent on vector habitat preferences • Diagnosis: microscopic diff of microfilariae from other species • Treatment: diethylcarbamazine + Ivermectin Filarid helminths, continued Loa loa (african eyeworm) • Transmission via chrysops/mango fly vectors • Pathogenic potential moderate, dependent on host sensitivity factors • Clinical signs: eosinophilia, few obvious signs except when adults are migrating across eye; occasional swellings, edema in local sites • Reservoir hosts: monkeys known, possibly et.al • Damage potential low, minor host response normally • Prevalence: tropical, rain forest vector habitat • Diagnosis: ID of microfilaria, extraction of adult • Treatment: Diethylcarbamazine + ivermectin Loa loa life cycle Filarid helminths, continued Mansonella spp., Dipetalonema spp., et.al. • Transmission by midges & blackflies • Pathogenic potential low to zero • Clinical signs usually non-existent • Reservoir hosts: humans, monkeys • Damage potental low, dependent on host sensitivity to specific worms • Prevalence: tropical, subtropical, warm temperate regions where vectors exist • Diagnosis: ID of microfilariae in blood • Treatment: Diethylcarbamazine + ivermectin, when warranted Filarid helminths, continued Onchocerca volvulus (river blindness) • Transmitted by blackfly vectors • Pathogenic potential moderate, dependent on death & decomposition of microfilariae • Clinical signs: adult clusters cause subcutaneous nodules, microfilariae cause blindness • Reservoir hosts: large domestic animals, probably others • Damage potential low/moderate, depending on host sensitivity, toxicity of worm ‘strain’, number and death/decomposition rate of larvae in eye Filarid helminths, continued O. volvulus, continued • Prevalence variable, 5 to 80% in endemic areas near streams needed by blackfly reproduction • Diagnosis; observation of adults in prominent subcutaneous nodules, skin biopsy and histologic examination for microfilariae • Treatment: surgical removal of adults, diethylcarbamazine, ivermectin for larvae Onchocerca volvulus life cycle Filarid helminths, continued Dirofilaria immitis (canine heartworm infection) • Transmission by mosquito vector • Pathogenic potential in human (unnatural host) low/moderate, dependent on host sensitivity • Clinical signs usually absent in humans, dependent on location of worm • Reservoir hosts; canines (dogs, coyotes, etc.) • Damage potential low in humans, dependent on host sensitivity, #s of worms, location of worms • Prevalence wide: tropical, subtropical, warm and cool temperate regions • Diagnosis: usually biopsy of dead, encysted worm • Treatment: surgical removal Flatworms/Platyhelminths Flatworm-related Terminology • Cestodes/tapeworms: segmented flatworms • Trematodes/flukes: leaf-shaped (except for schistosomes), single-unit flatworms • Oncosphere/hexacanth: egg-encased embryo of cyclophyllidean tapeworms • Coracidium: egg-encased embryo of pseudophyllidean tapeworms • Miracidium: egg-encased embryo of flukes • Cysticercoid, cysticercus, coenurus, hydatid cysts: cyclophyllidean tapeworm larval types in IHs Flatworm helminths, continued Flatworm terms, continued • Procercoid, plerocercoid: larvae of pseudophyllidean tapeworms • Scolex: organ of attachment, adult tapeworms • Proglottids: tapeworm body segments • Strobila: tapeworm body (all segments) • Sporocyst, redia: larvae of fluke species • Cercaria: end stage of asexual reproduction of flukes • Metacercaria: encysted cercaria infective to DH Flatworm helminths, continued Trematodes/Flukes Generalized Fluke Life Cycle Adults in DH Egg Miracidium (embryo) Snail primary IH Sporocyst &/or Redia larva Cercaria Vegetation/secondary IH Metacercaria Flatworm helminths, continued Fasciolopsis buski (intestinal fluke) • Transmission: ingestion of metacercaria on aquatic vegetation • Pathogenic potential 0/low • Clinical signs: none, rash, intestinal discomfort • Reservoir hosts: numerous, herbivores • Damage potential: low, minor SI mucosal damage • Prevalence: high, ~ 10 m infections annually in oriental and asian, tropical/subtropical areas • Diagnosis: ID of eggs in fecal sedimentation • Treatment: prazyquantel, niclosamide Fasciolopsis buski life cycle Flatworm parasites, continued Echinostoma spp. (spiny-mouthed flukes) • Transmission: ingestion of metacercaria in snail secondary IH • Pathogenic potential low/moderate • Clinical signs: # dependent, none/mild irritation • Reservoir: many snail-eating mammal DHs • Damage potential low: some SI abrasion • Prevalence: oriental, asian tropical/subtropical countries • Diagnosis: microscopic ID of ova in fecal sed • Treatment: praziquantel, niclosamide Flatworm helminths, continued Heterophyes spp., Metagonimus spp. • Transmission: ingestion of metacercaria in fish secondary IH • Pathogenic potential: low early, rising to high over time, re: worm #s, infection longevity • Clinical signs: none early, myocarditis, seizures, neurologic defecits, other, in chronic infections • Reservoir hosts: most piscivorous mammals • Damage potential: dependent on tissue-infested ova lodged in various organs, emitting toxins produced by embryos; egg #s determine level of damage Flatworm helminths, continued Heterophyes, Metagonimus, continued • Prevalence: high in oriental, asian and other countries where endemic, and cultural consumption of raw fish is common • Diagnosis: microscopic ID of ova in feces via sedimentation concentration • Treatment: nothing effective against systemically lodged ova; prazyquantel, tetrachloroethylene X adults Heterophyidae life cycle Flatworm helminths, continued Paragonimus westermani (lung fluke) • Transmission: ingestion of metacercaria in crustacean secondary IH • Pathogenic potential: moderate to high dependent on worm #s, species toxicity, level of tissue damage • Clinical signs: none, fever, cough, bloody sputum, chest pain, bronchitis, dyspnea • Reservoir: huge, almost any crustacean-eating mammal • Damage potential: early migration through tissues minor; encapsulation in lungs major Flatworm helminths, continued P. westermani, continued • Prevalence: worldwide, dependent on human consumption of raw crustaceans • Diagnosis: microscopic ID of ova in sputum or sedimentation-concentrated feces; ID of ova in needle biopsy of encapsulations in lungs • Treatment: praziquantel, bithionol Paragonimus westermani life cycle Flatworm helminths, continued Fasciola hepatica (sheep, et.al., liver fluke) • Transmission: ingestion of metacercaria on vegetation • Pathogenic potential moderate/high dependent on worm #s & length of infection period • Clinical signs: none early, fever, chills, pain, jaundice, eosinophilia, liver enlargement, other • Reservoir: huge, almost any herbivorous or omnivorous animal is suitable host • Damage potential: moderate to high depending on worm #s; migration through tissues & liver parenchyma, mechanical & toxic effects, hyperplasia of biliary epithelium, cirrhosis Flatworm helminths, continued F. hepatica, continued • Prevalence: millions of human infections probable, worldwide distribution dependent on aquatic vegetation production and consumption • Diagnosis: microscopic ID of ova in fecal sedimentation • Treatment: bithionol, praziquantel Fasciola hepatica life cycle Flatworm helminths, continued Clonorchis sinensis, Opisthorchis spp. (oriental liver flukes) • Transmission: ingestion of metacercaria in fish secondary IH • Pathogenic potential: 0 early, low/moderate late infection, depending on worm #s • Clinical signs: similar to those described for F. hepatica, but usually less intense until worms reach very large population levels • Reservoir: huge, nearly all piscivorous mammals in endemic areas • Damage potential: moderate, similar but usually smaller magnitude than F. hepatica Flatworm helminths, continued C. sinensis, O. spp., continued • Prevalence: high in oriental & other countries where fish are eaten raw; sporadic in many countries, dependent on local cultural factors; some outbreaks tied to transport of fresh fish in non-endemic areas • Diagnosis: microscopic ID of ova in feces processed by sedimentation concentration • Treatment: praziquantel, albendazole Clonorchis/Opisthorchis life cycle Flatworm helminths, continued Dicrocoelium dendriticum (terrestrial liver fluke) • Transmission: ingestion of metacercaria in ant secondary IH; primary IH is a terrestrial snail/slug • This agent is mentioned only to provide an example of adaptability, and is confined to warm, moist areas of the world where gastropod secondary IHs mingle with scavenging, arthropod-ingesting DHs; most of the internal factors described for other liver flukes are applicable to D. dendriticum Flatworm helminths, continued Schistosomes/Bloodflukes Generalized schistosomal life cycle Male & Female Adults in DH Egg Miracidium embryo Snail IH Sporocyst larvae Cercaria Flatworm helminths, continued Schistosoma mansoni, S. japonicum, S. haematobium (blood flukes) • Transmission: direct penetration of skin by forktailed cercaria in water • Pathogenic potential: high, based on worm populations and location in veins, capability of eggs to erode tissue, other • Clinical signs: none early or if worm #s low, transient skin reaction at entry, malaise, fever, skin rashes, cough, acute hepatitis, abcesses, hepatomegaly, cardiomyopathy, haematuria • Reservoir: limited?, monkeys, rodents, humans Flatworm helminths, continued S. mansoni, S. japonicum, S. haematobium, continued • Damage potential high, dependent on location of adults, excretions of adults and miracidia in ova, population #s, egg locations & #s, damage is accumulative over time • Prevalence: distribution worldwide in tropical, subtropical, temperate regions; human infections nearly equal to prevalence of malaria, • Diagnosis: microscopic ID of ova in feces, urine or biopsy specimen • Treatment: praziquantel, oxamniquin, bilarcil Schistosoma species life cycle Flatworm helminths, continued Shistosoma spp. • Transmission: cercarial penetration of skin in water • This group of schistosomes do not develop to adulthood in humans. They are parasites of birds and other animals, but will infect humans when in contact in water. They cause a cutaneous larval migrans referred to as “swimmers itch”, which is transitory and usually eliminated by the immune response Flatworm helminths, continued Generalized Pseudophyllidean Life Cycle Adults in DH SI Egg Procercoid larva Plerocercoid larva Coracidium Copepod primary IH Fish secondary IH Adults in DH SI Flatworm helminths, continued Pseudophyllidean tapeworms Diphyllobothrium latum (broad fish tapeworm) • Transmission: ingestion of plerocercoid larva in uncooked fish • Pathogenic potential: low, dependent on host sensitivity, location of worm in SI • Clinical signs: usually none, pernicious anemia if worm is anchored near pyloric sphincter • Reservoir hosts: various wild & domestic fisheating mammals; dogs, cats, bears, seals, other • Damage potential low: strong affinity for B12 Flatworm helminths, continued D. latum, continued • Prevalence worldwide, where freshwater or brackish water fish are consumed raw • Diagnosis: observation of proglottid chains in stools; microscopic ID of ova in feces • Treatment: prazyquantel, niclosamide Pseudophyllidean (Diphyllobothrium latum) life cycle Flatworm helminths, continued Generalized Cyclophyllidean Life Cycle Adults in DH SI Egg with Onchosphere/Hexacanth Embryo Larva (Cysticercoid, cysticercus, coenurus, hydatid) in IH Adults in DH SI Flatworm helminths, continued Cyclophyllidian tapeworms Taenia solium (pork tapeworm) • Transmitted by ingestion of cysticercus larvae in uncooked pork (adult worm in SI); ingestion of TW eggs in human fecal contamination (cysticercus/larval development in tissues) • Pathogenic potential: low as adult in SI; low/moderate as larvae in tissues • Clinical signs: usually none with adult infection, dependent on location with larval infection • Reservoir hosts: humans and pigs • Damage potential 0 to low with adults, low/moderate with larvae, location dependent Flatworm helminths, continued T. solium, continued • Prevalence: worldwide, where humans and pigs interact, and pork is eaten raw • Diagnosis: observation of proglottid chains in stool for adult worms; biopsy removal of larva from tissue site, microscopic ID of hooklets in a crush mount • Treatment: prazyquantel, niclosamide X adults; albendazole somewhat effective X cysticerci, untreated larval infections often subside (symptom-wise) within 2 to 5 years Flatworm helminths, continued Taenia saginata (beef tapeworm) • Transmission by ingestion of cysticercus larva in fresh, raw beef • Pathogenic potential 0/low • Clinical signs: none, usually • Reservoir hosts: bovine IHs, human DHs • Damage potential 0/low • Prevalence worldwide, wherever beef is eaten raw and cattle are exposed to human feces • Diagnosis: sight of proglottid chains in stool • Treatment: prazyquantel, niclosamide Taenia species life cycle Flatworm helminths, continued Hymenolepis nana, H. diminuta, Dipyllidium caninum, others • Transmission: ingestion of arthropod IH host containing cysticercoid larva • Pathogenic potential 0/very low • Clinical signs: usually none, sensitive DH may show diarrhea, headache, abdominal pain, dizziness, anorexia, other nonspecific signs • Reservoir hosts: rodents, dogs, “normal” DHs • Damage potential 0/very low • Prevalence world-wide, dependent on distribution of “normal” DHs Flatworm helminths, continued H. nana, H. diminuta, D. caninum, continued • Diagnosis complicated by small size of worms, making their observation in stools difficult; eggs may sometimes be observed in fecal flotation examinations • Treatment: prazyquantel, niclosamide Hymenolepis nana life cycle Hymenolepis diminuta life cycle Dipyllidium caninum life cycle Flatworm helminths, continued Larval Tapeworm Infections Echinococcus granulosus, E. multilocularis (unilocular/multilocular hydatidosis respectively) • Transmission: ingestion of ova in feces of DH • Pathogenic potential high, dependent on larval type and organ involved • Clinical signs dependent on size of cyst, organ location: related to pressure, abrasion, other • Reservoir hosts: DH carnivores/omnivores, IH prey species primarily herd animals (sheep, etc) • Damage potential dependent on organ location, size of cyst; moderate to high Flatworm helminths, continued E. granulosus, E. multilocularis, continued • Prevalence in humans spotty, dependent on human interaction with canine DH and herbivore IH; distribution world-wide from equator to arctic, wherever predator-prey activity occurs (everywhere?) • Diagnosis: microscopic ID of protoscoleces from needle biopsy of cyst, X-ray/other image detection of cyst in organ (liver, lung, brain, other); skin test, serotest • Treatment: Surgical removal of cyst (unilocular), albendazole somewhat (variably) effective Echinococcus species life cycle Flatworm helminths, continued Taenia spp. of carnivores • Transmission: ingestion of eggs in DH feces • Pathogenic potential low to moderate, dependent on host sensitivity, #s & location of cysticerci in IH (human) • Clinical signs: none, CNS-related abnormalities, subcutaneous nodules, et.al., site dependent • Reservoir hosts: DH carnivores, IH prey • Damage potential: dependent on worm species, larva type (cysticercus or coenurus), larva location; host sensitivity, number of larvae Flatworm helminths, continued Taenia spp., continued • Prevalence; worldwide, equator to arctic in normal carnivore DHs, prey IHs, spotty, somewhat infrequent/rare in humans • Diagnosis: microscopic ID of larval biopsy • Treatment: albendazole somewhat effectiveseldom/never 100% curative Cysticercosis-causing tapeworm life cycle