Document
advertisement

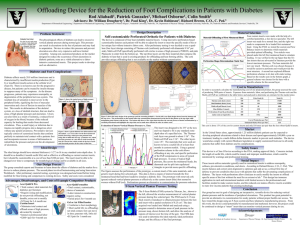
Offloading Device for the Reduction of Foot Complications in Patients with Diabetes Rod Aliabadi1, Patrick Gonzales1, Michael Osborne1, Colin Smith2 Advisors: Dr. William Dougherty3, Dr. Paul King1, Dr. Kevin Robinson4, Richard Brown, C.O., C. Ped.5 Department of Biomedical Engineering1, Department of Mechanical Engineering2, Department of Plastic Surgery3, Vanderbilt University, Nashville, TN, Department of Design Description Problem Statement Material Selection Self-customizable Perforated Orthotic for Diabetics The physiological effects of diabetes can lead to excessive vertical plantar pressure during normal gait. This pressure can result in ulcerations in the feet of patients and may lead to amputation. Devices to reduce this pressure and prevent ulceration are often very expensive and have limited versatility. Among non-customized products on the market designed to reduce the occurrence of foot ulcerations in diabetic patients, none are a viable alternative to labor-intensive customized inserts. Static Coin Test Left foot The device is composed of four individual, heat-moldable material layers. Using innovative perforated customizable features each patient will be able to adjust their insert to meet the specific needs of his or her unique feet. Using a quad-lam (four layer) design consisting of Thermo-cork (uniformly perforated), Multi-cell Puff (specifically perforated), Poron, and pink Plastizote (from the bottom up) optimal performance data was achieved. 15 10 5 0 100 70 200 300 400 500 Left foot coins 600 700 800 600 700 800 Offloading of First Metatarsal Head Legend – Inserts 60 – New Balance insert – Tri-lam/ – Tri-lam/ Plastizote base – Tri-lam/ cork base – Plasitzote/ Spenco 50 40 20 10 0 0 100 200 300 400 500 Four custom inserts were manufactured with the help of a certified pedorthist, a foot device specialist Using the FSM we tested five inserts (four custom and one factory insert) to determine which materials provided optimal offloading. Two coins were placed under the first metatarsal head of the foot (for simulated loading). It was verified that the tri-lam inserts (typically used for diabetic inserts) provided the best offloading. Different base layer materials did not vary a great deal, so Thermo-cork was chosen because it would be most easily perforated. A second test explored the effectiveness of a variety of perforation schemes. Based on the results, a general scheme was chosen for the base with a specific scheme for the second layer. Cost to Manufacture In order to accurately calculate the manufacturing cost of our proposed product, the group assessed the costs of mass production. The materials used in the prototype and the cost of labor for perforating the Thermocork and the multi-cell puff are quantified and exhibited in the table below. Estimate for 2400 Pairs Figure 1 shows the typical areas of high pressure that result in ulceration in the diabetic foot. a) b) d) c ) diabetic foot deformations and Figure 2 shows typical ulcerations. a) a severe ulcer on the first metatarsal head b) foot drop, which prevents patients from being able to hold their feet up c) hammer toe, which increases pressure on a toe after it curls towards the foot d) Charcot foot, which results in the loss of arch and increased pressure in the center of the foot. The ideal design should have minimal thickness (<1/2”) to fit in any standard extra-depth shoe. It should be as durable (4 month useful life) and as effective at offloading as current custom inserts, but it should be customizable at a cost of less than $100 per pair. The insert must be able to be changed over time to compensate for morphological change and be available in all sizes. Design Process The group met with experts and researched the effects of diabetes and the market for a device to reduce vertical plantar pressure in patients’ feet. The second phase involved brainstorming and preliminary testing of materials. A prototype was designed and tested before being modified for final testing and comparison to existing devices. Safety and cost were considered. Example Existing Products, Advantages, Disadvantages, and Cost • Total contact • Require sizing and modification; do not provide offloading; not durable; extra cost to modify • $20/pair for four month use Custom Insert • Maintains total contact and offloads areas of high pressure. • Requires intensive labor by a professional • $260/pair for four month use 0 30 Ideal Design Acor QuikFit Pro Legend - Shapes - Diamond - Circles - Diamonds and circles 20 Diabetes and Foot Complications Diabetes affects nearly 20.8 million Americans and is characterized by insufficient insulin production (Type I) or insufficient insulin action at the cellular level (Type II). There is no known cure for the progressive disease, but patients can be treated by insulin therapy to suppress many of the symptoms. As the disease progresses, patients may experience neuropathy, or degeneration of the peripheral nervous system. The resultant loss of sensation is most severe in the peripheral limbs, signifying the loss of muscular innervation and a loss of flexion in muscles of the feet. This results in deformation of the skeletal system, or a loss of skeletal structure, that can lead to areas of high plantar pressure and ulceration. Ulcers can also form as a result of ischemia, a reduced level of oxygen in the blood, because of the reduced capacity for healing that results from decreased circulation. Thus, a small injury or infection due to trauma can rapidly progress into a dangerous ulcer without any patient awareness. Preventative devices typically consist of customized insoles that conform perfectly to maintain total contact with a patients foot and incorporate recesses in areas of deformation to redistribute the pressure and prevent the development of ulcerations. static coins 25 Acor QuikFormables • Total contact; customizable • Labor intensive construction; requires sizing • Varied prices for four month use Gel or Air Filled Insoles • Conforms to foot morphology • Short useful life; no offloading; not total contact; foot can move in shoe; puncture risk, little aid •$15/pair for one month use Part Qty Price Each ($) Total ($) Thermo-cork sheets (Acor) 100 156 15600 Dual laminate sheets (Acor) 100 120 12000 Multi-cell puff sheets (Acor) 100 48 4800 Glue (Rubber Cement) 25 2.50 67.50 Perforations (H and K perforations) 200 25 5000 Labor costs (at 6 pairs/hr) 40 15/hr 600 Figure 3 shows the basic design of the prototype and the reasoning behind it. On the left is our final design shown from the bottom and the top views. The perforations on the bottom allow the customization demonstrated on the heel in the photos at the top right. The bottom left shows a flow chart that describes the current process of insole customization by a certified professional and highlights the steps that can be made more efficient in order to reduce costs. Cost per Pair Estimated Cost of Device Social Impact The insert was designed to be 3/8” in thickness and shaped to fit in any standard extra depth shoe. The Thermo-cork layer was ground to approximately 1/16”. The Multi-cell Puff was also 1/16”. The remainder of the thickness came from the other layers, which were 1/8” each. The materials that were used are known to have a useful life of at least four months in current models, so this application should be similarly useful. A general perforation scheme in the cork will allow offloading at any site, and the specific perforation of the Puff compensates in areas of typical high pressure. The devices can be quickly ground to any size during fabrication. Test 1L Max 30 20 $15.86 $30 In the United States alone, approximately 1.25 million diabetic patients can be expected to develop peripheral ulcerations related to their disease and spend approximately $30,000 a year on treatment, leading to a multi-billion dollar domestic market to prevent such maladies. The device would also comply with current Medicare legislation to supply customized footwear to all needy patients that suffer from diabetes and its complications. Safety Issues This device is a Class I Device according to the FDA, making approval likely. Concerns include the length of useful life, which could be tested, and improper modification, which could be minimized by warnings and professional training. Conclusion 50 40 38067.50 Market These inserts utilize materials typically used in customized inserts to address neuropathy, calluses, pre-ulcerative conditions, and ulcers. According to Richard Brown, C.O., C. Ped, “The inserts balance and correct joint alignment to optimize gait and act as a critical first line of defense to prevent conditions that occur with patients that suffer the devastating complications of diabetes. The layers with perforations allow clinicians to easily modify the inserts to offload specific areas of the foot without the need for an extensive lab.” This design has immense application in rural and international markets with limited access to the professionals and facilities needed to make custom insoles, and the reduced cost makes effective inserts available to more low-income patients than existing technology. F-Scan Vertical Plantar Pressure Testing A maximum pressure map of the left foot produced using data obtained from the F-Scan Mobile (FSM) system is exhibited to the right. The FSM uses a 0.15 10 mm thick resistive transducer to obtain vertical plantar pressures of the foot during its natural gait 20 2 cycle with a spatial resolution of 0.25 cm . This data was then loaded into Matlab and analyzed using a 30 program created to determine areas of peak pressure to view regions of interest over the period of the gait. 40 A graphic showing the FSM apparatus is displayed on the left. This free-moving device measured and 50 relayed plantar pressures between the foot and 60 insert. The FSM data was also used to determine the efficacy of the final prototype. Sum Our group has met its goal of designing an inexpensive and versatile device effective in reducing vertical plantar pressure by means of customization. We have tested the design using an F-Scan sensor and have planned a manufacturing process. From the work we have completed, the device could potentially be manufactured and marketed; however, the project could be continued in order to develop a “smart” insert to plan and monitor pressure offloading throughout a patient’s use. Acknowledgements 10 0 5 10 15 20 Richard Brown Nashville Orthotic & Prosthetic Services Dr. Kevin Robinson Department of Physical Therapy Dr. William Dougherty, Dr. Naji Abumrad, Michele Frisbie, Dr. Horace Watson