Healthy Feet HQ EBOOK
advertisement

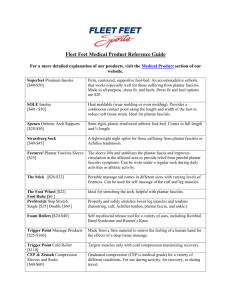
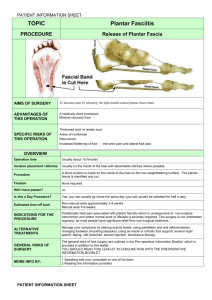
Common Causes of Achilles Tendon Pain The Achilles’ tendon is located down the back of the lower leg. This tendon connects to the heel bone and calf muscle and enables you to walk by helping you to raise your heel off the ground. Achilles tendon pain can be difficult to deal with, especially because it limits your mobility, which can be a big problem if you’re active. Learning how to cope and treat this issue can help you to get back on your feet significantly faster while also working to prevent future injuries from occurring. Injury to the tendon can be frustrating and recuperating is a long process, even for mild cases. Because of this, many people find it difficult to take the necessary amount of time to ensure that the tendon is fully healed before beginning strenuous physical activity. It’s best to wait until you receive approval from your physician prior to restarting your workout regimen or returning to work. Achilles tendon Pain and other Causes of Heel Pain As you walk, you put a lot of stress on your feet. The feet are able to handle a heavy load, but significant stress and overuse can push your tendon over the limit. Running on hard surfaces or playing sports can irritate sensitive tissues in the heels and feet, resulting in severe pain. The heel can usually heal on its own but can require several months of rest. If you experience pain beneath the heel you may suffer from stone bruises, plantar fasciitis, heel spurs or a tendon issue. A stone bruise results when the runner steps on a hard object, bruising the underside of the heel. Typically, this injury will heal after only a few weeks of rest. Plantar fasciitis can be caused by overuse, resulting in inflammation of the band of tissue that connects the heel bone to the base of the toes. Again, several weeks of rest will usually resolve this issue. A heel spur can form in the area where the fascia tissue connects to the heel bone. Treatment usually involves rest until the pain subsides. Achilles tendinosis and tendonitis are the most common types of issues diagnosed when a patient suffers from tendon pain. Tendinitis versus Tendinosis Tendinitis is diagnosed when inflammation is noted. This type of inflammation should resolve in a matter of days as long as the patient avoids strenuous physical activity. If left untreated or if the patient fails to rest for the required amount of time this condition can progress to tendinosis. Tendinosis is the degeneration of the tendon and is considered a serious condition that can require surgery and months of recovery time. Tendinitis is usually caused by excessive running, walking or exercise. Other causes include exercising without warming up, playing certain types of sports such as tennis, wearing high heels daily, and wearing poorly fitting shoes. Diagnosing this type of condition is fairly simple. First, your physician will ask questions regarding your pain level and evaluate the amount of swelling in the heel. They may also ask you stand on the balls of your feet and test your range of motion. Tendinitis treatment can range from taking anti-inflammatory medication to steroid injections. Surgery is rarely required unless the condition has progressed to tendinosis. Other treatments include stretching daily, rest, wearing a brace, icing the area several times a day and elevating the foot. The cause of these conditions usually involves the overuse of the tendon by creating an increase in repetitive activity. This type of activity will put too much pressure and strain on the tendon leading to injury. Because of the ongoing stress, the tendon is unable to repair itself in a timely manner and instead more pressure is put on the tendon causing the structure to become altered, thus resulting in injury. Tendinosis is a condition that’s not well understood and it is often confused with tendonitis. Tendinosis is a chronic condition that’s characterized by small tears in the tendon. Tendinitis refers to inflammation of the tendon and is characterized by pain, warmth, swelling and redness. While tendonitis can be resolved easily with rest and time, tendinosis is much different and isn’t characterized by inflammation. Instead, patients with this condition will have thicker tendons, with no redness or warmth present. This condition is also considered a chronic problem that can gradually develop over time and last for years without treatment. While treatment for this condition is similar to that of tendinitis, it’s not the same. Because tendinosis lacks inflammation, the treatment will be directed towards stretching, exercising and shoe inserts. Commonly, when left untreated surgery is the recommended treatment. So what are the common causes of both tendon conditions? Individuals with physically demanding jobs, fitness enthusiasts and athletes are commonly at risk for developing these types of issues. Additionally, people with low arches also have a tendency to develop tendon pain. Signs, Symptoms and Treatment for Tendon Disorders Signs and symptoms can vary from person to person and can range from mild to severe. These symptoms can include intense pain on each side of the tendon, sore or stiff ankles, and enlargement of the tendon and limited range of motion. Diagnosing tendon pain or stiffness may require extensive testing. Initially, your physician will examine your feet and ankles and determine if you suffer from tendinosis or tendinitis. MRIs or x-rays may be necessary in order to determine the extent of damage and to rule out or in favor of surgery. Treatment for tendon pain heavily depends on the amount of damage and the length of the injury. Mild cases may require the use of a cast in order to immobilize the tendon and promote healing. Ice should also be frequently used to reduce swelling. To use, apply a pack of ice to the affected area for a period of twenty minutes each hour until improvement is noted. Ice should never be placed directly against the skin. Instead, wrap the ice pack in a towel or cloth. Obviously, you will need to stop working out or doing the activity that’s causing the tendon pain. This can be required for a period of two to six weeks, based on the condition of the tendon. If you’re worried about getting out of shape during this time, you can try other types of low-impact activities that will reduce the amount of stress placed on the tendons. This includes strength training, cycling or water activities. After your doctor has given you the okay to get back to higher impact workouts you should do so gradually. When you become injured it’s usually necessary to replace the type of footwear you normally wear when working out or running because they can have a negative impact on your stride or gait. You may also need to replace your everyday shoes if you do a lot of walking. Anti-inflammatory medication is often recommended for tendinitis. These medications are known as NSAIDS and can be helpful in reducing swelling, tenderness and pain. Physical therapy may be ordered a few times a week to strengthen the tendon and can include exercises for tendon re-education and massage therapy for patients with tendinitis or tendinosis. If these treatments fail to be successful, your physician may recommend surgery. The type of surgery needed will depend on the extent of the injury. Stretching the other muscles in the lower body can also work to alleviate some stress from the foot and ankle area. Some experts believe that if there is tension in other muscles in the legs or back that this can cause undue stress on the tendons. Try stretching your leg muscles for a period of fifteen minutes a day or consider a professional massage one to two times a week to really loosen up your muscles and promote circulation. If any of these above treatments fail to improve your condition then your physician may recommend surgery, however, surgery should only be considered as a last resort if the patient does not display signs of improvement after a period of four to six months of treatment. What you can expect from Surgery for Tendinosis When surgery is necessary for tendinosis treatment, you can expect a painful and complicated healing process that can take several months. Surgery is not usually part of tendinitis treatment unless it has turned into tendinosis, a process that takes several weeks or months. The surgery itself involves cutting away the degenerated areas of the tendon by removing the outer sheath and working inward removing degenerated areas. During this process, the patient must extend or flex their foot in order to make the degenerated areas easier to view. This is typically an outpatient process, rarely requiring a patient to spend the night in the hospital unless complications arise. After the surgery is complete the patient must wear a hard cast for several weeks and complete physical therapy in order to strengthen the foot and ankle. The entire process can take four to six months. During this time, the patient will be unable to work and must spend a significant amount of time with the foot elevated and with minimal mobility. This is definitely a long and painful process which is why many physicians will attempt to treat your tendon condition using a number of methods prior to recommending surgery. When the Achilles’ tendon has ruptured, successful treatment can be accomplished with or without surgery. This will all rely on how well a patient responds to non-surgical treatment. However, with surgical treatment, the odds of re-rupturing the tendon are significantly reduced. Strengthening the Tendon using Eccentric Exercise and Other Alternative Treatments You can easily avoid issues with your Achilles’ tendon by consistently doing strengthening exercises that will make them more resilient and less vulnerable to injury. If you run or jog, at some point you may experience tendon pain and injury. Unfortunately, this is all too common for the avid runner. If you have had a tendon injury in the past, once you’re able to return to running you’ll be required to reduce the length of your stride significantly. You’ll also need to avoid any other type of cardio workout until the tendon is no longer sensitive. If treated early on, this type of injury is no big deal, but if left untreated the injury can turn into a classic case of tendinosis. Commonly, the avid runner fails to give the tendon the amount of time it needs to truly heal, which in turn can lead to multiple partial ruptures. Fortunately, there are exercises you can do at home that have been proven to prevent future tendon injury. These exercises are known as eccentric exercises. This type of treatment will involve wearing a backpack that’s weighted as you stand on the very edge of a step, placing the heels off the step. You’ll need to raise both heels as high as you can, then remove the injured leg off the step. This leg should be lowered gradually, then placed back on the step. For best results repeat this exercise fifteen times for three sets. Do this exercise for a period of two to four months depending on the condition of the tendon, or a few times a week as prevention. Certain injuries will also respond well to other calf strengthening exercises. Deep tissue massage is another alternative method used to improve Achilles function. Researchers believe that an aggressive massage has the ability to break down weak collagen fibers while also promoting circulation resulting in a faster healing time. Shock wave therapy is a high-tech method used to break down scar tissue. This method utilizes high-frequency machinery that blasts sonic vibrations to the injured area. Some research has shown that the success of this treatment is comparable to the results experienced from consistent eccentric exercise. Plantar Fasciitis Brace for a better night’s rest Plantar fasciitis involves the plantar fascia, which is a thick band of tissue that can be found along the bottom of the foot, connecting the heel bone to the toes. It’s also a common cause of heel pain and can send stabbing pain throughout the foot upon walking. This type of condition is very common in runners or people who are obese or individuals who fail to wear the proper type of running shoes. Using a plantar fasciitis brace during the night can help to minimize pain as you sleep and prevent morning discomfort. How a Plantar Fasciitis Brace can help Wearing a night splint to treat plantar fasciitis will keep the foot in a ninety-degree position, stretching the fascia and relieving pain that’s commonly associated with the first steps of the morning. The only drawback with wearing a brace is the fact that most types may have a negative impact on how well you sleep considering these braces are somewhat bulky and can cause excessive sweating. There are a couple of popular types of splints recommended for plantar fasciitis: the boot and the dorsal. The dorsal brace features a hard plastic support which runs along the shin down to the top of the foot, keeping the foot securely in a ninety-degree angle and leaving the arch of the foot and the heal open. The boot splint features a spine located on the back of the calf and leg, running just under the foot. This type is significantly larger than the dorsal model. With the dorsal brace, the foot can slip out of the brace if you’re a restless sleeper, which can work against holding the proper stretch. It can also be very hot to wear and may cause excessive sweating. With the boot model, it may cause the toes to go numb and is often described by patients as uncomfortable and bulky. It can also be difficult to walk with. Custom Splints for Plantar Fasciitis If you have tried both types of braces without success, another option is having a custom brace made. A custom brace can be made to specifically fit the shape of your feet, providing you with the most comfort and allowing you to move more freely during rest. In order to have a custom model made, you’ll need to meet with a podiatrist. The specialist will take a mold of your foot and send it to a lab where it will be created in just two or three weeks. The splint itself can be created to control foot motion that is unique to the wearer and will fit snugly to the leg with little or no padding. Because this type of splint is custom made it will usually cost significantly more than a commercial model. Most insurance companies will pay for part or all of the cost of a custom model, with written proof of medical necessity by the ordering physician. Fasciitis braces aren’t designed for walking and can cause a fall should you try to ambulate with it on. Most insurance companies will pay for part or all of the cost of a custom model, with written proof of medical necessity by the ordering physician. Pain on Side of Foot: Pain Management and Recovery Pain on side of foot can be caused by a number of issues. Initially, the type of activity you were engaged in during the onset of the pain can help your doctor to determine the root cause. This type of pain can be on the inside or outside of the foot and can often radiate to other areas of the foot without proper treatment. Pain on Side of Foot: Stress Fractures and Sprains A common cause of pain on the side of the foot is a stress fracture. A stress fracture occurs when there is a small break on one of the bones found in the foot. This can be caused by tripping, running or repetitive sports activities. Where the pain is located primarily depends on which bone is affected. A fracture of the metatarsals can cause pain on either side of the foot. This type of pain usually begins as mild and can gradually worsen without treatment. According to studies, one of the most common cause of pain in this area of the foot is caused by an ankle sprain. A sprain can affect ligaments in the foot which can become damaged if the patient rolls the foot inwards. Almost forty percent of patients who have sprained their ankle will experience recurring issues and can require physical therapy in order to learn how to avoid reinjuring the ankle and foot. Common signs of a sprain include swelling, bruising, pain and limited mobility. Another common cause of outside foot pain is known as peroneal tendinitis. This condition develops as a result of repetitive tension through the tendons of the foot, leading to degeneration, irritation, limited mobility, pain and swelling. It’s usually caused by overuse and is frequently diagnosed in runners. This type of condition can come on slowly and increase in intensity over time. If left untreated or if the patient fails to rest the injured foot, surgery may be necessary. Tarsal coalition is caused by two of the foot bones connected via an excess bar of bone. This is a fairly rare condition that only affects approximately one out of a hundred people. The onset of symptoms is described as sudden and can result in extreme pain and cramps. It can also lead to other problems with the foot including frequent ankle sprains. Surgery is usually required if casting the foot fails to show improvement in symptoms. A bunion can also cause pain in the side of the foot. This type of pain occurs when the big toe is turned inward causing the bone at the base of the big toe to stick out, resulting in inflammation, pain that runs along the side of the foot, and swelling. The occurrence of bunions can be blamed on genetics, especially in families where joint flexibility is common. This condition is commonly experienced in people with rheumatoid arthritis or gout. When to see your Podiatrist Medical attention is necessary if you experience severe foot pain, redness, swelling or a change in mobility. Often, foot injuries will heal in a matter of days with proper rest, elevation and icing the area several times a day. Plantar Fasciitis Surgery: Is it Worth it? Plantar fasciitis surgery is an effective treatment option that’s designed to reverse the effects of plantar fasciitis. However, this type of surgery is not commonly used to treat this condition, with only about six percent of patients suffering from plantar fasciitis qualifying for this option. The majority of patients with this diagnosis can fully recover with routine treatment, in rare cases surgery may be necessary. Plantar Fasciitis Surgery: When all other Treatment Fails This type of surgery is only considered after all other routine treatments have failed. Typically, initial treatment involves the use of orthotics, an effective method that can provide immediate pain relief. Other treatments include wearing a night splint and the use of anti-inflammatory medication. However, these methods can fail to minimize pain so more serious treatment may be needed in the form of extracorporeal shock therapy or monthly cortisone injections. Certain criteria must be met before surgery is a viable option. To start, the patient should have a case that’s serious enough to last for more than nine months. Exercises specifically designed to reduce symptoms should also be done on a daily basis without success before surgery is considered. Last of all, the patient must be made aware of the risks involved with surgery. While not considered a serious procedure, complications can arise during the healing period that will prolong recovery. What you can expect after Surgery for Heel Pain Following surgery, several complications can arise that can prevent or prolong a full recovery. The patient may experience numbness in certain areas of the foot if nerves are damaged during the procedure. Infection is also a possibility and a risk that’s common with any surgery. Lastly, after surgery, the patient may still experience the same type of pain around the heel. The surgical procedure for plantar fasciitis often involves open surgery. During the procedure, the specialist will make cuts along the ligament, which in turn relieves tension that has built up. The surgeon will begin by making an incision around the heel pad. If damaged portions of the tendon need to be located endoscopic surgery may be necessary. After the surgery is complete the patient will need to wear a brace or cast which will reduce weight on the heel, allowing the tissue to heal. It can take several weeks before the patient is able to bear weight, making their mobility very limited. Usually, it takes three to four months for the patient to regain full activity in the foot. Every surgery will have its risks. The patient will need to consider the benefits of surgery and the slow recovery time before making a final decision. Most patients who undergo this procedure will experience a full recovery. If mobility complications arise during the healing process physical therapy may be needed in order to assist with regaining strength in the foot and improving mobility. Benefits of Plantar Fasciitis Socks People suffering from severe heel pain caused by plantar fasciitis can benefit from wearing compression socks, also referred to as plantar fasciitis socks. These socks are designed to provide extra pressure along the ligament and can offer instant pain relief. They’re especially effective for patients who spend a lot of time on their feet at work. How to Wear Plantar Fasciitis Socks These socks should be worn with the proper orthotic support and arch support shoes. Often, people will opt for the compression socks over night splints because they don’t interfere with a good night’s rest. The compression socks can provide a snug fit, which keeps the foot stable and the fascia ligament comfortably stretched. The result is a significant reduction in morning pain. They can also be worn all day and night, allowing for around the clock treatment. Shopping for Compression Socks for Plantar Fasciitis Treatment When shopping around for the right pair of compression socks, make sure that they feature arch and heel compression support. Never wear socks that are too tight before it can restrict circulation and cause swelling. Compression foot sleeves by FS6 feature six zones of compression along the ankle, running down to the ball of the foot. These socks are also designed to promote circulation, which can speed up the healing time. They can be worn alone or under socks and are easy to put on and remove. Some users had complaints that the socks were too tight and caused increased heel tenderness. Feetures compression socks utilize unique compression zone technology that stabilizes the fascia ligament, promoting circulation and reducing discomfort caused by plantar fasciitis. Many consumers have reported that they’re comfortable enough to sleep in, which is a huge bonus for users with severe pain. Compression socks by Sox Multisport are designed for more active consumers and offer more flexibility and room to move without the tight restricted feeling you can expect from other brands of compression hose. They’re also designed to improve blood flow and feature quick-dry material and provide mid-foot support. The sleek design allows the socks to be worn day and night, but they may not provide enough arch support for some consumers. Strassburg compression socks feature more of a night splint design. These socks are designed to keep the foot in a stretched position during sleep, in order to relieve morning pain. The flexibility and soft material make these socks a good alternative for patients who found boot splints uncomfortable to sleep in. While they’re more comfortable than a boot and allow the wearer to still wiggle their toes, they can also pull on them, causing numbness. Some users also reported that these socks were much too warm and caused excessive sweating throughout the night. The choices for socks designed to treat plantar fasciitis are somewhat limited, but the models available are all designed to prevent severe pain that occurs with the first steps of the day. They’re also covered by many insurance companies and can be found online or at pharmacies and medical supply stores. Insoles for Plantar Fasciitis for Pain Relief Insoles for plantar fasciitis are designed to realign the feet into a more neutral position. This type of treatment can help minimize pain commonly associated with plantar fasciitis and offers more arch support while relieving tension in the feet. These insoles should be used in addition to the type of footwear that promotes good posture. Insoles for Plantar Fasciitis: Do I Need Inserts? Plantar fasciitis involves the inflammation of the plantar fascia ligament and it’s the most common cause of heels spurs or generalized heel pain. This thick ligament runs from the heel to the ball of the foot and is designed to provide support to the arch while also acting as a natural shock absorber. Individuals who work in positions that require them to stand on their feet for long periods of time and people who suffer from obesity are more at risk for plantar fasciitis. People with fallen arches or individuals who engage in any type of activity that puts undue stress consistently on the feet are also at risk. What most people don’t know is that all insoles will go through a breaking-in period, much like a new pair of shoes. Some models may not adjust to the contours of your feet as easily as others. Typically, insoles can feel awkward or uncomfortable for the first one to two weeks of wear. Fortunately, there is a wide variety of orthotic insoles to choose from. All of which are designed to provide support while increasing shock absorption and correctly positioning the foot. Depending on the severity of your condition, you can purchase a commercial pair of orthotics or have a custom pair made. Custom-made orthotics will run on the expensive side, however some insurance companies will cover part or all the cost depending on your health plan and the medical necessity of these inserts. Commercial pairs are significantly cheaper and don’t require a prescription to purchase. They can be found in pharmacies, online or through medical supply stores. How to choose the right Orthotics A good pair of orthotics will allow you to wear your favorite shoes comfortably. Active inserts are designed to provide improved control for individuals who participate in sports or for runners. Slim fit orthotics can be a little pricey, but they’re designed for everyday use and can be worn in almost any type of shoe with heels that are up to three inches high. Gel heel inserts are a type of orthotic that’s designed for walking and everyday activity. This type of insert is more recommended for light activity. Shock absorber orthotics is designed for cross training and provide the most support. They also have a reputation for preventing the occurrence of plantar fasciitis. Inserts known as relief orthotics are designed for everyday use and can provide moderate support for the avid walker. They can be used in most types of shoes including dress shoes or work boots. The type of insert you choose will ultimately depend on your activity level or the type of job you have. Manual labor or positions that require you to spend a significant amount of time on your feet require more padding and support. Runners will need special orthotics that are more directed