Formative Assesments
advertisement

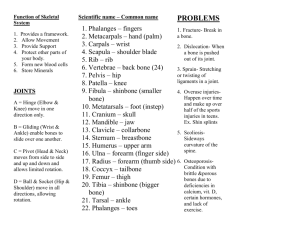
The human skeleton is initially made of cartilage but as development progresses most of this is replaced by bone. The remaining cartilage exists in areas where flexible support is needed. Cartilage contains chondrocyte cells surrounded by a jellylike matrix that is made mostly of water and fibers which combined allow cartilage to spring back to its original shape after being compressed. Remember that cartilage does not have nerves or blood vessels which means it depends on the surrounding dense irregular tissue (perichondrium) for nutrients through diffusion. This limits the thickness of cartilage. The 3 types of cartilage reviewed in the previous section are used in different location. • Hyaline cartilage includes; 1) articular cartilage which covers the ends of most bones at joints; 2) costal cartilage, which connects the ribs to the sternum; 3) respiratory cartilage, which reinforces air passageways; 4) nasal cartilage, which supports the external nose. • Elastic cartilage: the ear and epiglottis (flap that prevents food from entering the lungs). This type provides strength and stretchability. • Fibrocartilage: in the knee and between the vertebrae where strong support and resistance of heavy pressure is required. The axial skeleton: bones of the skull, vertebral column, and rib cage. Generally these bones protect, support, and carry other body structures. The appendicular skeleton: bones of the upper and lower limb girdles and limbs. These bones are mainly used for locomotion. Beyond the classification based on region, most bones are classified based on shape. • Long Bones: bones that are longer than they are wide (note named for shape not size). The bones of the limbs except the patella and the bones of the wrist and ankle are long bones. • Short Bones: roughly cube shaped. These include the bones of the wrist and ankle. • Sesamoid Bone: special type of short bone that forms in a tendon. These vary in size and number in different individuals and while some clearly act to alter the directional pull of the tendon the functions of others are not known. The most prominent example is the patella. • Flat Bone: These include the sternum, scapulae, ribs, and most skull bones. These bones are thin, flattened bones that are normally curved. • Irregular Bones: Bones that do not fit into the other categories. These include the hip and vertebrae. Support: create a framework that supports tissues and cradles soft organs. Protection: fused skull bones, vertebrae that surround the spinal cord, and the rib cage all protect the structures they contain. Movement: Skeletal muscles that attach to the bones by tendons use them as levers to move the body. Mineral Storage: Bone acts as a reservoir for minerals (most important being calcium and phosphate). These minerals are released into the blood stream as needed which carries the minerals to any part of the body. Blood cell formation: Hematopoiesis (the creation of blood cells) occurs in the marrow cavity of certain bones. Bones contain several types of tissues which makes them organs Gross Anatomy • Bone markings: Bones are rarely smooth; instead they have projections, depressions, and openings that serve as the site of muscle/ligament/tendon attachment, as joint surfaces, or as conduits for blood vessels and nerves. **Chart on pg 179/119 small book you need to know** Bone textures: The outer layer that in dense is called compact bone. The inner bone is a honeycomb of branches called trabeculae. In living bone the open spaces between these branches are filled with red and yellow bone marrow. Red marrow makes blood cells while yellow marrow is a fat reserve. This inner layer is called spongy bone. • Structure of a long bone: Diaphysis: The shaft of the bone. The outer layer is a thick collar of compact bone with a center medullary cavity which in adults is filled with yellow bone marrow. In infants the marrow is red and forms blood cells. Epiphyses: Bone ends that are normally expanded. The outer layer is compact bone while the inner layer in spongy bone. The joint surface is covered with hyaline cartilage which cushions the bone during joint movement. Between the diaphysis and the epiphysis there is an epiphyseal line. This used to be a disc of hyaline cartilage called the epiphyseal plate that grew during childhood to lengthen the bone. Periosteum: A double layer membrane that covers the external surface of the bone. The outer layer called the fibrous layer is dense irregular connective tissue while the inner layer called the osteogenic layer is composed of cells that make (osteoblast) and break down (osteoclast) bone. This membrane provides anchoring points for the tendons and ligaments. Endosteum: Internal lining of the medullary cavity • Structures of flat, short, and irregular bones These bones have a periosteum that covers compact bone which covers the spongy bone within and while they contain bone marrow there is no centralized marrow cavity. Microscopic Anatomy: • Inorganic calcium salts in the matrix allow bone to have exceptional strength while organic collagen fibers provide bone with some flexibility and great tensile strength. • Mature bone cells (osteocytes) exist in tiny cavities in the matrix called lacunae which are arranged in concentric circles called lamellae around a central canal called the Haversian canal. Together the circles and canal make an ostean or Haversian system. Bone has a maze of passageways called conaliculi for carrying nerves and blood vessels which provide the cells with nutrients and a way to get rid of waste that allows bone to be well nourished in spite of its hard matrix. This also allows bone to heal quickly and well. The bone and the rest of the body communicate through a Volkmann’s canal that runs into the bone at a right angle. Formation: With the exception of some flat bones, bones form by replacing a hyaline cartilage model formed during the embryonic stage in a process called ossification. This involves two major phases. • The hyaline cartilage model is covered with bone matrix created by bone forming cells called osteoblasts. The enclosed hyaline cartilage model is digested away making a medullary cavity. Most “bones” of an embryo are converted to bone with two execptions: the articular cartilage that covers bone ends which exists for life to reduce friction and the epiphyseal plates which allow bones to increase in length through childhood. Growth: bones grow in two directions. • Increase in length in achieved by the epiphyseal plate. New cartilage is created on the surface of the plate that is furthest from the medullary cavity and on the surface of the articular cartilage while on the opposite side of each location “old” cartilage cells are broken down and replaced by boney matrix. • Increase in width is achieved by osteoblasts in the periosteum adding bone tissue while osteoclasts in the endosteum remove bone from the inner surface. This process is called appositional growth and is controlled by growth horomone and sex horomones (during adolescence) until the epiphyseal plates are completely converted to bone in the late teens. Remodeling: 2 Aspects • Calcium deposits in bone are determined by the levels in the blood. When calcium levels are low the parathyroid gland releases a hormone (PTH) that encourages the breakdown of bone releasing the mineral into the blood. When levels are high it is deposited into the bone as calcium salt. At locations where bones need to be thicker or form larger projections to increase their strength where muscles attach osteoblasts lay down a new matrix and become trapped within it. On the other hand if areas of bone are not subject to stress by muscles or gravitational pull the bone loses mass and atrophies. **So the hormone released by the parathyroid determines if bone needs to be broken or made and the pull of muscles and gravity will determine where the breakdown or creation occurs** Types of fractures • Closed/Simple Fracture: The bone breaks cleanly but does not break the skin • Open/Compound Fracture: The broken bone protrudes through the skin • Comminuted: Bone breaks into many pieces come in brittle bones of elderly • Compression: Bone is crushed which is common in porous bone • Impact: Broken ends are forced into each other such as when you try to catch yourself in a fall • Spiral: Ragged break occurs when twisting forces are applied to the bone such as in sports • Greenstick: Bone does not break all the way through, common in the more flexible bones of children. Treatment of fractures: • Reduction is the realignment of the broken ends of the bone. In closed fractures the bones are coaxed back into position. In an open reduction surgery is performed and then wires or pins are used to hold the bones in place. After reduction the break is immobilized by a cast or traction. Healing of a simple fracture should take 6-8 weeks. Large bones and bones of the elderly take longer to heal. Bone repair includes 4 events • Blood vessels ruptured when a bone breaks resulting in a blood-filled swelling called a hematoma. The bone cells that are deprived of nutrients die • New capillaries (granulation tissue) grow into the clotted blood at the site of damage and dead cells are disposed of using phagocytosis. Connective tissue cells form a mass of repair tissue called the fibro cartilage callus that contains cartilage matrix, bony matrix, and collagen fibers to act as a splint closing gap. • More osteoblast and osteoclast migrate to the site gradually replacing the fibro cartilage with spongy bone (bony callus) • The bony callus is remodeled in response to stress exerted by muscles to form a permanent “patch” at the fracture site. Includes the skull, vertebral column and the thorax. It is responsible for supporting the head, neck, trunk and protecting the brain, spinal cord and organs of the thoracic cavity. Most of the bones of the skull (except the mandible) are flat bones that are firmly united by interlocking joints called sutures. The cranium encloses and protects the brain and is composed of eight large flat bones. The facial bones hold the eyes and the facial muscles to change expressions Cranium: • Frontal bone: The forehead, brow ridge and upper eye orbit • Parietal bones: Pair of bones that cover the superior and lateral areas. The suture where they meet at the midline of the skull is the sagittal suture. The one that connects these to the frontal bone is the coronal suture • Temporal bones: A pair of bones that lie inferior to the parietal bones and are joined to them by the squamous suture. Important bone markings of these bones include: External auditory meatus: canal that leads to the eardrum and middle ear. Styloid process: Sharp, needlelike projection that is inferior to the external auditory meatus. Place of attachment for many neck muscles. Zygomatic process: Thin bridge that joins with the cheek bone • Mastoid process: Rough projection that is posterior and inferior to the external auditory meatus that is full of air cavities and is a place of attachment for some neck muscles. • Jugular foramen: An opening between the occipital and temporal bones that allows the jugular through to drain blood from the brain. • Carotid canal: Allows the internal carotid artery through to supply most of the brain with blood. Occipital Bone: From the floor and back wall of the skull. It joins the parietal bones at the lambdoid suture. • Foramen magnum: Opening that allows the spinal cord to connect with the brain • Occipital condyles: On either side of the foramen magnum which rest on the first vertebra. Sphenoid bone: Spans the width of the skull forming part of the floor of the cranial cavity. At the midline is a depression called a sella turcica which holds the pituitary gland in place. Posterior to the sella turcica is the foraman ovale which is a large opening that allows the cranial nerves to pass to chewing muscles of the sphenoid bone. Ethmoid bone: Very irregularly shaped bone anterior to the sphenoid bone. Forms the roof of the cavity and the medial wall of the orbits Facial Bones: • Maxillae: Two bones that fuse to join the upper jaw and the hard palate of the nose. • Palatine Bones: Pair of bones that form the posterior hard palate. Failure of the fusion of theses bones causes a cleft palate. • Zygomatic bones: Cheek bones that form the lateral wall of the orbits • Lacrimal bones: Bones on the medial wall of the orbits that have a groove to allow for the passage way of tears • Nasal bones: Form the bridge • • • • of the nose Vomer bone: Forms most of the nasal septum Inferior conchae: Project from the lateral wall of the nasal cavity Mandible: Lower jaw that holds the bottom teeth and joins the temporal bone at the only free moving joint of the skull. Hyoid bone: Only bone of the body that does not articulate to another bone. It is a movable base for the tongue and attachment point for the neck muscles that raise and lower the larynx when swallowing or speaking. Fetal Skull: There many differences between an infant skull and an adult • The infants face is small in comparison to the cranium • The skull itself is a quarter of the body length while in adults it is an eighth of the body length. The bones of the skull are not fully fused (fibrous membranes remain between them). These “soft spots” are called fontanels with the two largest being the anterior and posterior fontanels. This allows the skull to be slightly compressed during birth and the brain to grown in early infancy. They are gradually converted to bone and should be fully fused by age 2. Composed of 33 separate bones before birth. 9 of these bones will fuse together to form the 2 composite bones of the sacrum and coccyx. The other 24 single bones are divided among region: 7 cervical vertebrae, 12 thoracic, and 5 lumbar. The vertebrae are irregular bones that posses a central cavity that the spinal cord runs through. Each vertebrae is separated by a pad of fibrocartilage called the intervertebral discs which cushion the bones and absorb shock. As a person ages these discs begin to dry out and ligaments become weaker which predisposes older people to herniated discs which can cause a numbness and pain. The curves of the spine are divided into two groups. The curve in the thoracic and sacral regions are primary because they exist before birth. The cervical curve develops when a baby begins to raise its head and the lumbar curvature develops when baby starts to walk. Both are secondary curvatures. The 3 main types of abnormal spine curvature are scoliosis, kyphosis, and lordosis. These can result from poor posture, disease, unequal pull of muscles, or could be congenital. Cervical Vertebrae: Identified as C1-C7. The first two have specific functions so they are different. The atlas (C1) has no body, instead it has large depressions that receive the occipital condyle of the skull. This joint allows you to nod. The axis (C2) acts as a pivot for rotating the atlas. The joint between C1 and C2 allows you to turn your head side to side. The other typical vertebrae have an additional feature called a transverse process which allows arteries to pass through on the way to the brain. Thoracic vertebrae: identifies as T1-T12 are all typical vertebrae but there is a facet on the transverse process for the ribs to articulate and the spinous process is long and hook downward causing the bone to look like a giraffe’s head from the side. Lumbar vertebrae: identified as L1-L5 they have massive block like bodies and are the sturdiest of the vertebrae. Sacrum: made from five fused vertebrae. Articulates superiorly with the L5 vertebrae, inferiorly with the coccyx and laterally with the hip bones. The surface has median sacral crests which are the fused spinous processes of the original vertebrae. The sacral canal is an extension of the vertebral canal for the spinal cord. Coccyx: formed by the fussion of 3-5 irregular vertebrae. This is the remnant of a tail. Sternum: flat bone that forms from the fusion of the manubrium, the body, and the xiphoid process. The first seven ribs attach to the sternum and it has three important markings: • Jugular notch: concave upper border of the manubrium that is easily palpated. • Sterna angle: place where the manubrium and body meet at a slight angle creating a transverse ridge that provides a reference for counting ribs to find the second intercostal space to listen to certain heart valves. • Xiphisternal joint: point of fusion between the sterna body and the xiphoid process. Ribs: there are twelve pairs of ribs. The first seven are called true ribs because they articulate to the sternum directly. Then there are three pairs that articulate indirectly and two pairs that are called floating ribs because they do not articulate at all. These five pairs are called false ribs. Remember all ribs articulate to a vertebra. The intercostals spaces are filled with muscle that aids in breathing. Clavicle/collarbone: attaches to the sternum medially and the scapula latterly where it helps to form the shoulder joint. It acts as a brace to hold the arm away from the thorax and helps to prevent the dislocation of the shoulder. Scapulae: loosely held in place by muscles, the shoulder blade has two processes: the anterior acromion process that connects to the clavicle and the posterior coracoid process which anchors some arm muscles. It also has a glenoid cavity which is the shallow socket that receives the head of the arm bones. The girdle allows the arm to have exceptionally free movement due to • Each girdle attaches to the axial skeleton at only one point (clavicle to sternum) • The loose muscle attachment of the scapula allows it to slide with muscle movement • The cavity is shallow and the joint is poorly reinforced by ligaments Humerus (arm bone): the typical long bone that forms the arm has many distinguishing marks. The greater and lesser tubercles opposite the head of the bone are the location of muscle attachment. At the midpoint of the shaft is the deltoid tuberosity which is where the deltoid muscle of the shoulder articulates. The radial groove runs down the posterior shaft and marks the path of the radial nerve (major nerve of the limb). At the distal end the medial trochlea and lateral capitulum are processes that articulate with the bones of the forearm. Above the trochlea are two depressions which hold the processes of the same name of the ulna in a pliers-like joint to allow the elbow to bend. The anterior depression is the coronoid fossa and the posterior is the olecranon fossa. Forearm: the two bones of the forearm are the radius on the thumb side and the ulna at the pinky. They are connected at both ends by the radioulnar joints and down their entire length by a flexible interosseous membrane. The radius articulates with the humerus and just below the head is the radiul tuberosity where the tendon of the bicep attaches. The ulna has the two processes that fit the depressions in the humerus and between them is the trochlear notch. Hand: • Carpal: two irregular rows of four bones that make up the wrist or carpus that are held together tightly by ligaments. • Metacarpals: make up the palm of the hand and are number from the thumb as 1-5. • Phalanges: each finger has three phalanges (proximal, middle, and distal) while the thumb has two (proximal and distal) The coxal bones (hip bones) are attached securely to the axial skeleton and the socket that receives the thigh bone is deep and heavily reinforced by ligaments. Supporting the weight of the entire upper body and protecting the reproductive organs, the bladder, and the lower parts of the large intestines are two main functions of the pelvis. The coxal bone is formed by the fusion of three bones: the ilium, ischium, and pubis. • Ilium: connects to the sacrum and forms the upper flaring part of the hip. • Ischium: the “sit down” bone supports the bodies weight when sitting. The ischium has a tuberosity which forms the majority of the base, a spine that narrows the pelvic outlet, and the greater sciatic notch which allows the sciatic nerve and blood vessels passage to the thigh. • Pubis: the most anterior part of the coxal bone. The two pubis bones fuse to for the cartilaginous joint called the pubic symphysis. • All three bones fuse to form the acetabulum which receives the head of the thigh bone. The pelvic bones of the male and female have structural differences to allow for child birth. The inlet is more circular, the pelvis is shallower, the iliac flare is more lateral, the sacram is shorter and less curved, the ischial spines are shorter, and the pubic arch is more rounded in a female. Femur (thigh): the strongest and heaviest bone of the body. The head of the femur articulates securely with the acetabulum of the pelvis. The neck of the femur is thinner and a common fracture site in the elderly. The femur slants medially so that the knee is in line with the bodies center of gravity. Leg: the tibia and fibula which are connected along their lengths by an interosseous membrane form the leg. The tibia (shin bone) is larger and more medial. The tibial tuberosity is the site of attachment for the patellar (knee cap) ligament. Foot: supports the bodies weight and acts as a lever that allows the body to move forward. The foot has three types of bones. • Tarsuls: the seven bones that create the posterior half of the foot. Most body weight is carried by the calcaneus (heel bone) and the talus (ankle). • Metatarsuls: five bones that form the sole of the foot. • Phalanges: the fourteen bones that make up the toes. The large toe contains two (distal and proximal) while the other toes contain three (distal, middle, and proximal). Function: hold bones together securely while also allowing mobility. Functional types of joints: • Synarthroses: immovable joint such as those of the cranium. • Amphiarthroses: slightly moveable joint such as the spine. • Diarthroses: freely movable joints such as those of the limbs. Structural classification of joints: • Fibrous joints: bones are united by fibrous tissue such as the sutures of the skull. • Cartilaginous joints: bones are connected by cartilage. Slightly movable joints that fall into this category are the pubic symphysis and the interverbral joints. The immovable examples include the cartilage that attaches the true ribs to the sternum and the cartilage found in the epiphyseal plates of the growing long bones. • Synovial joints: the bones are separated by a fluid filled cavity. All of these joints have articular cartilage that covers the end of the bones, the joint is enclosed by a sleeve of fibrous connective tissue, a cavity that contains synovial fluid, and reinforcing ligaments. These joints can be further classified based on shape Plane joint: articulating surfaces are flat and the joint is able to slide but not rotate (nonaxial) such as the joints between the bones of the wrist. Hinge joints: one bone fits into the “trough” of another bone. Angular movement within one plane is allowed such as the elbow and the joints of the phalanges. Pivot joint aka gliding joints: the bones fit together like a hinge point but are only allowed to rotate along the long axis. The best example is the joint between the bones of the lower leg. Condyloid joints aka ellipsoid joint: allows movement side to side and back to front but no rotation around the long axis such as the joints of the knuckles. Saddle joints: both bones are saddle shaped. This joint allows essentially the same movement as the condyloid joint with the best example being the joint between the carpal and metacarpal of the thumb (twiddle your thumbs) Ball and socket: allows movement on all axes such as the shoulder and hip.