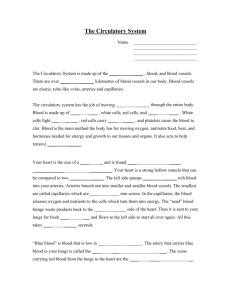
Ch 17-19 The Circulatory (Cardiovascular) System

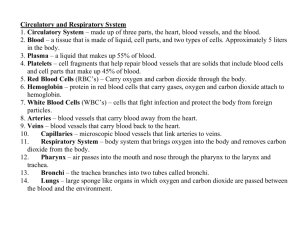
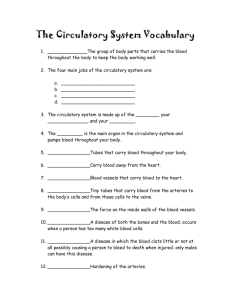
What is the role of the circulatory system?
Maintain internal homeostasis
What are some things that would need to be balanced within the body?
Maintain temperature, O
2 conc., blood glucose, etc.
Deliver and remove nutrients and gases to and from the body
Maintain cells in a fluid environment that allows for these exchanges to occur
To do all of this, the circulatory system must come into contact with most tissues in the human body.
Which of the organisms below have transport systems?
Which do not? Explain your reasoning!
How can the paramecium and hydra thrive with no circulatory system?
Open vs. Closed Systems
Which system seems more efficient? What are your reasons?
Open Circulatory System
Body fluid is pumped through open ended vessels and bathes organs.
Occurs in insects, crabs, and other animals that have exoskeletons
Body fluid is circulated by the heart
How efficient is this? Why?
Why Do Bugs Make
Such a Mess?
Closed Circulatory Systems
Blood is confined to major vessels which branch into smaller vessels that carry blood to organs.
Blood is pumped through the body by the heart.
Blood flow is faster than in an open system
If you are a cheetah, what type of circulatory system would you need? Why?
Several types of blood vessels exist in the circulatory systems of vertebrates.
What are the three types of blood vessels?
Arteries, capillaries, & veins
Blood Vessels
Blood Vessels
Blood travels through three types of vessels:
What are some differences you notice between these vessels?
1. Arteries 2. Capillaries 3. Veins
Blood Vessels
Blood is carried in a closed system of vessels that begins and ends at the heart
The three major types of vessels are arteries, capillaries, and veins
Arteries carry blood away from the heart, veins carry blood toward the heart
Capillaries contact tissue cells and directly serve cellular needs
Elastic (Conducting) Arteries
Thick-walled arteries near the heart; the aorta and its major branches
Large lumen allow lowresistance conduction of blood
Contain elastin in all three tunics
Withstand and smooth out large blood pressure fluctuations
Allow blood to flow fairly continuously through the body
Arteries of the Head and Neck
Arteries of the Brain
Arteries of the Upper Limbs and Thorax
Arteries of the Abdomen
Arteries of the Lower Limbs
Muscular (Distributing) Arteries and
Arterioles
Muscular arteries – distal to elastic arteries; deliver blood to body organs
Have thick tunica media with more smooth muscle and less elastic tissue
Active in vasoconstriction
Arterioles – smallest arteries; lead to capillary beds
Control flow into capillary beds via vasodilation and constriction
Capillaries
Capillaries are the smallest blood vessels
Walls consisting of a thin tunica interna, one cell thick
Allow only a single
RBC to pass at a time
Pericytes on the outer surface stabilize their walls
There are three structural types of capillaries: continuous, fenestrated, and sinusoids
Capillary Beds
A microcirculation of interwoven networks of capillaries, consisting of:
Vascular shunts – metarteriole –thoroughfare channel connecting an arteriole directly with a postcapillary venule
True capillaries – 10 to
100 per capillary bed, capillaries branch off the metarteriole and return to the thoroughfare channel at the distal end of the bed
Venous System: Veins
Veins are:
Formed when venules converge
Composed of three tunics, with a thin tunica media and a thick tunica externa consisting of collagen fibers and elastic networks
Capacitance vessels (blood reservoirs) that contain 65% of the blood supply
Venous System: Veins
Veins have much lower blood pressure and thinner walls than arteries
To return blood to the heart, veins have special adaptations
Large-diameter lumens, which offer little resistance to flow
Valves (resembling semilunar heart valves), which prevent backflow of blood
Venous sinuses – specialized, flattened veins with extremely thin walls (e.g., coronary sinus of the heart and dural sinuses of the brain)
Factors Aiding Venous Return
What is the purpose of the valves found in veins?
Keep blood flowing toward the heart.
So what happened here?
Why must the capillary walls be so thin?
So materials can diffuse through the wall for exchange.
Veins of Systemic Circulation
Veins of the Head and Neck
Veins of the Brain
Veins of the Upper Limbs and Thorax
Veins of the Abdomen
Veins of the Pelvis and Lower Limbs
Blood Vessels - Summary
Arteries : carry blood away from the heart, thickest walls
Veins : carry blood toward the heart, thinner walls, one-way valves
Capillaries : extremely thin walls, sites of exchange in lungs and body cells
ARTHERIOSCLER
OSIS=The narrowing of blood vessels due to build- up of fats that turn into plaque on the artery and vein walls.
How do these three different circulatory systems compare?
What are systemic capillaries?
Capillaries that are located throughout the body
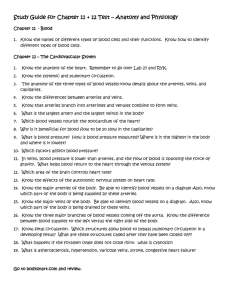
Circulation in Fish
How many chambers does the heart have?
-2 chambered heart
How many loops does this circulatory system have?
1
Blood is oxygenated in gills and travels to the body
Heart
gills
systemic
heart
Circulation In Amphibians and Reptiles
How many chambers does the reptilian heart have?
-3 chambered heart
How many loops does this circulatory system have?
2 (double loop circulatory system)
Trace the blood flow through the body…
Heart
lungs
heart
systemic
Where is the inefficiency in the amphibian
3-chambered system?
The Heart and Blood Flow in Mammals
How many chambers are there?
-4 chambered heart
How many loops?
2
Trace the blood flow through the body…
Heart lung heart systems
How is this heart more efficient than the reptilian heart?
Heart Animation
Heart Anatomy
The Circulatory System
Coverings of the Heart: Physiology
The pericardium:
Protects and anchors the heart
Prevents overfilling of the heart with blood
Allows for the heart to work in a relatively frictionfree environment
Heart Wall
Epicardium – visceral layer of the serous pericardium
Myocardium – cardiac muscle layer forming the bulk of the heart
Fibrous skeleton of the heart – crisscrossing, interlacing layer of connective tissue
Endocardium – endothelial layer of the inner myocardial surface
External Heart: Major Vessels of the Heart (Anterior View)
Vessels returning blood to the heart include:
Superior and inferior venae cavae
Right and left pulmonary veins
Vessels conveying blood away from the heart include:
Pulmonary trunk, which splits into right and left pulmonary arteries
Ascending aorta (three branches) – brachiocephalic, left common carotid, and subclavian arteries
External Heart: Major Vessels of the
Heart (Posterior View)
Vessels returning blood to the heart include:
Right and left pulmonary veins
Superior and inferior venae cavae
Vessels conveying blood away from the heart include:
Aorta
Right and left pulmonary arteries
Gross Anatomy of Heart: Frontal Section
Atria of the Heart
Atria are the receiving chambers of the heart
Each atrium has a protruding auricle
Pectinate muscles mark atrial walls
Blood enters right atria from superior and inferior venae cavae and coronary sinus
Blood enters left atria from pulmonary veins
Ventricles of the Heart
Ventricles are the discharging chambers of the heart
Papillary muscles and trabeculae carneae muscles mark ventricular walls
Right ventricle pumps blood into the pulmonary trunk
Left ventricle pumps blood into the aorta
Pathway of Blood Through the Heart and Lungs
Right atrium tricuspid valve right ventricle
Right ventricle pulmonary semilunar valve pulmonary arteries lungs
Lungs pulmonary veins left atrium
Left atrium bicuspid valve left ventricle
Left ventricle aortic semilunar valve aorta
Aorta systemic circulation
Pathway of Blood Through the Heart and Lungs
Coronary Circulation: Arterial Supply
Coronary Circulation: Venous Supply
Heart Valves
Heart valves ensure unidirectional blood flow through the heart
Atrioventricular (AV) valves lie between the atria and the ventricles
AV valves prevent backflow into the atria when ventricles contract
Chordae tendineae anchor AV valves to papillary muscles
Heart Valves
Aortic semilunar valve lies between the left ventricle and the aorta
Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk
Semilunar valves prevent backflow of blood into the ventricles
Heart Valves
Heart Valves
Atrioventricular Valve Function
Semilunar Valve Function
Microscopic Anatomy of Heart Muscle
The Heart
The Mammalian Heart
The Cardiac Cycle
The heart is composed of cardiac muscle and each beat is a muscle contraction and relaxation
Contraction = Systolic Pressure
Relaxation = Diastolic pressure
How is blood pressure written?
Systolic / diastolic
Heart Physiology: Sequence of
Excitation
Heart Excitation Related to ECG
Extrinsic Innervation of the Heart
Heart is stimulated by the sympathetic cardioacceleratory center
Heart is inhibited by the parasympathetic cardioinhibitory center
Electrocardiography
Heart Sounds
Heart sounds (lub-dup) are associated with closing of heart valves
First sound occurs as AV valves close and signifies beginning of systole
Second sound occurs when SL valves close at the beginning of ventricular diastole
Cardiac Cycle
Cardiac cycle refers to all events associated with blood flow through the heart
Systole – contraction of heart muscle
Diastole – relaxation of heart muscle
Preload and Afterload
Regulation of Heart Rate: Autonomic
Nervous System
Sympathetic nervous system (SNS) stimulation is activated by stress, anxiety, excitement, or exercise
Parasympathetic nervous system
(PNS) stimulation is mediated by acetylcholine and opposes the SNS
PNS dominates the autonomic stimulation, slowing heart rate and causing vagal tone
Factors Involved in Regulation of
Cardiac Output
Blood Pressure
What is blood pressure?
The force that blood exerts against vessel walls
Is BP greater in arteries or veins?
In arteries
Find your pulse- what are you feeling here?
Pulse is measure of BP
Which would have a higher blood pressure, constricted blood or dilated vessels?
Constricted vessels
Does the BP have an effect on veins?
No- the pressure is lost in the capillaries
How, then does blood move in veins?
What is average blood pressure?
120/80 (mm Hg) of pressure on artery walls.
Which part of the heart contracts first?
The atria contract first, followed immediately by the ventricles.
Systemic Blood Pressure
The pumping action of the heart generates blood flow through the vessels along a pressure gradient, always moving from higher- to lowerpressure areas
Pressure results when flow is opposed by resistance
Systemic pressure:
Is highest in the aorta
Declines throughout the length of the pathway
Is 0 mm Hg in the right atrium
The steepest change in blood pressure occurs in the arterioles
Arterial Blood Pressure
Systolic pressure – pressure exerted on arterial walls during ventricular contraction
Diastolic pressure – lowest level of arterial pressure during a ventricular cycle
Pulse pressure – the difference between systolic and diastolic pressure
Mean arterial pressure (MAP) – pressure that propels the blood to the tissues
MAP = diastolic pressure + 1/3 pulse pressure
Blood Pressure
Cardiac Output (CO)
Volume of blood pumped/ minute
Stroke Volume (SV)
Amount of blood pumped by the left ventricle each time it contracts (about 75 mL per beat for the average person)
75 X 70 = 5250 mL/min.
CO is affected by heart rate and SV
Alterations in Blood Pressure
Hypotension – low BP in which systolic pressure is below 100 mm Hg
Hypertension – condition of sustained elevated arterial pressure of 140/90 or higher
Transient elevations are normal and can be caused by fever, physical exertion, and emotional upset
Chronic elevation is a major cause of heart failure, vascular disease, renal failure, and stroke
Hypotension
Orthostatic hypotension – temporary low
BP and dizziness when suddenly rising from a sitting or reclining position
Chronic hypotension – hint of poor nutrition and warning sign for Addison’s disease
Acute hypotension – important sign of circulatory shock
Threat to patients undergoing surgery and those in intensive care units
Hypertension
Hypertension maybe transient or persistent
Primary or essential hypertension – risk factors in primary hypertension include diet, obesity, age, race, heredity, stress, and smoking
Secondary hypertension – due to identifiable disorders, including excessive renin secretion, arteriosclerosis, and endocrine disorders
How Does Your Heart Beat?
Can you control the beating of your own heart?
No- the heart muscles contract on their own.
The heart has a pacemaker, or SA node, that maintains the heart’s rhythm.
• The pacemaker sets the tempo of the heartbeat.
Blood Composition continued ...
Diagramatic View Real Blood Cells
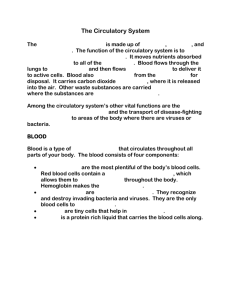
Overview of Blood Circulation
Blood leaves the heart via arteries that branch repeatedly until they become capillaries
Oxygen (O
2
) and nutrients diffuse across capillary walls and enter tissues
Carbon dioxide (CO
2
) and wastes move from tissues into the blood
Overview of Blood Circulation
Oxygen-deficient blood leaves the capillaries and flows in veins to the heart
This blood flows to the lungs where it releases CO
2 and picks up O
2
The oxygen-rich blood returns to the heart
Composition of Blood
Blood is the body’s only fluid tissue
It is composed of liquid plasma and formed elements
Formed elements include:
Erythrocytes, or red blood cells (RBCs)
Leukocytes, or white blood cells (WBCs)
Platelets
Hematocrit – the percentage of RBCs out of the total blood volume
Blood
Blood is the Liquid Tissue
55% of blood is plasma (mostly water) carries nutrients, wastes and important proteins like antibodies and clotting factors.
45% is made of cells
Red, white blood cells and platelets
Erythrocytes (RBC) contain hemoglobin and carry oxygen
Leukocytes (WBC) are usually stored in the bone marrow, and are the body’s defense system
Platelets are pieces of white blood cells that are in charge of clotting
Red blood cell
Platelet
White blood cell
Components of Whole Blood
Physical Characteristics and Volume
Blood is a sticky, opaque fluid with a metallic taste
Color varies from scarlet (oxygen-rich) to dark red
(oxygen-poor)
The pH of blood is 7.35
–7.45
Temperature is 38
C, slightly higher than “normal” body temperature
Blood accounts for approximately 8% of body weight
Average volume of blood is 5 –6 L for males, and
4 –5 L for females
Distribution
Blood transports:
Oxygen from the lungs and nutrients from the digestive tract
Metabolic wastes from cells to the lungs and kidneys for elimination
Hormones from endocrine glands to target organs
Regulation
Blood maintains:
Appropriate body temperature by absorbing and distributing heat
Normal pH in body tissues using buffer systems
Adequate fluid volume in the circulatory system
Blood plasma contains over 100 solutes, including:
Proteins – albumin, globulins, clotting proteins, and others
Nonprotein nitrogenous substances – lactic acid, urea, creatinine
Organic nutrients – glucose, carbohydrates, amino acids
Electrolytes – sodium, potassium, calcium, chloride, bicarbonate
Respiratory gases – oxygen and carbon dioxide
Erythrocytes (RBCs)
Biconcave discs, anucleate, essentially no organelles
Filled with hemoglobin
(Hb), a protein that functions in gas transport
Contain the plasma membrane protein spectrin and other proteins that:
Give erythrocytes their flexibility
Allow them to change shape as necessary
Structure of Hemoglobin
Hemoglobin
Oxyhemoglobin – hemoglobin bound to oxygen
Oxygen loading takes place in the lungs
Deoxyhemoglobin – hemoglobin after oxygen diffuses into tissues (reduced Hb)
Carbaminohemoglobin – hemoglobin bound to carbon dioxide
Carbon dioxide loading takes place in the tissues
Production of Erythrocytes
Hematopoiesis – blood cell formation
Hematopoiesis occurs in the red bone marrow of the:
Axial skeleton and girdles
Epiphyses of the humerus and femur
Hemocytoblasts give rise to all formed elements
Dietary Requirements of
Erythropoiesis
Erythropoiesis requires:
Proteins, lipids, and carbohydrates
Iron, vitamin B
12
, and folic acid
The body stores iron in Hb (65%), the liver, spleen, and bone marrow
Intracellular iron is stored in protein-iron complexes such as ferritin and hemosiderin
Circulating iron is loosely bound to the transport protein transferrin
Fate and Destruction of Erythrocytes
The life span of an erythrocyte is
100 –120 days
Old erythrocytes become rigid and fragile, and their hemoglobin begins to degenerate
Dying erythrocytes are engulfed by macrophages
Heme and globin are separated and the iron is salvaged for reuse
Fate and Destruction of Erythrocytes
Heme is degraded to a yellow pigment called bilirubin
The liver secretes bilirubin into the intestines as bile
The intestines metabolize it into urobilinogen
This degraded pigment leaves the body in feces, in a pigment called stercobilin
Globin is metabolized into amino acids and is released into the circulation
Hb released into the blood is captured by haptoglobin and phgocytized
Life Cycle of Red Blood Cells
Erythrocyte Disorders
Anemia – blood has abnormally low oxygen-carrying capacity
It is a symptom rather than a disease itself
Blood oxygen levels cannot support normal metabolism
Signs/symptoms include fatigue, paleness, shortness of breath, and chills
Anemia: Insufficient Erythrocytes
Hemorrhagic anemia – result of acute or chronic loss of blood
Hemolytic anemia – prematurely ruptured erythrocytes
Aplastic anemia – destruction or inhibition of red bone marrow
Anemia: Decreased Hemoglobin
Content
Iron-deficiency anemia results from:
A secondary result of hemorrhagic anemia
Inadequate intake of iron-containing foods
Impaired iron absorption
Pernicious anemia results from:
Deficiency of vitamin B
12
Lack of intrinsic factor needed for absorption of
B
12
Treatment is intramuscular injection of B
12
; application of Nascobal
Anemia: Abnormal Hemoglobin
Thalassemias – absent or faulty globin chain in hemoglobin
Erythrocytes are thin, delicate, and deficient in hemoglobin
Sickle-cell anemia – results from a defective gene coding for an abnormal hemoglobin called hemoglobin S (HbS)
HbS has a single amino acid substitution in the beta chain
This defect causes RBCs to become sickleshaped in low oxygen situations
Leukocytes (WBCs)
Leukocytes, the only blood components that are complete cells:
Are less numerous than RBCs
Make up 1% of the total blood volume
Can leave capillaries via diapedesis
Move through tissue spaces
Leukocytosis – WBC count over 11,000 per cubic millimeter
Normal response to bacterial or viral invasion
Granulocytes
Granulocytes – neutrophils, eosinophils, and basophils
Contain cytoplasmic granules that stain specifically (acidic, basic, or both) with Wright’s stain
Are larger and usually shorter-lived than RBCs
Have lobed nuclei
Are all phagocytic cells
Neutrophils
Neutrophils have two types of granules that:
Take up both acidic and basic dyes
Give the cytoplasm a lilac color
Contain peroxidases, hydrolytic enzymes, and defensins (antibiotic-like proteins)
Neutrophils are our body’s bacteria slayers
Eosinophils
Eosinophils account for 1 –4% of WBCs
Have red-staining, bilobed nuclei connected via a broad band of nuclear material
Have red to crimson (acidophilic) large, coarse, lysosome-like granules
Lead the body’s counterattack against parasitic worms
Lessen the severity of allergies by phagocytizing immune complexes
Basophils
Account for 0.5% of WBCs and:
Have U- or S-shaped nuclei with two or three conspicuous constrictions
Are functionally similar to mast cells
Have large, purplish-black (basophilic) granules that contain histamine
Histamine – inflammatory chemical that acts as a vasodilator and attracts other WBCs
(antihistamines counter this effect)
Agranulocytes
Agranulocytes – lymphocytes and monocytes:
Lack visible cytoplasmic granules
Are similar structurally, but are functionally distinct and unrelated cell types
Have spherical (lymphocytes) or kidneyshaped (monocytes) nuclei
Lymphocytes
Account for 25% or more of WBCs and:
Have large, dark-purple, circular nuclei with a thin rim of blue cytoplasm
Are found mostly enmeshed in lymphoid tissue
(some circulate in the blood)
There are two types of lymphocytes: T cells and B cells
T cells function in the immune response
B cells give rise to plasma cells, which produce antibodies
Monocytes
Monocytes account for 4 –8% of leukocytes
They are the largest leukocytes
They have abundant pale-blue cytoplasms
They have purple-staining, U- or kidneyshaped nuclei
They leave the circulation, enter tissue, and differentiate into macrophages
Monocytes
Macrophages:
Are highly mobile and actively phagocytic
Activate lymphocytes to mount an immune response
Formation of Leukocytes
Leukocytes Disorders: Leukemias
Leukemia refers to cancerous conditions involving white blood cells
Leukemias are named according to the abnormal white blood cells involved
Myelocytic leukemia – involves myeloblasts
Lymphocytic leukemia – involves lymphocytes
Acute leukemia involves blast-type cells and primarily affects children
Chronic leukemia is more prevalent in older people
Leukemia
Immature white blood cells are found in the bloodstream in all leukemias
Bone marrow becomes totally occupied with cancerous leukocytes
The white blood cells produced, though numerous, are not functional
Death is caused by internal hemorrhage and overwhelming infections
Treatments include irradiation, antileukemic drugs, and bone marrow transplants
Platelets
Platelets are fragments of megakaryocytes with a blue-staining outer region and a purple granular center
Their granules contain serotonin, Ca 2+ , enzymes, ADP, and platelet-derived growth factor (PDGF)
Platelets function in the clotting mechanism by forming a temporary plug that helps seal breaks in blood vessels
Platelets not involved in clotting are kept inactive by NO and prostaglandin I
2
Detailed Events of Coagulation
Hemoglobin=Is the protein attahced to the red blood cell that carries oxygen around the blood stream. It gets its help from an iron molecule.
Antigens- Substances that stimulate an immune response. They recognize foreign objects.
ABO Blood Groups
Type A (antigen A- antibody B)
Type B(antigen B- antibody A)
Type AB(antigens A and B, anibodies
A and B)
Type O (No antigens or antibodies A and B) rH factor (antigen rH-Either you have it (positive) or you don’t (negative).
ABO Blood Groups
The ABO blood groups consists of:
Two antigens (A and B) on the surface of the
RBCs
Two antibodies in the plasma (anti-A and anti-
B)
An individual with ABO blood may have various types of antigens and spontaneously preformed antibodies
Agglutinogens and their corresponding antibodies cannot be mixed without serious hemolytic reactions
ABO Blood Groups
Rh Blood Groups
There are eight different Rh agglutinogens, three of which (C, D, and E) are common
Presence of the Rh agglutinogens on RBCs is indicated as Rh +
Anti-Rh antibodies are not spontaneously formed in Rh – individuals
However, if an Rh
– individual receives Rh + blood, anti-Rh antibodies form
A second exposure to Rh + blood will result in a typical transfusion reaction
Blood Typing
When serum containing anti-A or anti-
B agglutinins is added to blood, agglutination will occur between the agglutinin and the corresponding agglutinogens
Positive reactions indicate agglutination
Prevention of Undesirable Clots
Substances used to prevent undesirable clots include:
Aspirin – an antiprostaglandin that inhibits thromboxane A
2
Heparin – an anticoagulant used clinically for pre- and postoperative cardiac care
Warfarin – used for those prone to atrial fibrillation
Hemostasis Disorders: Bleeding
Disorders
Thrombocytopenia – condition where the number of circulating platelets is deficient
Patients show petechiae (small purple blotches on the skin) due to spontaneous, widespread hemorrhage
Caused by suppression or destruction of bone marrow (e.g., malignancy, radiation)
Platelet counts less than 50,000/mm 3 is diagnostic for this condition
Treated with whole blood transfusions
Hemostasis Disorders: Bleeding
Disorders
Hemophilias – hereditary bleeding disorders caused by lack of clotting factors
Hemophilia A – most common type (83% of all cases) due to a deficiency of factor VIII
Hemophilia B – results from a deficiency of factor IX
Hemophilia C – mild type, caused by a deficiency of factor XI
Hemostasis Disorders
Disseminated Intravascular Coagulation
(DIC): widespread clotting in intact blood vessels
Residual blood cannot clot
Blockage of blood flow and severe bleeding follows
Most common as:
A complication of pregnancy
A result of septicemia or incompatible blood transfusions
RBC formation animation
Blood clotting animation
Fun Facts
•There are almost 60,000 miles of blood vessels in the human body.
•Red blood cells are formed at the rate of 2 million per second.
•Within a tiny droplet of blood, there are 5 million red blood cells, 300,000 platelets and 10,000 white cells.
•It takes about 1 minute for a red blood cell to circle the whole body.