AOA Cardiology Review
advertisement

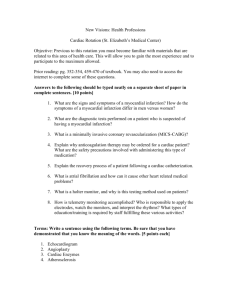
AOA Cardiology Review Part 1: Myocardial Infarction Objectives • Work through a typical cardiac patient case presentation • Review acute myocardial infarction from risk factors, symptoms, diagnosis, treatment, and complications • Understand mechanism of major drugs used to treat HTN and MI Case presentation • A 62yo Caucasian Male presents in the ED with the chief complaint of chest pain and difficulty breathing • What more do you want to know? Symptoms • Patient describes a sensation of “crushing heaviness” at his sternum “like an elephant is sitting on my chest” 10/10 • It has been going on for the last half hour and started after dinner • He has had this sensation before but usually it occurred when he was mowing the lawn or raking leaves and always went away with rest and some Bayer Aspirin • Nothing seems to make it better or worse • The patient denies any nausea or vomiting • States that he feels a little sweaty and that he just can’t seem to catch his breath, however he admits that he may just be anxious and overly concerned as to what is causing his pain. • The patient also states that his left shoulder is a little sore but that may be due increased activity • He has also had a nonproductive cough for 3 days but no fevers, chills, or night sweats Medical History PMHx: The patient has struggled with obesity for most of his adult life. Five years ago he started watching what he eats after his doctor told him that his blood sugar was too high. He tries to remember to take his “water pill” and baby aspirin every day but admits that usually he is just too busy with work to remember to do so. FamHx: Mother died at age 72 of cancer Father had heart attack and age 43 but lived until the age of 78 One younger brother with COPD Older sister with diabetes Has two sons (42 and 37, both healthy as far as he knows) Social: lives at home with wife, works full time 20 pack year history of smoking, quit two years ago Drinks EtOH socially at holiday parties, no other drug use Medications: Baby ASA daily “Water pills” - thinks its HCTZ for some elevated blood pressures he had 4 years ago, have not been rechecked since Claritin for allergies Glucosaimine/Chondrioitin for joint pain Differential Diagnosis • • • • • • • Myocardial Infarction Angina Aortic Dissection GERD Pulmonary Embolism, Pneumonia Muscle Strain, Costochondritis Panic Attack, Anxiety What do You Want to do Now? • VS: HR: 156 BP: 164/98 RR: 35 O2: 98% • CXR: Clear lung fields, no cardiomegaly or pneumonia • Cardiac Enzymes: Troponin and CK-MB • EKG: ST elevations in V2, V3, and V4 • Sublingual nitroglycerin = minimal pain relief STEMI Alert!!!! • ED resident calls STEMI Alert and cath lab is notified for possible PTCA • Patient given morphine for pain and sublingual nitro 2 more times at five minute intervals • Cardiology is consulted and patient started on heparin, ASA, β-blocker, statin, and given sublingual nitrate for home use. Also started on ACEi for renal protection Ischemic Heart Disease Usually secondary to coronary artery disease (atherosclerosis) 1. Subintimal thickening causes occlusion of lumen 2. Early fatty streaks progress to plaque formation (LDL oxidization, foam cells, fibrous cap) 3. Any damage to the endothelial cell layer exposes the vessel to the coagulation cascade and further thrombus formation Myocardial oxygen consumption/demand depends on HR, BP and contractility When vessels of heart are diseased, they are maximally dilated in order to maintain adequate perfusion of the heart (cardiac myocytes maximally extract O2 from blood) Tachycardia increases O2 deliver to tissue, however also decreases time in diastole → less filling time, less perfusion time CAD Spectrum • Stable Angina – Predictable chest pain; usually brought on by exertion, psychological stress, cold weather, or heavy meals; relieved by rest and sublingual nitro. Usually < 10min. No changes on EKG or elevation of cardiac enzymes. • Unstable Angina – new onset, changing in severity, frequency or duration, 10-20 min, occurring at rest. No EKG changes or elevation of cardiac enzymes • Non STEMI – Subendothelial infarct • STEMI – Transmural infarct (Prinzmetal’s Angina – transient coronary vasospasm occurring at rest, transient ST elevation but negative cardiac enzymes, Tx with CCB’s or nitrates) Risk Factors for CAD and MI • Diabetes – tight glycemic control DOES NOT prevent macrovascular complications • • • • Hypertension – BP> 140/90 x3 Smoking - #1 preventable risk factor Hyperlipidemia – elevated LDL Family history – premature CAD in first-degree male relatives < 45 or female relatives < 55 • Metabolic Syndrome – waist circumference, triglycerides, HDL, BP, and fasting glucose Myocardial Infarction Demographics • Leading cause of Symptoms: Chest “pain” – pressure, tightness, squeezing, heaviness, burning May radiate to neck, jaw, shoulder, arms Associated with N/V, diaphoresis, cough, dizziness, SOB, Levine Sign, anxiety • • • • morbidity and mortality in USA 1.3 million nonfatal MI/yr 0.5-0.7 million fatalities/yr Male predilection, ages 40-70 Elderly patients and diabetics may not present with typical findings Pathology of Acute MI • Myocytes begin to die within 20-40 minutes of ischemia • 1st 24hrs: coagulative necrosis begins, contraction bands form, loss of cross striations and nuclei within myocyte * Death is due to fatal arrhythmias • 2-4 days: Acute inflammation, neutrophil emigration secondary to release of inflammatory cytokines from necrotic myocytes, increased coagulative necrosis • 5-10 days: Grossly, the area of infarct has a hyperemic border with central yellow/brown softening, ingrowth of granulation tissue, macrophages are present, fibroblasts begin laying down scar * Death due to myocardial rupture → cardiac tamponade • 7 weeks: hypertrophic cardiac myocytes are present adjacten to scar (collagen), collagen is weaker than surrounding heart tissue, contractions pull on collagen increasing risk for aneurysm formation Treatment for acute MI • Nitrates – ↓ preload thus ↓ demand, dilates coronary arteries, reduces chest pain • Oxygen – decreases area of ischemic injury • Morphine - ↓ pain, thus may decrease tachycardia and O2 demand, also ↓ preload • Heparin – prevents progression of thrombus, does NOT ↓ mortality (CI’s do exist) • Revascularization – Consider thrombolysis or Percutaneous Transluminal Coronary Angioplasty Prolonged Treatment for MI • ASA - ↓ mortality, reduces risk for reocclusion by preventing platelet aggregation • Β-blocker – reduces HR, contractility and afterload thus reducing myocardial O2 demand, ↓ mortality • ACEi - ↓ mortality, use if no contraindications • Statins - ↓ risk of further coronary events • Cardiac Rehabilitation/ Lifestyle Modifications Complications of MI • Arrhythmia: • Recurrent MI • LV failure → pulmonary edema, (S3, S4, pulmonary rales) → right heart failure • Cardiogenic Shock: hypotension, tachycardia, hypoxia, JVD, ↓CO, ↑ PCWP • Aneurysm: can ↓ CO, cause, arrhythmias, mural thrombus formation, rupture (especially • Rupture: free wall, interventricular septum, papillary muscle • Early Fibrinous pericarditis: pain worse when lying done or with deep inspiration, • Dressler’s Syndrome – autoimmune fibrinous pericarditis most common cause of pre-hospital death in MI, Right Coronary artery supplies SA and AV node, PVC, PSVT, Vtach, Vfib, sinus tach, sinus brady, asystole can all occur = treat appropriately pseudoaneurysms) better with leaning forward • • • • • • Cardiac Tamponade Life threatening complication of MI, aortic dissection, trauma, etc Bleeding into pericardial sac → equalization of pressures in all four chambers → diastolic dysfunction Triad of JVD, muffled heart sounds, and hypotension Pulsus paradoxus – exaggerated decrease in arterial pressure with inspiration >10mmHg Electrical alternans on EKG Treatment depends on cause – pericardiocentesis vs. emergent surgery Hypertension • BP > 140/90 x3 separate occasions • 95% essential/primary HTN • 5% secondary (Endo, Renal, Meds/Drugs, Iatrogenic) • Malignant HTN: rapidly progressive, young AA males, causes markedly ↑ DBP, malignany nephrosclerosis/flea-bitten kidneys, focal retinal hemorrhages, papilledema • Hypertensive urgency: BP> 200/110 but no end organ damage • Hypertensive Emergency: with end-organ damage such as encephalopathy, renal failure, CHF Tx: IV labetalol or nitroprusside, decrease BP slowly to decrease risk of stroke HTN Treatment • Lifestyle Modifications (exercise, diet) • Consider Comorbidities when choosing a medication • Often using more than 1 medicine, a thiazide diuretic should be part of treatment regimen if not contraindicated to provide synergy Thiazides • Decrease sodium reabsorption via Na/Cl channel in distal loop of Henle thus decrease fluid retention - SE: HyperGLUC (glycemia, lipidemia, uremia, and calcemia) hypokalemia - Avoid in diabetics, gout - Good for patients with osteoporosis • Loop Diuretics – effective diuretic but do not do much to lower BP unless etiology is volume overload ACE Inhibitors • ↓ angiotensin converting enzyme to ↓vasoconstriction, catecholamine release, sodium reabsorption, and fluid retention - Renoprotective = use in diabetics - Avoid use in patients who already have renal failure because ACEi can increase CR and K+ - SE: cough (bradykinin), angioedema, teratogenic (consider switching to ARB if having these symptoms) * Proven to decrease MORTALITY post MI! Calcium Channel Blockers • Decrease contractility, decrease afterload via arteriodilation - Dihydropyridines: Nifedipine ↓ afterload, less effect on heart itself, can cause reflex tachycardia so use with a β-blocker to prevent especially post MI - Non-dihydropyridines: Verapamil, Diltiazem Class IV antiarrhytmics, act on cardiac myocytes to decrease contractility SE: Cardiac depression, peripheral edema, constipation, prolongation of PR interval → torsades de pointes β-blockers • Metoprolol, Atenolol, Esmolol Cardioselective = β1 only, ↓ CO, ↓ HR, ↓ MVO2 • Propanolol, Timolol, Labetalol Noncardioselective = avoid use in patients with COPD or asthma due to risk of bronchoconstriction Propanolol may prevent reinfarct and SCD • Useful in HTN, Angina, SVT, CHF • Proven to ↓ MORTALITY Post MI! Reduces risk of SCD! • SE: impotence, bronchoconstriction, bradycardia, AV block, sedation, mask symptoms of hypoglycemia Others • Hydralazine – reduces afterload by unknown mechanism, does not affect heart so results in reflex tachycardia (use with β-blocker) • Minoxidil – reserved for severe, refractory HTN, side effects include hypertrichosis, pericardial effusion, and reflex tachycardia (use with β-blocker and diuretic) Side Notes • Heart Attacks in KIDS?!?! • Rare (0.2/100,000) • Usually associated with: 1. Kawasaki’s Disease 2. HOCM 3. Congenital anomaly • “Holiday Heart” • EtOH cardiomyopathies and arrhythmias associated with weekend alcohol and drug use Take Home Points • HTN and MI are common things seen by physicians, therefore it is likely that you will see them on the USMLE Step 1 • Learn key facts about the medicines such as odd side effects, these will help you save time on the test • Most often, the CXR, other imaging, or EKG help you confirm your answer, usually you can AOA Cardiology Review Part 2: Cardiomyopathies Dilated Cardiomyopathy • Most common • Four chambered dilation and hypertrophy • Systolic dysfunction (poor contractility) • Poor prognosis: death within 5 years of symptom onset Etiology 1. CAD with prior MI 2. Toxic: EtOH, doxorubicin, adriamycin 3. Infectious: Coxsackie B, Chagas’ disease, Lyme disease, HIV 4. Metabolic: beriberi, uremia, genetic storage diseases 5. Thyroid Disease 6. Pregnancy 7. Rheum: SLE, scleroderma 8. Idiopathic: 50% of cases Dilated Cardiomyopathy Diagnosis 1. Signs and symptoms of Left and Right CHF 2. Arrhythmias 3. S3, S4, AV valve insufficiency 4. EKG, ECHO, CXR consistent with heart failure Treatment • Digoxin, diuretics, β-blockers, heart transplant • Discontinue offending agent if possible • Anticoagulation due to ↑ risk of embolization • ICD if Vtach or Vfib Hypertrophic Cardiomyopathy Symptoms/Signs 1. 2. 3. 4. • Autosomal dominant missense mutation in 1 of 10 genes that encode for protein of the sarcomere • Cardiac Myocyte disarray • Diastolic dysfunction due to poor left ventricle relaxation • May have dynamic outflow obstruction with asymmetric hypertrophy of IVS 5. DOE, syncope Angina, Palpitations, Arrhythmias Sudden Cardiac Death Loud S4, strong apical impulse, systolic ejection murmur, no click (valve not involved) Murmur decreases with increased preload or afterload, decreased contractility; increases with Valsalva and standing Hypertrophic Cardiomyopathy Diagnosis • Family history • ECHO • Myocardial biopsy diagnostic Treatment • Avoid strenuous exercise • Β-blockers, CCB if symptomatic • Myomectomy has high success rate for relieving symptoms • ICD to prevent SCD • 5% annual mortality due to SCD Restrictive Cardiomyopathy • Infiltration of myocardium • Impaired diastolic function due to decreased ventricular compliance • Systolic dysfunction in advanced disease due to impaired contractility Etiology 1. Amyloidosis 2. Sarcoidosis 3. Hemochromatosis 4. Scleroderma 5. Carcinoid Syndrome 6. Idiopathic Restrictive Cardiomyopathy Diagnosis 1. ECHO: thickened myocardium 2. Increased RA, LA with normal LV, and RV size 3. Bright, sparkled myocardium in amyloidosis 4. EKG: low voltage 5. Endomyocardial biopsy 6. Can mimic constrictive pericarditis Treatment 1. Treat underlying disorder 2. Digoxin if systolic dysfunction present Questions? hwasserm@neoucom.edu THANK YOU!