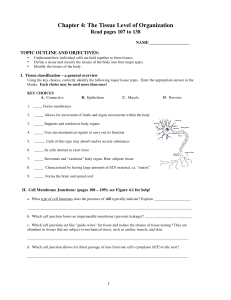
CHAPTER 5: TISSUES - Ashland Independent Schools
advertisement

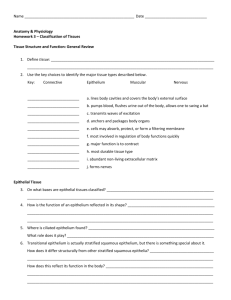
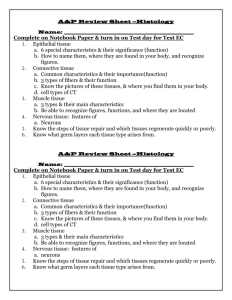
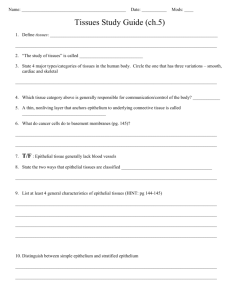
The Tissue Level Of Organization BIO 137: Anatomy & Physiology I Tissues • Tissues are a group of cells with a common embryonic origin that function together to carry out specialized activities. – They include various types, ranging from hard (bone) to semisolid (fat) to liquid (blood). Intercellular Junctions • Tissues are formed by grouping cells together using a variety of Intercellular Junctions . – Intracellular Junctions connect adjacent cells mechanically at the cell membranes or through cytoskeletal elements within and between cells. Intercellular Junctions • Tight Junctions are found where a leakproof seal is needed between cells. – They keep materials from leaking out of organs like the stomach and bladder. Intercellular Junctions • Adherens Junctions make an adhesion belt (like the belt on your pants) that keeps tissues from separating as they stretch and contract. • Cadherin is a glycoprotein that forms the belt-like “plaque”. Intercellular Junctions • Desmosomes act as “spot welds”. They also use cadherin glycoprotein (plus intermediate filaments) to hook into the cytoplasm. Intercellular Junctions • Hemidesmosomes are half-welds that join cells to the basement membrane. Intercellular Junctions • Gap Junctions are pores (connexons) that allow small substances like ions to pass between cells. If one of the cells gets sick or dies, these seal like a hatch to prevent damage to other cells. The 4 Basic Tissues • Of all the cells in the body, they combine to make only 4 basic tissue types: – Epithelial tissues – Connective tissues – Muscular tissues – Nervous tissues Epithelial Characteristics Cover body surfaces, form glands, line hollow organs, body cavities and ducts. • Tightly packed sheets of cells w/ little intercellular material • All epithelia have a free surface that faces an opening and an attached basal surface – Basement membrane • May possess cilia or microvilli on free surface • Avascular • Readily divide Epithelial Locations & Functions • Epidermis • Protection • Covers ventral body organs (serous membranes) • Absorption • Lines body cavities (parietal membranes) • Excretion • Lines exocrine glands • Lines hollow organs • Lines capillaries • Secretion • Filtration • Diffusion Classification of Epithelium • Number of Layers • Simple • Stratified • Pseudostratified • Shape of Cells • Squamous • Cuboidal • Columnar Epithelium Classification Epithelium Studied in BIO 137 • Simple Squamous ET (lung alveoli) • Simple Cuboidal ET (thyroid gland) • Simple Columnar ET (duodenum) • Pseudostratified Columnar ET (trachea) • Stratified Squamous ET (skin) • Transitional ET (ureter) • Glandular ET (not studied in lab) Simple Squamous Epithelium A single layer of thin, flattened cells • Locations: – – – – *Lining air sacs (alveoli) Lining capillaries Kidney glomeruli Lining vessels • Functions: – Diffusion (exchange of gases, nutrients, wastes) – Filtration Simple Squamous Epithelium (a) Simple squamous epithelium Description: Single layer of flattened cells with disc-shaped central nuclei and sparse cytoplasm; the simplest of the epithelia. Function: Allows passage of materials by diffusion and filtration in sites where protection is not important; secretes lubricating substances in serosae. Location: Kidney glomeruli; air sacs of lungs; lining of heart, blood vessels, and lymphatic vessels; lining of ventral body cavity (serosae). Air sacs of lung tissue Nuclei of squamous epithelial cells Photomicrograph: Simple squamous epithelium forming part of the alveolar (air sac) walls (400x). Simple Cuboidal Epithelium • A single layer of cube-shaped cells with large prominent nuclei • Locations: – Lining kidney tubules – Lining the ducts of exocrine and endocrine glands • Functions: – Secretion (exocrine and endocrine glands) – Secretion and Reabsorption (kidney tubules) Simple Cuboidal Epithelium (b) Simple cuboidal epithelium Description: Single layer of cubelike cells with large, spherical central nuclei. Simple cuboidal epithelial cells Function: Secretion and absorption. Location: Kidney tubules; ducts and secretory portions of small glands; ovary surface. Basement membrane Connective tissue Photomicrograph: Simple cuboidal epithelium in kidney tubules (400x). Simple Columnar Epithelium • A single layer of column like cells, with nuclei located near the basement membrane • Other structures of interest: – Goblet cells - mucus – Microvilli – increase surface area for absorption – May be ciliated • Location: Intestinal lining (Villi), uterus • Functions: – Protection – Absorption – Secretion Intestinal Villi: Simple Columnar Epithelium GOBLET CELL Ciliated Pseudostratified Columnar Epithelium • A single layer of elongated cells – Nuclei dispersed throughout the cytoplasm (appears to have layers) • Other structures of interest: – Cilia – Goblet cells • Location: Lining of trachea • Functions: – Secretion – Protection Ciliated Pseudostratified Columnar Epithelium GOBLET CELL CILIA Epithelium • Stratified Squamous Epithelium has an apical surface that is made up of squamous (flat) cells. – The other layers have different shapes, but the name is based on the apical layer. – The many layers are ideal for protection against strong friction forces. Transitional Epithelium • Multilayered cells that change shape due to changes in pressure in the tissue • Locations: – Lining of Urinary bladder – Lining of Ureter • Function: – Distensibility TRANSITIONAL ET: URETER ~LOW POWER~ TRANSITIONAL ET SMOOTH MUSCLE Copyright 2006 Dr. Mary Cat Flath Epithelium • Although epithelia are found throughout the body, certain ones are associated with specific body locations. Connective Tissue • Includes bones, adipose, blood, cartilage and other connective tissues • Functions: support, framework for attachment, hematopoiesis, energy stores, protection Connective Tissue • Connective Tissues are the most abundant and widely distributed tissues in the body • Sparse cells separated by intercellular material called matrix • Can usually divide Connective Tissues • Collagen is the main protein of C.T. and the most abundant protein in the body, making up about 25% of total protein content. • Connective tissue is usually highly vascular and supplied with many nerves. – The exception is cartilage and tendon - both have little or no blood supply and no nerves. Connective Tissue Matrix • Found between cells, secreted by immature blast cells • 2 components of matrix – Protein Fibers – 3 types of fibers • Secreted by fibroblasts • Fiber types vary among CT – Ground substance – fluid, semi-fluid, gelatinous or calcified • Material in CT that provides a media for movement of nutrients and gases & binds CT components together Connective Tissue Fibers • Collagen – Give a tissue High tensile strength and resists pulling – Found in ligaments and tendons • Elastic Fibers – Composed of elastin protein – Give a tissue Elasticity – Fibers are easily stretched and reformed – Found in Vocal cords, external ear and air passages • Reticular Fibers – Composed of collagen fibers called reticulin – Found in basement membrane, also support capillaries and nerve fibers Cell Types Found in CT • Fibroblasts – Most abundant, produce fibers of matrix • White Blood Cells – Macrophages phagocytosis – Mast Cells - Release heparin and histamine for Tissue repair and healing • Chondrocytes - cartilages • Osteocytes – bone Connective Tissue Classification • Embryonic connective tissue – Mesenchyme – Mucous connective tissue • Mature connective tissue – Loose connective tissue – Dense connective tissue – Cartilage – Bone – Liquid Embryonic Connective Tissues • There are 2 Embryonic Connective Tissues: – Mesenchyme gives rise to all other connective tissues. – Mucous C.T. (Wharton's Jelly) is a gelatinous substance within the umbilical cord and is a rich source of stem cells. CT Studied in Bio 137 • • • • • • • Loose Areolar CT Adipose Tissue Dense Regular CT (White fibrous CT) Hyaline Cartilage Elastic Cartilage Blood Bone Loose Areolar Connective Tissue • The most widely distributed in the body. • Contains several types of cells and all three fiber types. • Location: papillary layer of dermis, Component of basement membrane, Between muscles, between other tissues • Functions: – Diffusion & Cushioning – Binds skin to underlying tissues Loose Areolar Connective Tissue Loose Areolar Connective Tissue (a) Connective tissue proper: loose connective tissue, areolar Photomicrograph: Areolar connective tissue, a soft packaging tissue of the body (400x). Adipose Tissue • Cells: Adipocytes filled with fat globules • Locations: – Subcutaneous layer – Around organs and joints • Functions: – – – – Energy Store Protection Cushion Insulation Adipose Tissue Mature Connective Tissues • Dense Connective Tissues – Dense Irregular Connective Tissue consists predominantly of fibroblasts and collagen fibers randomly arranged. • It provides strength when forces are pulling from many different directions. – Dense regular – Elastic Dense Regular Connective Tissue • Matrix of tightly packed collagen fibers with few fibroblasts • Lacks a direct blood supply • Locations: – Tendons Ligaments • Functions: – Attachment/ High tensile strength Dense Regular Connective Tissue Cartilage • Rigid connective tissue with a poor direct blood supply • Abundant collagen and/or elastic fibers in gellike ground substance • Primary cell is chondrocyte • Do not divide often • Classified by type of matrix Hyaline Cartilage • Most abundant type of cartilage in the body • Locations: – Wall of trachea and larynx – Nose – Embryonic Skeleton – Costal cartilages – Ends of long bones • Function: Support and protection Hyaline Cartilage Fibrocartilage • Thick bundles of collagen fibers • A very strong, tough cartilage. • Locations: – Intervertebral spaces – Knee joints • Support Elastic Cartilage • Chondrocytes surrounded by matrix filled with elastic fibers • Locations: – Auricle or Pinna of External Ear – Epiglottis • Function: – Flexibility with maintenance of shape Elastic Cartilage (g) Cartilage: elastic Note the presence of elastic fibers Photomicrograph: Elastic cartilage from the human ear pinna; forms the flexible skeleton of the ear (640x). Blood • The only liquid connective tissue • Blood cells (Erythrocytes, leukocytes, and thrombocytes) in a liquid matrix of plasma • Location: – Heart and blood vessels • Function: – Transport of gases, nutrients and wastes Compact Bone • Osteocytes surrounded by a solid matrix of calcium phosphate and collagen • Location: skeleton • Functions: – Support – Protection – Movement – Hematopoiesis – Calcium (mineral) Store Figure 4.9i: Connective tissues (continued), pp. 137-138. (i) Others: bone (osseous tissue) Description: Hard, calcified matrix containing many collagen fibers; osteocytes lie in lacunae. Very well vascularized Function: Bone supports and protects (by enclosing); provides levers for the muscles to act on; stores calcium and other minerals and fat; marrow inside bones is the site for blood cell formation (hematopoiesis). Location: Bones Central canal Lacunae Lamella Photomicrograph: Cross-sectional view of bone (70x). Summary of Mature Connective Tissues Muscle Tissues • Long, thin fibers that shorten and contract to allow movement • Three types: – Skeletal muscle – Smooth muscle – Cardiac muscle • Will be studied in greater detail during the muscular and cardiovascular systems Muscle Tissue Nervous Tissue • Neurons (nerve cells) with multiple extensions surrounded by neuroglial cells • Locations: – Brain and spinal cord (CNS) – Nerves (PNS) • No reproduction of cells • Function: – Integration and coordination of all body parts Nervous Tissue Epithelial Membranes • A layer of epithelium that lies over a layer of connective tissue • Three types of epithelial membranes: – Serous Membranes – Mucous Membranes – Cutaneous Membranes Serous Membranes • Thoracic and Abdominopelvic Membranes – Line the walls of body cavities and fold back to cover the organs – Secrete serous fluid for lubrication • Visceral layer – covers an organ • Parietal layer – lines a cavity or body wall Serous Membranes • Thoracic Membranes: Lungs – Visceral Pleura – Parietal Pleura • Thoracic Membranes: Heart – Visceral Pericardium – Parietal Pericardium • Abdominopelvic Membranes – Visceral Peritoneum – Parietal Peritoneum Mucous Membranes • Mucous membranes line interior body surfaces open to the outside – Digestive tract lining – Respiratory Tract – Reproductive Tract • Functions: – Protection – Lubrication Cutaneous Membrane • Location: Skin • Function: – Protection • Will be studied further in Chapter 5 Glandular Epithelium • Composed of cells specialized that produce & secrete substances into ducts or body fluids • Usually simple cuboidal or simple columnar ET • Function: Secretion • Include exocrine and endocrine glands Exocrine Glands • Exocrine glands secrete substances through ducts to the surface of the skin or into the lumen of a hollow organ. • Secretions of the exocrine gland include mucus, sweat, oil, earwax, saliva, and digestive enzymes. Exocrine Glands • Merocrine secretion is the most common manner of secretion. – The gland releases its product by exocytosis and no part of the gland is lost or damaged . – Salivary gland Exocrine Glands • Apocrine glands “bud” their secretions off through the plasma membrane, producing membrane-bound vesicles in the lumen of the gland. – The end of the cell breaks off by “decapitation”, leaving a milky, viscous odorless fluid. – Mammary gland Exocrine Glands • Holocrine secretions are produced by rupture of the plasma membrane, releasing the entire cellular contents into the lumen and killing the cell (cells are replaced by rapid division of stem cells.) – Sebaceous gland Aging and Tissues • Tissue heals faster in young adults. • Surgery of a fetus normally leaves no scars. • Young tissues have a better nutritional state, blood supply, and higher metabolic rate. • Extracellular components also change with age. • Changes in the body’s use of glucose, collagen, and elastic fibers contribute to the aging process.