Level I - Rackcdn.com
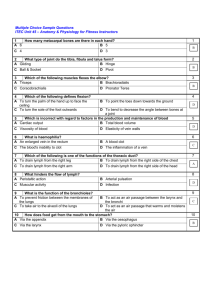
advertisement

The Nuts and Bolts of Head and Neck Tumor Evaluation Colin McKnight, Kelly Malloy, Amanda Corey, Ashok Srinivasan Presentation Number: eEdE-126 Disclosures NONE Purpose To review the key imaging features that are crucial to patient management as discussed in head and neck tumor boards. Approach Various teaching points are critical to the radiologist’s ability to provide useful and relevant insight into the pertinent imaging findings in a head and neck tumor board case. Topics covered include: -Lymph nodal stations in the neck -Accepted ranges for normal size in neck lymph nodes at different levels -When is a lymph node morphologically abnormal? -Where to look for the ‘unknown primary’ -What are ‘orphan’ lymph nodes? -How is carotid artery encasement determined? -Importance of TNM staging Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations Level I: All nodes above the hyoid bone, below the mylohyoid muscle, and anterior to a line drawn through the posterior edge of the submandibular gland. Level IA: Lie between the medial margins of the anterior bellies of the digastric muscles. Level IB: Lie posterior and lateral to the medial edge of the anterior belly of the digastric muscle, and anterior to a line drawn between the posterior surface of the submandibular glands. IA I I II II V V IB Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations Level II: Lie from the skull base, at the lower level of the bony margin of the jugular fossa, to the level of the lower body of the hyoid bone. Level II nodes lie anterior to a line drawn through the posterior edge of the sternocleidomastoid muscle and posterior to a line through the posterior edge of the submandibular gland. Level IIA: Lie anterior, lateral, or medial to the jugular vein; or lie posterior to the internal jugular vein and are inseparable from the vein. Level IIB: Lie posterior to the internal jugular vein and have a fat plane separating the nodes and the vein. I I II II V V IIA IIB Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations Level III: Lie between the level of the lower body of the hyoid bone and the lower margin of the cricoid cartilage arch, anterior to the posterior edge of the sternocleidomastoid muscle and lateral to the common/internal carotid artery. II VI III III IV V Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations Level IV: Lie between the level of the lower margin of the cricoid cartilage arch and the level of the clavicle. These are located anterior to the posterior edge of the stenocleidomastoid muscle and the posterolateral edge of the anterior scalene muscle and are located lateral to the common carotid artery. II VI IV III IV V Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations VI Level V: Extend from the skull base to the level of the clavicle. III Level VA: Lie between the levels of the skull base and the bottom of the cricoid arch. These nodes are situated posterior to a transverse line drawn on each axial scan through the posterior edge of the sternocleidomastoid muscle. Level VB: Lie between the axial level of the bottom of the cricoid arch and the level of the clavicle. Level VB nodes lie posterior and lateral to an oblique line through the posterior edge of the sternocleidomastoid muscle and the posterolateral edge of the anterior scalene muscle. V VI IV V Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations VI IV VI III V V Level VI: Lie inferior to the lower body of the hyoid bone, superior to the top of the manubrium, and between the medial margins of the left and right common carotid arteries or the internal carotid arteries. Discussion Lymph nodal stations in the neck: How to divide the neck into different lymph nodal stations VII Level VII: Lie caudal to the top of the manubrium in the superior mediastinum, between the medial margins of the left and right common carotid arteries. These nodes extend caudally to the level of the innominate vein. Discussion Accepted ranges for normal size in neck lymph nodes at different levels: -Nodal size criteria can be used when nodes are homogenous and clearly delineated. -Upper limit for short axis is 11 mm for jugulodigastric lymph nodes and 10 mm for all other nodes. -Upper limit for greatest nodal diameter is 1.5 cm for jugulodigastric, submandibular and submental nodes, and 1 cm for all other nodes. -Retropharyngeal node <8mm AJR 1992 158(5):961-969 Discussion Accepted ranges for normal size in neck lymph nodes at different levels: There is an error rate of ≈ 10 - 20% if using size criteria alone. The long to short axis ratio has also been proposed to help evaluate enlarged nodes in the setting of head and neck SCC. When nodes have a ratio of >2 (ie long and flat) 95% are benign. When the ratio is less than 2 (i.e. rounder) then a similar proportion where malignant. AJR 1992 158(5):961-969 Discussion When is a lymph node morphologically abnormal? Rounded Low density or cystic (long-short axis ratio <2) (internal low attenuation without thick rim) Discussion When is a lymph node morphologically abnormal? Necrotic Internal low T1 signal with peripheral thick rim of enhancement Extracapsular spread Pericapsular infiltration implies worse prognosis Calcified E.g., papillary thyroid cancer metastases, tuberculosis Discussion Where to look for the ‘Unknown Primary’: Metastatic lymph node Where is the primary tumor? Discussion Where to look for the ‘Unknown Primary’: Look at: 1. Nasopharynx 2. Oropharynx – (Base of tongue/palatine tonsil) 3. Supraglottic larynx 4. Pyriform sinus 5. Thyroid gland Occasionally none is seen on CT. Next step… PET CT Primary SCC in palatine tonsillar fossa Discussion What are ‘Orphan’ Lymph Nodes? Lymph nodes in the face and retropharyngeal region that do not fit into the nodal stations from I-VII With permission from Radiology 1993; 188(3):695-700. Discussion Zygomatic group lymph nodes: T2 Recurrent SCC in right cheek T1 Post Discussion Parotid space mass. Where are the nodes? While the retropharyngeal lymph node is apparent on the T2W image, it is easier to appreciate on the diffusion image Discussion One more: Zygomatic lymph node Discussion -Do not forget retropharyngeal lymph nodes. -These are probably the most commonly missed lymph nodes in the neck -Look for asymmetry, as well as displacement of the carotid artery Discussion How is carotid encasement determined? 0 Shows 360 involvement suggestive of encasement -Determined by calculating degree of circumferential contact around the carotid artery by tumor >270 degrees considered threshold for encasement - Makes the tumor inoperable Increases risk of carotid blowout Discussion Importance of TNM staging: 1. Dictates prognosis 2. Treatment is based on staging T1 – T2: Single modality: surgery vs radiation therapy T3 – T4: Combination of both T4: Can be locally advanced, may not do surgery Discussion Importance of TNM staging: Laryngeal Cancer: Discussion Importance of TNM staging: Laryngeal Cancer: -Invades paraglottic fat -Was clinically staged as T2 -Upstaged to T3 based on CT Normal Effaced paraglottic fat paraglottic fat Discussion Importance of TNM staging: Subglottic involvement -Lesion involves supraglottis, glottis, subglottis -Lesion is transglottic -While this remains T3, the surgical approach is changed Discussion Nasopharyngeal cancer staging: Discussion Nasopharyngeal cancer staging: -Invasion of the medial pterygoid: Upstaged to T4 based on imaging -Also, there is an involved retropharyngeal lymph node -Skull base invasion, if present, would reflect T3 disease Discussion Nasopharyngeal cancer staging: -Invasion of longus colli muscle: While not in TNM staging, implies worse prognosis -Intracranial extension would qualify as T4 disease Discussion Squamous cell cancer staging: Invasion of the genioglossus and hyoglossus: Extrinsic tongue muscle invasion is T4 disease MRI Confirms invasion Discussion Squamous cell cancer staging: Another patient with invasion of posterior genioglossus indicating T4 disease; the normal muscle on the left is depicted as well Discussion Squamous cell cancer staging: Normal fat plane of separation Patient with pyriform sinus cancer shows loss of fat planes on CT with the prevertebral muscle. If truly involved, this would be T4 disease. MRI is a better modality for making this assessment and shows no convincing extension into the muscles. At surgery, the muscle was free from tumor. Discussion Remember Perineural Spread Right Parotid acinic cell CA with perineural spread along the facial nerve involving multiple segments. The genu of the facial nerve …And the IAC Note anterior spread from genu to involve the greater superfical petrosal nerve that reached up to the pterygopalatine fossa and also retrogradely involve the maxillary N. Discussion Utility of fat suppression imaging: Separating fatty atrophy from tumor Increased conspicuity of primary tumor borders after contrast administration “Revealing” small lesions including perineural spread surrounded by fat Discussion Fatty denervation versus tumor Fat sat imaging helpful because fat is abundant in the neck. Fat sat imaging reveals fatty denervation in the right tongue from hypoglossal nerve palsy. Clinically diagnosed as bulky tongue lesion Discussion T1 + Without Fat saturation T1 + With Fat saturation Right neck SCC Perineural spread along V3 nerve is seen much more conspicuously with fat saturation (Sometimes subtle enhancement such as this can be seen only after fat saturation) Summary Knowing the imaging pearls and pitfalls in head and neck tumors is crucial to making a difference to patient management Contact: cmcknig@med.umich.edu Bibliography 1. Som PM, Curtin HD, Mancuso AA. Imaging-based nodal classification for evaluation of neck metastatic adenopathy. AJR 2000; 174(3):837-844. 2. Som PM. Detection of metastasis in cervical lymph nodes: CT and MRI criteria and differential diagnosis. AJR 1992; 158(5):961-969. 3. Tart RP, Mukherji SK, Avio AJ, Stringer SP, Mancuso AA. Facial lymph nodes: normal and abnormal CT appearance. Radiology 1993; 188(3):695700.